Introduction
Many of us think of Botox primarily as a cosmetic treatment for lines and wrinkles on the face, but the botulinum toxin that Botox is derived from has a long history of medically therapeutic uses such as in cervical dystonia, hyperhidrosis, strabismus and blepharospasm. Botox has now been increasingly used in dentistry as well due to its therapeutic uses in treatment of certain oral conditions. The Dental Quality Assurance Commission (DQAC) of Washington has released an interpretive statement effective July 26, 2013, which now affirms the ability of general dentists to use Botox and dermal fillers when “used to treat functional or aesthetic dental conditions and their direct aesthetic consequences and the treating dentist has appropriate, verifiable training and experience.”Similarly, Michigan board of dentistry and New Jersey state board also approves the use of Botox and dermal fillers by general dentists. Botulinum toxin is a protein and neurotoxin produced by the bacterium Clostridium botulinum [1] [Table/Fig-1] [2]. Currently, seven botulinum neurotoxin serotypes (A, B, C1, D, E, F, and G) produced by Clostridium botulinum, are recognized. Although botulinum toxin is a lethal, naturally occurring substance, it can be used as an effective and powerful medication [3].
Commercially available Botulinum Toxin A as Botox (Allergan) [2]

Three forms of botulinum toxin type A (Botox, Dysport and Xeomin) and one form of botulinum toxin type B (MyoBloc) are available commercially for various cosmetic and medical procedures.
Each vial of BOTOX contains-
100 Units (U) of Clostridium botulinum type A neurotoxin complex,
0.5 milligrams of Albumin Human,
And 0.9 milligrams of sodium chloride in a sterile, vacuum-dried form without a preservative.
Botulinum toxin type A can be used in following dental conditions:-
Temporomandibular joint disorders
Bruxism
Oromandibular dystonia
Mandibular spasm
Pathologic clenching
Dental implant and surgery
Gummy smile
Masseteric hypertrophy
Mechanism of Action
Injecting overactive muscles with minute quantities of botulinum toxin type-A results in decreased muscle activity. Botulinum toxin type-A inhibits the exocytosis of acetylcholine on cholinergic nerve endings of motor nerves [4], as it prevents the vesicle where the acetylcholine is stored from binding to the membrane where the neurotransmitter can be released. Botulinum toxin achieves this effect by its endopeptidase activity against SNARE proteins, which are 25-kd synaptosomal associated proteins that are required for the docking of the ACH vesicle to the presynaptic membrane [5]. Botulinum toxin type-A thus blocks the release of acetylcholine by the neuron. This effectively weakens the muscle for a period of three to four months [6].
Temporomandibular Joint Disorders
Temporomandibular disorder (TMD) is a term used to describe a number of diseases affecting masticatory function, which may include true pathology of the temporomandibular joint as well as masticatory muscle dysfunction [7,8]. TMD manifests with facial pain, joint sounds, headache, peri-auricular pain, neck pain, and/or decreased jaw excursion. The majority of TMD cases include a myogenic component [9,10] and muscular spasticity secondary to bruxism, external stressors, oromandibular dystonia, and psychomotor behaviours are common aetiologic factors of TMD [11].
TMD caused by excessive biting forces has conventionally been treated with intraoral appliances, occlusal adjustments, dental restoration, and/or surgery. These techniques are invasive, irreversible, and expensive for the majority of patients.
Techniques currently employed for aesthetic, conservative restorations may not withstand the parafunctional forces continually applied by some patients. Thus, many of these treatment options are not ideal for all patients, and muscular relaxation with botulinum toxin A is a viable alternative. When a muscle relaxant is used with the muscles of mastication, this clenching reflex can be reduced or eliminated [12]. Because a very small percentage of available force is required to masticate food, a slight relaxation of muscle function reduces bruxing and is usually insufficient to affect chewing and swallowing [13].
Dentofacial Aesthetics
Botox and Dermal fillers can provide immediate volume to areas around the mouth, such as the nasolabial folds, marionette lines, and lips to create the proper lip lines, smile lines, and phonetics. Dermal fillers, such as Juvéderm® and Restylane®, are volumizers—or plumpers—that fill out lips and static folds in the face caused by loss of collagen and fat.
Botox can also be used in a lip deformity where the lip rises more on one side than the other. It has to be injected at a specific site controlling where the lip goes and how much of it is raised and where and finally, the dreaded “black triangles” which is one of the most challenging aesthetic problems, for which there are very limited successful treatment options. Food particles accumulate in the space and create aesthetic issues. Dermal fillers can be injected into the interdental papilla to plump it and close the interdental space [Table/Fig-2][14]. Treatment outcome usually last for eight months or longer—at which point the treatment needs to be repeated.
Black triangles between the teeth can be filled up by Botulinum toxin A [14]

Bruxism
Botulinum neurotoxin has also shown promise in alleviating the symptomatology of bruxism. One of the earliest reports on use of botulinum toxin type A for bruxism was by Van Zandijcke and Marchau [15], who described the successful treatment of a brain-injured patient with severe bruxism with 100 U of a botulinum toxin type A injections to the temporalis and masseter muscles.
Dental Implants and Surgery
Overloading of the muscles of mastication can prevent or impede osseointegration of implants and/or fracture callus formation [16,17]. The muscular relaxation achieved with botulinum toxin type A injections to the masticatory muscles can be therapeutically beneficial by allowing implants better unimpeded osseointegration and fracture healing in a more stable environment.
Kayikvioglu and colleagues [17] conducted a small open-label study to prospectively examine the use of botulinum toxin type A as an adjunct to zygomatic fracture fixation surgery, in an attempt to reduce the number of fixation sites and to prevent dislocation of the zygomatic bone. Five male patients with zygomatic bone fractures were injected with 100 U of botulinum toxin type A into the masseter muscle of the fractured side. Patients were then operated on 12 to 48 h after the injection and EMG confirmation of muscle denervation. The temporary paralysis of the masseter muscles allowed for fewer miniplate and/or microplate insertions in all patients, and resulted in no complications related to either the botulinum toxin injections or surgical procedures [17]. Kayikvioglu’s group also found similar benefits of adjunct botulinum toxin treatment for surgical reduction of mandibular and condylar bone fractures [17].
Gummy Smile
The display of excessive gingival tissue in the maxilla upon smiling, or “gummy smile,” is both an oral hygiene and cosmetic issue with no simple remedy. Excessive gum exposure is frequently attributable to over-contraction of the upper lip muscles, particularly the levator labii Superioris alaeque nasi. Although several surgical techniques have been reported in the literature for correction of hyperfunctional upper lip elevator muscles, such as the Rubinstein and Kostianovsky [18], Miskinyar [19], and Rees and LaTrenta [20] techniques, they are not routinely used to treat gummy smile [21]. In general, the most common surgical corrections currently used are the LeFort I maxillary osteotomies with impaction for skeletal vertical maxillary excess, and gingivectomies for delayed passive dental eruption with excessive gingival display [21,22].
Botulinum toxin should be injected in small, carefully titrated doses to limit muscular over-contraction of upper lip, thus reducing exposure of the upper gums when smiling. Hwang et al., at Yonsei University College of dentistry, Seoul, Korea have proposed a injection point for botulinum toxin and named it as Yonsei point [23]. It is basically a point located at the centre of triangle formed by levator labii superioris, levator labii superioris alaeque nasi and zygomaticus minor [Table/Fig-3] [24]. A dose of 3U is recommended at each injection site.
Botulinum toxin A is being used in treating patients with gummy smile [24]

In a small open-label trial, five patients with excessive gingival display resulting from hyperfunctional upper-lip elevator muscles were treated with Botox injections under electromyographic guidance [25]. Patients received one 0.25 U per muscle bilaterally into the levator labii superioris, levator labii Superioris alaeque nasi, and at the overlap areas of the levator labii superioris and zygomaticus minor muscles. All of the patients were pleased with the results and the effective increase in upper-lip length upon smiling averaged 124.2% [25]. The duration of effect ranged from 3 to 6 months, and no adverse effects were reported or observed. However, the improvement is temporary and must be repeated every six months to one year.
Masseteric Hypertrophy
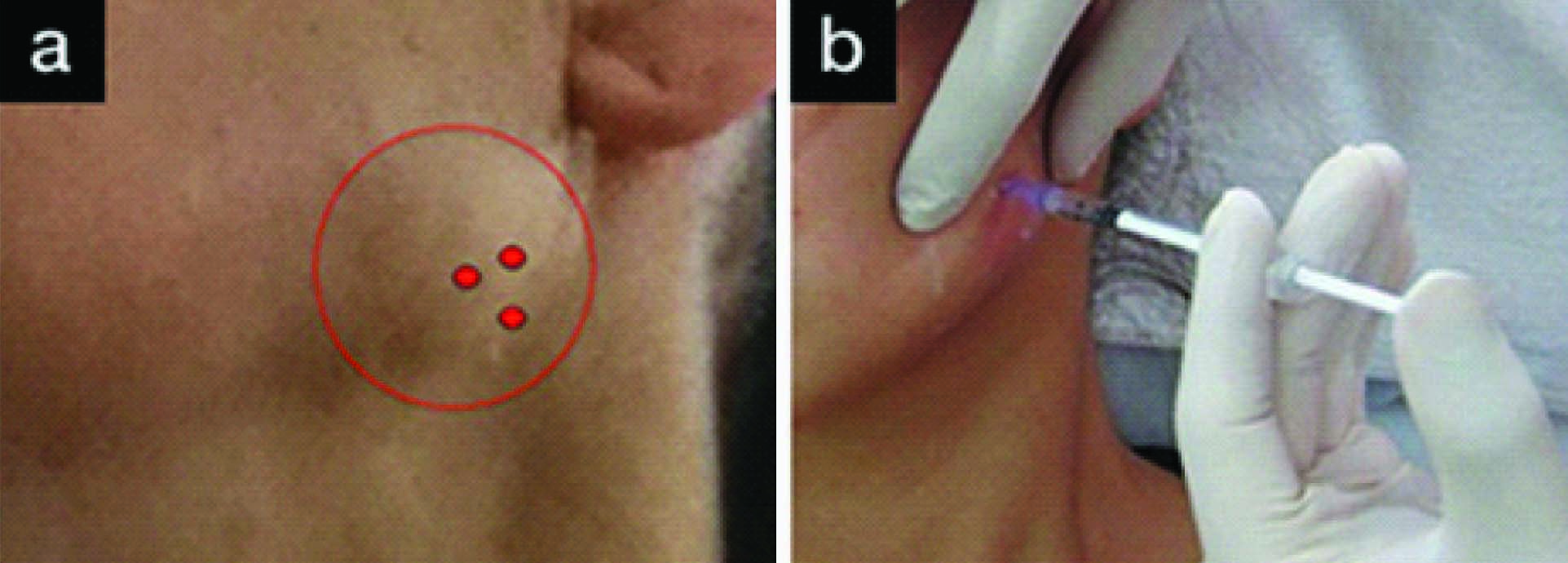
Patients who are chronic jaw clenchers frequently present with masseter hypertrophy [26,27]. The increased size of these muscles is evident in the patient’s facial appearance which is often substantially altered. The jaw appears swollen and misshapen. The common treatment before botulinum toxin was surgical resection [28], which results in substantial contracture. In several small but well-documented clinical trials, the injection of small aliquots (e.g., 30 U per side) of Botox into the masseter muscles resulted in a sustained reduction of masseter hyperactivity [26,27,29,30] [Table/Fig-4a,b] [31]. Over time, in most patients, reduction in masseter hyperactivity has been found to yield a concomitant reduction in gross masseter size (maximum reduction 35.4%) [27]. If the underlying pathology responsible for the hyperactivity is resolved, the reduction in masseter hypertrophy remains an enduring effect even after Botox applications have ceased [29,30].
(a)Location for botulinum toxin A injection in hypertrophied masseter muscle (b) botulinum toxin A injection of masseteric hypertrophy [31]
Mandibular Spasm
When the mandibular closing musculature remains semicontracted or in spasm, mouth opening becomes limited. This type of muscular spasm places limitations on completing the basic oral hygiene necessary to prevent oral disease [32]. Other impairments can include: restrictions on dental treatment, difficulty with eating and diminished oral utility (a broad spectrum of oral functions are impaired by restricted opening and the contraction of bite radius). Botulinum toxin treatment to the masticatory musculature diminishes the effects of hyperfunctional or spastic muscles [33].
Oromandibular Dystonia
Oromandibular dystonia (OMD) is a movement disorder characterized by involuntary spasms and muscle contractions. It manifests as distorted oral position and function resulting in difficulty in speaking, swallowing, and eating. Although it is a neurologic disorder, it is included as a subset of TMD because of its involvement of the masticatory apparatus [34]. Most of the reported literature on OMD has been open-label studies, but all have reported improvement with botulinum toxin injections [35–39]. The largest study to date was a prospective open-label conducted by Tan and Jankovic that treated 162 patients with OMD over a 10-year period [39]. Botulinum toxin type A was injected into the masseters and/or the submental is complex. Improvement in function for chewing and speaking was reported in 67.9% of the patients, and mean duration of clinical improvement was 16.4 ± 7.1 wk [38].
Pathologic Clenching
Excessive forces created by parafunctional clenching impede healing and reattachment of gum and bone in the mouth after trauma [40]. Botulinum toxin type A limits the muscle contraction, and this reduction in clenching intensity will allow traumatized tissue to heal. Because parafunctional clenching contributes to periodontal trauma, botulinum toxin type A can limit clenching before and after periodontal surgery to improve healing. Further, in this application, the use of a splint is often contraindicated because the teeth should be functional during healing, so Botulinum toxin acts as a pharmaceutical splint.
Orthodontic treatments on patients who are clenchers or have a deep or crossed bite are prolonged if the vertical component of muscular force is greater than the force of the fixed or removable appliance. These cases often require the use of removable functional retainers in combination with regular fixed braces in an attempt to control the component of vertical force [41]. With the use of botulinum toxin, orthodontic treatment time can be reduced, and patients would be far more comfortable and functional (eating, speaking, swallowing).
Other Uses
Sialorrhea: This toxin also blocks the release of acetylcholine at the cholinergic synapses of the autonomic nervous system; thus, this toxin can block cholinergic parasympathetic secretomotor fibers of the salivary gland. Hence, botulinum toxin has been tested in some autonomic disease, such as achalasia, hyperhidrosis and gustatory sweating (Frey syndrome) [42]. Lim and Choi [43] have reported that injection of botulinum toxin type A is a highly effective and relatively safe primary method of treatment for an acute postparotidectomy salivary fistula that, if treated with conventional pressure dressings, takes long to subside.
Trigeminal Neuralgia: BOTOX 25–75 U injected into pericranial muscles relieves headache by relaxing the over active muscles by blocking nerve impulses that trigger contractions. According to Elcio, excruciating pain associated with inflammation of the trigeminal nerve of the head and face can be substantially relieved by injections of BOTOX [44].
Retraining Muscles During Orthodontic Treatment: Botox can be used to prevent relapse of orthodontic treatment in case of patients with stronger muscle activity such as that of mentalis muscle. Botox can be used to reduce the intensity of the muscle post treatment and over time, the muscle may be retrained to a more physiological movement.
Botox can be used in patients with a new denture especially if the patient has long history of edentulousness and has decreased vertical dimension.
Higher doses of botulinum toxin type A may potentially be used as a pharmaceutical splint, limiting muscle contraction before resetting and during rehabilitation after fracture of a facial bone (e.g., fractured mandibular condyle).
Botulinum toxin type A can be used to verify whether the pain is muscular or pulpal (e.g., complex toothache) in origin in patients with chronic intermittent toothache [45]. For example, muscle pain from the anterior temporalis is often referred to the teeth. This should be treated before any major irreversible dental treatments are undertaken. In this context, the use of botulinum toxin type A is both prophylactic as well as diagnostic.
Contraindications
Patients should not be treated or treated with extreme caution who are [46]:
Psychologically unstable or who have questionable motives and unrealistic expectations.
Dependent on intact facial movements and expressions for their livelihood (e.g. actors, singers, musicians and other media personalities).
Afflicted with a neuromuscular disorder (e.g.myasthenia gravis, Eaton-Lambert syndrome).
Allergic to any of the components of BTX-A or BTX-B (i.e. BTX, human albumin, saline, lactose and sodium succinate).
Taking certain medications that can interfere with neuromuscular impulse transmission and potentiate the effects of BTX (e.g. aminoglycosides, penicillamine, quinine, and calcium blockers).
Pregnant or lactating (BTXs are classified as pregnancy category C drugs)
Discussion
Botox is a safe, conservative, non surgical, reversible, minimally invasive treatment modality to achieve cosmetic results. Training is absolutely necessary for dentists to administer injections, but learning curve is very short, because dentists can already achieve profound anaesthesia in the orofacial region, thus making patient more comfortable and at ease. Botulinum toxin A is kept frozen (2–40C) in a vial until it is ready to use. The drug is put into solution, following manufacturer’s guidelines, by adding normal saline (preservative-free 0.9% saline solution). Once prepared it should be used within four hours. The preferred syringe is a calibrated 1.0-mL tuberculin syringe, and the needle selected for injection usually is between 26 and 30 gauge. Skin preparation involves alcohol wipes and dry sterile gauze sponges. Aspiration before injection is recommended to avoid involuntary deposition of toxin into the facial arteries. Botulinum Toxin A achieves close to immediate results in one short appointment, but the results are not permanent and last for 6 months, with a range of 4-8 months [47]. Botulinum Toxin needs to be administered 2-3 times a year depending upon the declination of its effect. The therapeutic effects of Botulinum toxin A first appear in 1 to 3 d, peak in 1 to 4 wk, and decline after 3 to 4 mnth [48]. At the cellular level, 3 to 4 wk after a single injection of Botulinum toxin A in mice, there is sprouting of new processes along the nerve axon, with formation of multiple synapses with the muscle and up regulation of the muscle nicotinic receptors. Subsequently, the neuronal sprouts undergo regression and the original synaptic connection is restored, with restoration of the original neuromuscular junction [46,49]. Therefore, Botulinum toxin injections are needed to be administered 2-3 times a year, thereby increasing the cost factor to slightly higher level. Injections are spaced out for a minimum of three months to minimize the risk of antibody formation to the protein,which would prevent BOTOX from working the subsequent time [45]. Mild stinging, burning or pain with injection, edema and erythema around injection site are the localized adverse effects which are of limited duration .The potential adverse effects of botulinum toxin in oromandibular disorders include facial nerve palsy, pain at the injection site, flu-like symptoms, non-targeted muscle weakness, dysphagia, and hematoma. These complications are generally transient, and resolve within a couple of weeks. Hands-on training is essential in learning proper techniques of administration and intertwining them with dental treatment plans. With proper training, dentists are usually more proficient than any of other healthcare professionals in providing these treatments to patients, both for dental and cosmetic needs.The American Academy of Facial Aesthetics is conducting more than 50 local courses a year, has trained more than 6,000 dental professionals from 48 states and 28 countries through comprehensive hands-on live patient two-day facial aesthetic training sessions with Botox and dermal fillers [50]. The Indian Academy of Facial Aesthetics (IAOFE) in conjunction with the American Academy of Facial Aesthetics (AAFE) is also offering Botox and dermal fillers training course for dentists and physicians [51].
Conclusion
BOTOX has important clinical uses as an adjunct therapy in temporo mandibular joint (TMJ) and bruxism cases, and for patients with chronic TMJ and facial pain. BOTOX is also used to complement aesthetic dentistry cases, as a minimally invasive alternative to surgically treating high lip-line cases, for denture patients who have trouble adjusting to new dentures, periodontal cases, gummy smiles, lip augmentation, and also for orthodontic cases where retraining of the facial muscles is necessary. However, much more is still to be discovered before its routine use in dentistry for various conditions. There are still many dental conditions which require FDA approval to be treated by botulinum toxin. Botulinum toxin has no doubt broadened the horizon of dentistry and is persuading dentists all over the world to bring it into their clinical practices.
[1]. Montecucco C, Molgó J, Botulinal neurotoxins: revival of an old killerCurrent Opinion in Pharmacology 2005 5(3):274-79. [Google Scholar]
[2]. http://www.kencomerdds.com/botox.html [Google Scholar]
[3]. Barbano Richard, Risks of erasing wrinkles: Buyer beware!Neurology 2006 67(10):E17-18. [Google Scholar]
[4]. Meunier FA, Schiavo G, Molgo J, Botulinum neurotoxins: from paralysis to recovery of functional neuromuscular transmissionJ Physiol (Paris) 2002 96(1–2):105-13. [Google Scholar]
[5]. Aoki KR, Evidence for antinociceptive activity of botulinum toxin type A in pain managementHeadache 2003 43(Suppl 1):S9-15. [Google Scholar]
[6]. Edwards, Michael (2006). "Anal fissure". Dumas Ltd. Retrieved August 21, 2010 [Google Scholar]
[7]. Bentsianov BL, Francis A, Blitzer A, Botulinum toxin treatment of temporomandibular disorders, masseteric hypertrophy, and cosmetic masseter reductionOperative Techniques in Otolaryngology-Head and Neck Surgery 2004 15(2):110-13. [Google Scholar]
[8]. Olivo S, Bravo J, Magee DJ, The association between head and cervical posture and temporomandibular disorders: A systematic reviewJ Orofac Pain 2006 20(1):9-23. [Google Scholar]
[9]. Schwartz M, Freund B, Botulinum Toxin A Therapy for Temporomandibular Disorders 2002 Philadelphia, PaLippincott Williams & Wilkins [Google Scholar]
[10]. Schwartz M, Freund B, Treatment of temporomandibular disorders with botulinum toxinClin J Pain 2002 18(6 Suppl):S198-203. [Google Scholar]
[11]. Castenada R, Occlusion. In: Kaplan A, Assael L (eds)Temporomandibular Disorders 1992 Philadelphia, PaSaunders [Google Scholar]
[12]. Gobel H, Heinze A, Heinze-Kuhn K, Botulinum Toxin A is effective in cases of oromandibular dysfunction even if previous bite splint therapy has proved unsuccessfulCephalalgia 2001 :514-15. [Google Scholar]
[13]. Freund B, Schwartz M, Symington JM, The use of botulinum toxin for the treatment of temporomandibular disorders: Preliminary findingsJ Oral Maxillofac Surg 1999 57(8):916-21. [Google Scholar]
[14]. http://www.dentaltown.com/dentaltown [Google Scholar]
[15]. Van Zandijcke M, Marchau MM, Treatment of bruxism with botulinum toxin injectionsJ Neurol Neurosurg Psychiatry 1990 53(6):530 [Google Scholar]
[16]. Nishimura K, Itoh T, Takaki K, Periodontal parameters of osseointegrated dental implants: A four-year controlled follow-up studyClin Oral Implants Res 1997 8(4):272-78. [Google Scholar]
[17]. Kayikvioglu A, Erk Y, Mavif E, Botulinum toxin in the treatment of zygomatic fracturesPlast Reconstr Surg 2003 111(1):341-46. [Google Scholar]
[18]. Rubenstein A, Kostianovsky A, Cosmetic surgery for the malformation of the laugh: original techniquePrensa Med Argent 1973 60:952 [Google Scholar]
[19]. Miskinyar SA, A new method for correcting a gummy smilePlast Reconstr Surg 1983 72:397-400. [Google Scholar]
[20]. Rees T, LaTrenta G, The long face syndrome and rhinoplastyPersp Plast Surg 1989 3:116 [Google Scholar]
[21]. Polo M, Botulinum toxin type A in the treatment of excessive gingival displayAm J Orthod Dentofacial Orthop 2005 127(2):214-18. [Google Scholar]
[22]. Amin V, Amin V, Swathi,Jabir A, Shetty P, Enhancing the smile with Botox-case reportGlobal Journal of Medical Reasearch 2013 13(2):14-18. [Google Scholar]
[23]. Hwang Surface anatomy of the lip elevator muscles for the treatment of gummy smile using botulinum toxinAngle Orthod 2009 79(1):70-77. [Google Scholar]
[24]. http://www.vancouverlaser.com/procedures-treatments/botox-before-after-photos-05/ [Google Scholar]
[25]. Polo M, Botulinum toxin type A in the treatment of excessive gingival displayAm J Orthod Dentofacial Orthop 2005 127(2):214-18. [Google Scholar]
[26]. Kim HJ, Yum KW, Lee SS, Effects of botulinum toxin type A on bilateral masseteric hypertrophy evaluated with computed tomographic measurementDermatol Surg 2003 29(5):484-89. [Google Scholar]
[27]. Al-Ahmad HT, Al-Qudah MA, The treatment of masseter hypertrophy with botulinum toxin type ASaudi Med J 2006 27(3):397-400. [Google Scholar]
[28]. Clark GT, The management of oromandibular motor disorders and facial spasms with injections of botulinum toxinPhys Med Rehabil Clin North Am 2003 14(4):727-48. [Google Scholar]
[29]. Mandel L, Tharakan M, Treatment of unilateral masseteric hypertrophy with botulinum toxin: Case reportJ Oral Maxillofac Surg 1999 57(8):1017-19. [Google Scholar]
[30]. Rijsdijk BA, Van Es RJJ, Zonneveld FW, Botulinum toxin type A treatment of cosmetically disturbing masseteric hypertrophyNed Tijdschr Geneeskd 1998 142(10):529-32. [Google Scholar]
[31]. http://www.dentmaster.ru/articles/109 [Google Scholar]
[32]. Erdal J, Werdelin L, Prytz S, Experience with long-term botulinum toxin treatment of oromandibular dystonia, guided by quantitative EMGActa Neurologica Scandinavica 1996 94(6):210 [Google Scholar]
[33]. Cersosimo MG, Bertoti A, Roca CU, Botulinum toxin in a case of hemimasticatory spasm with severe worsening during pregnancyClin Neuropharmacol 2004 27(1):6-8. [Google Scholar]
[34]. Blitzer A, Brin MF, Greene PE, Botulinum toxin injection for the treatment of oromandibular dystoniaAnn Otol Rhinol Laryngol 1989 98(2):93-97. [Google Scholar]
[35]. Brin MF, Fahn S, Moskowitz C, Localized injections of botulinum toxin for the treatment of focal dystonia and hemifacial spasmMov Disord 1987 2(4):237-54. [Google Scholar]
[36]. Hermanowicz N, Truong DD, Treatment of oromandibular dystonia with botulinum toxinLaryngoscope 1991 101(11):1216-18. [Google Scholar]
[37]. Jankovic J, Orman J, Botulinum toxin for cranial-cervical dystonia: a double-blind, placebo-controlled studyNeurology 1987 27:616-23. [Google Scholar]
[38]. Laskawi R, Rohrbach S, Oromandibular dystonia. Clinical forms, diagnosis and examples of therapy with botulinum toxinLaryngorhinootologie 2001 80(12):708-13. [Google Scholar]
[39]. Tan EK, Jankovic J, Botulinum toxin A in patients with oromandibular dystonia: Long-term follow-upNeurology 1999 53(9):2102-07. [Google Scholar]
[40]. Glaros A, Tabacchi K, Glass EG, Effect of parafunctional clenching on TMD pain and hearing lossJ Orofacial Pain 1998 12(2):145-52. [Google Scholar]
[41]. Freund B, Schwartz M, Symington JM, The use of botulinum toxin for the treatment of temporomandibular disorders: Preliminary findingsJ Oral Maxillofac Surg 1999 57(8):916-21. [Google Scholar]
[42]. Laskawi R, Drobik C, Schönebeck C, Up-to-date report of botulinum toxin type A treatment in patients with gustatory sweating (Frey's syndrome)Laryngoscope 1998 108(3):381-84. [Google Scholar]
[43]. Lim YC, Choi EC, Treatment of an acute salivary fistula after parotid surgery: botulinum toxin type A injection as primary treatmentEur Arch Otorhinolaryngol 2008 265(2):243-45. [Google Scholar]
[44]. Elcio JP. BOTOX injections relieve severe facial pain. Available from: http://www.news-medical.net/news/2005/10/25/14010.aspx. [last citedon 2009] [Google Scholar]
[45]. Rao LB, Sangur R, Pradeep S, Application of Botulinum toxin Type A: An arsenal in dentistryIndian J Dent Res 2011 22:440-45. [Google Scholar]
[46]. Patel D, Mehta F, Trivedi R, Thakkar S, Suthar J, Botulinum Toxin and Gummy smile-A ReviewIOSR Journal of Dental and Medical Sciences 2013 4(1):1-5. [Google Scholar]
[47]. Grover S, Malik V, Kaushik A, Diwakar R, Yadav P, A Future perspective of Botox in Dentofacial RegionJ Pharm Biomed Sci 2014 04(05):525-31. [Google Scholar]
[48]. Clark Botulinum toxin in orofacial pain disordersDent Clin N Am 2007 51:245-61. [Google Scholar]
[49]. Comella Jankovic C, Brin M. F, Dystonia: Etiology, Clinical Features, and TreatmentPhiladelphiaLippincott Williams & Wilkins:93-112. [Google Scholar]
[50]. www.FacialAesthetics.org [Google Scholar]
[51]. http://www.iaofe.com/about.html [Google Scholar]