Increased intra-abdominal pressure (IAP) is an adverse complication seen in a number of critically-ill and post-operative children. Intra-abdominal hypertension (IAH) and abdominal compartment syndrome (ACS) occur as a result of elevated IAP. Elevated IAPs have a detrimental effect on the functions of several organs in the body and may lead to organ failure and death [1,2]. However, there is still not much experience of measuring IAP in the paediatric age group and it is not standard practice in most PICUs [3]. This study was done to determine the feasibility of measuring intra-abdominal pressures in critically-ill children using simple inexpensive equipment available in most PICUs.
Materials and Methods
This study was done over a three month period in the paediatric intensive care unit (PICU) of the Lokmanya Tilak Municipal General Hospital, a tertiary-care medical college hospital in Mumbai. The PICU admits critically-ill children with medical problems. Paediatric patients with trauma and surgical conditions are admitted elsewhere. Consecutive patients admitted to the PICU for more than 24 h and requiring a urinary catheter were included after obtaining written informed consent from the parent or guardian.
The study was started after approval from the institutional ethics committee.
Parameters noted were demographic data and risk factors for elevated intra-abdominal pressure including mechanical ventilation, use of pressors, requirement for fluid resuscitation, renal replacement therapy and presence of abdominal distension or ascites.
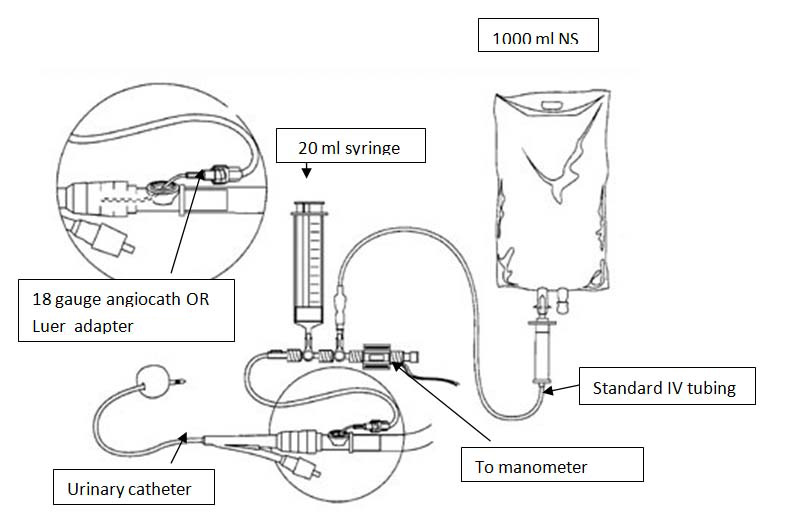
The intra-abdominal pressure was measured twice a day via a urinary catheter [Table/Fig-1]. The urinary catheter was connected to a 3-way stopcock. One end of the stopcock was connected to the urine bag and the other to a manometer (a disposable manometer used routinely for measurement of cerebrospinal fluid pressures was used). Sterile normal saline 1ml/kg (maximum 25 ml) was instilled into the bladder to ensure a continuous column of fluid. The measurement of intra-abdominal pressure was done after 60 sec of instillation of fluid to allow for equilibration. The zero reference point was the mid-axillary line at the iliac crest. IAP was measured twice a day for seven days or till discharge from the PICU or death. Pressure was measured in cm of water and converted to mm of Hg. The IAP values obtained in each patient were averaged and recorded. The course of the patient during the PICU stay as well as outcome in terms of survival or death was recorded.
Diagrammatic illustration for method for intra-vesical pressure monitoring
Results
Thirty-two patients were studied. Though patient diagnoses varied widely the most common were CNS disease, sepsis and tetanus (n = 9, 6 and 6 respectively).
The mean IAP in the different age groups is shown in [Table/Fig-2] and varied between 4.19 to 4.5 mmHg. [Table/Fig-3] shows the mean IAP in the different conditions. The mean IAP was highest in the miscellaneous group. This group included one patient with scorpion bite and four patients with dengue shock syndrome. The lowest mean IAP was seen in patients with tetanus. [Table/Fig-4] shows the association of IAP with risk factors. Patients with no risk factors had the lowest mean IAP.
Mean IAP in the various age groups
| Age | Number of patients | Mean IAP (mm Hg) ±S.D. |
|---|
| < 1year | 3 | 4.30±3.10 |
| Years | 17 | 4.50±2.90 |
| >5 years | 12 | 4.19±2.12 |
Mean IAP in the various conditions
| System | Mean IAP (mm Hg) ±S.D. |
|---|
| Renal | 6.75±3.75 |
| Sepsis | 6.06±2.50 |
| Respiratory | 5.40±2.00 |
| Metabolic | 4.90±1.82 |
| CNS | 4.70±2.10 |
| Tetanus | 2.09±1.30 |
| Miscellaneous | 8.16±4.04 |
Mean IAP and various risk factors
| Risk factors | Mean IAP (mmHg) ±S.D. |
|---|
| Fluid resuscitation, pressor support, and ventilation | 10.00±1.90 |
| Fluid resuscitation alone | 5.68±3.30 |
| No risk factors | 3.00±1.20 |
[Table/Fig-5] shows the range of intra-abdominal pressures in the patients and the outcome. All patients with a mean IAP >8mmHg died.
Range of intra-abdominal pressure and outcome
| Range of IAP | No of patients | Died |
|---|
| <5 mm Hg | 20 | 09 |
| 5-7 mm Hg | 04 | 02 |
| 8-11 mm Hg | 05 | 05 |
| 12-15 mmHg (grade 1) | 03 | 03 |
| Total | 32 | 18 |
Discussion
Twenty of thirty-two patients had a mean IAP < 5mmHg.Three patients had Grade 1 intra-abdominal hypertension (i.e. IAP >12 mmHg). All patients with a mean IAP >8mmHg died as compared with 11 of 24 patients with a mean IAP <8mmHg.
In our study the mean IAP across the different age groups was similar. There is limited data on the incidence of intra-abdominal hypertension in the paediatric age group. Ejike and co-workers studying intra-abdominal pressures in critically ill children found a mean IAP of 7±3 mm Hg in their patients. They found the mean IAP to be similar in different weight groups [3].
Patients with no risk factors and those with tetanus showed the lowest mean IAP. The abdominal wall compliance in patients with tetanus is low due to board-like rigidity of the abdomen and one would expect the mean IAP to be high [4]. The low mean IAP in these patients probably suggests that sedation and neuromuscular blockade in these patients was adequate.
Of the three patients with grade 1 IAH one was a case of acute pancreatitis. The patient was an 8-year-old girl admitted to the paediatric intensive care unit (PICU) with fever of three days duration and severe abdominal pain and anuria for one day. On admission, the patient was in shock and required fluid resuscitation and pressor support. Her mean IAP was 13 mm Hg. She was diagnosed to have acute pancreatitis and transferred to paediatric surgery. Following abdominal decompression urine output improved and renal function returned to normal over the next three days without dialysis. Studies have shown that IAH is a frequent finding in adults with severe pancreatitis. Pupeilis found a relationship of elevated intra-abdominal pressure and subsequent organ dysfunction in these patients [5]. De Waele et al., found the incidence of IAH in patients with severe acute pancreatitis to be as high as 51% [6].
The second patient with grade 1 IAH was a 4-year-old boy with septic shock who required fluid resuscitation, pressor support and ventilation. IAH is a common association with septic shock [7].
The third patient with grade 1 IAH was a 5-year-old girl with dengue shock syndrome. She had been anuric for 16 h and had deranged renal function and was transferred for management of renal failure. On admission her abdomen was found to be tense with guarding, rigidity and absent bowel sounds. Ultrasonography of the abdomen showed a large retroperitoneal hematoma. She was taken up for exploratory laparotomy after stabilization and platelet transfusions. Following surgery the urine output increased dramatically and renal function returned to normal. However the child died four days later due to a massive pulmonary hemorrhage due to decreasing platelet counts. Abdominal decompression resulted in normalization of renal dysfunction in our patient. Renal dysfunction in IAH is a multifactorial process and decreased cardiac output, altered renal blood flow and hormonal changes have been implicated as factors. Abdominal decompression seems to have a beneficial effect [8].
Eleven of 24 patients with a mean IAP < 5 mm Hg survived as compared to none of patients with an IAP of 8-11 mm Hg and grade 1 IAH, suggesting that increasing IAP is associated with increasing mortality. However, more extensive studies are required to determine whether there is a dose-dependent relationship. Grade 1 IAH was defined by adult values. All patients whose IAP was between 8-11 mm Hg also died.
More studies are required to determine intra-abdominal pressures in critically children. The values for defining intra-abdominal hypertension in children also need to be re-examined. Transducer sets with microprocessors are being increasingly used for measurement of IAP and may be better for continuous measurements. We used an inexpensive disposable manometer which is used routinely for measurement of cerebrospinal fluid pressures in our PICU. Lack of sophisticated equipment should not deter us from measuring the intra-abdominal pressures in critically ill children.