Comparison of Mast Cells and Inflammatory Cells within Periapical Lesions and Comparison of Degranulated Mast Cells Between Fibrous and Inflamed Area in Radicular Cysts: An Immunohistochemical Study
Aseem Shiromany1, Rahul Sood2, Syed Akifuddin3, Gagandeep Kaur Sidhu4, Nadia Khan5, Kapil Singla6
1 Reader, Department of Conservative & Endodontics, KD Dental CollegeMathura, (UP), India.
2 Professor and Head, Department of Oral and Maxillofacial Surgery, Maharaja Ganga Singh Dental College and Research Center, Sriganganagar, Rajasthan, India.
3 Reader, Department of Oral and Maxillofacial Surgery, Daswani Dental College & Hospital, Kota, Rajasthan, India.
4 Senior Lecturer, Department of Oral Pathology and Microbiology, Maharaja Ganga Singh Dental College and Research Center, Sriganganagar, Rajasthan, India.
5 Reader, Department of Pedodontics, Carier Postgraduate Institute of Dental Sciences and Hospital, Lucknow, India.
6 Senior Lecturer, Department of Prosthodontics, Adesh Institute of Dental Sciences and Research, Bathinda, Punjab, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Aseem Shiromany, Reader, Department of Conservative & Endodontics, KD Dental College, Mathura, U.P., India.
Objective: The role of mast cells as the key effector of allergic inflammation, anaphylactic inflammatory reactions and in the pathogenesis of chronic inflammation, is well-known. The present study is adopted to compare mast cells and inflammatory cells within periapical granuloma and cysts and localize the mast cells and quantify their number in the periapical cysts so as to propose a role of mast cells in the pathogenesis of this lesion.
Materials and Methods: Biopsy specimens of 30 periapical lesions were stained with hematoxylin–eosin, and immunohistochemical Mast Cell Tryptase from Bio SB (IHC detection system kit) antibody. The tryptase positive mast cells and mononuclear inflammatory cells were counted in 10 consecutive high power fields (100X) using the binocular microscope from Motic attached to a computer with Motic Advanced Images 3.2 software.
Results: Comparative microscopic analysis indicated that periapical cyst shows more percentage of mast cells and less percentage of inflammatory cell than periapical granuloma (comparison of mean and standard deviation of total number of mast cells and inflammatory cells, mast cells 3.15±1.39 in the granuloma group and 4.43±1.91in the cyst group, inflammatory cells, 67.11±1.2 in the granuloma group and 52.66±0.8 in the cyst group). Numerous degranulated mast cells were observed in the fibrous wall than the inflammatory infiltrate of the periapical cysts. The mean and standard deviation of degranulated mast cells between the inflammatory and fibrous zone within the cyst group, being 0.95±1.10 and1.68±1.34 respectively. The values varied significantly between the two zones.
Conclusion: The number of inflammatory cells in the cyst group is less than periapical granuloma and total number of mast cells in the cyst group is more as compared to periapical granuloma. The degranulated cells were quantified and they were higher in the fibrous area of the cysts than the inflammatory zone. This study could support the fact that the various mediators released on degranulation play a role in the connective tissue remodeling, chronicity and expansion of the periapical lesion.
Cancer, Gender gap, Proportion-tobacco related cancers, Tobacco
Introduction
The healthy dental pulp is protected from oral microorganisms by enamel and dentin. Exposure of the dental pulp to bacteria and their by-products, acting as antigens, may elicit nonspecific inflammatory responses as well as specific immunological reactions in the periradicular tissues. The periradicular lesions formed are the result of the local defense reactions against the bacterial challenge. Periradicular granulomas represent a subsequent reparative process of chronic local inflammation whilst periradicular cysts are thought to be derived from epithelial rests within or adjacent to granulomatous tissue. The tissues of periradicular lesions are infiltrated by specific and nonspecific cells involved in the local immunological responses. The local antigen presentation taking place in periradicular tissues leads to activation of immune cells [1].
Periapical lesions are the most common osteolytic lesions in the maxilla and mandible. Both granulomas and radicular cysts are thought to represent two different stages of development of the same inflammatory process. They are characterized by the infiltration of lymphocytes, plasma cells, mast cells and macrophages into the granulomatous tissue. A sequel to granuloma formation is the proliferation of the epithelial cell rests of Malassez associated with the inflammation, which may lead to the development of an inflammatory radicular cyst [2].
The role of mast cells as the key effector of allergic inflammation, anaphylactic inflammatory reactions and in the pathogenesis of chronic inflammation, is well-known [3]. Perrini and Fonzi suggested that IgE has an active role in the pathogenesis of the periapical granuloma, and that the anaphylactic and hypersensitivity reactions represent an active immunologic phenomenon in the pathogenesis of these lesions [4]. Mast cells are able to produce a wide variety of mediators, creating reciprocal functional interaction between mast cell activation and subsequent T-cell stimulation [3]. Mast cells appear to modulate CD8+T cell proliferative responses and cytokine production and to present antigens in vitro. Mast cells may also prime T cells in vivo for efficient T cell as well as antibody responses to specific antigens [5]. The present study is adopted to compare mast cells and inflammatory cells within periapical granuloma and cysts and to identify the role of degranulated mast cells in fibrosis and bone resorption thus to identify the role in the pathogenesis of the lesion.
Materials and Methods
The present retrospective study was conducted in Department of Oral and Maxillofacial Pathology in our institute and Biopsy specimen of 30 periapical lesions were selected on the basis of microscopic examination of slides stained with hematoxylin and eosin from the archives of the institute. A total of 15 cases each of periapical granuloma and periapical cyst were included in this study. For microtomy, paraffin blocks of the selected subjects were taken and sectioning was done using semiautomatic Rotary Microtome for making 5μ thick sections (Leica RM 2245) and were mounted on super frost slides (size 25x75x1.0mm). Immuno histochemical study was carried out using polymer labeling technique (Dako Envision). Sections were dewaxed, washed in alcohol and antigen retrieval was carried out in a Decloaking Chamber (Biocare) with 10 mM Citra solution at 125°C for 30 seconds followed by 90°C for 10 seconds. Slides were cooled naturally and brought to room temperature. Then were placed inside the Dako Autostainer Universal Staining System (Automated Immunohistochemistry Staining System). Endogenous peroxidase was blocked by using 0.3% hydrogen peroxide in methanol at room temperature for 10 min. Sections were washed PBS (Phosphate Buffered Saline) briefly and incubated with primary antibody (Mast Cell Tryptase from Bio SB) for 60 min. Diaminobenzidine (DAB) was used as the chromogen in hydrogen peroxide for 10 min. Sections were then counterstained with haemotoxylin and mounted. The mast cells usually take up brown stain against blue staining stroma, fibroblasts and inflammatory cells. Mast cells could be of varying shapes, some of them with intact cell membrane whereas others showing degranulation. In some of the cells, the nucleus could be masked by the mast cell granules. So, these criteria were followed for evaluation of slides. Mast cells were counted in a representative section of each slide. These cells were counted in 10 consecutive high power fields (100X) using the binocular microscope from Motic attached to a computer with Motic Advanced Images 3.2 software. The grid consisted of 100 squares each measuring 1μmx1μm in size. The fields containing artefactual changes such as chatter, tears etc were omitted from the study. Granules lying irregularly in the stroma were not taken into account.
Statistical Analysis
Data analysis and database management were done using SPSS (statistical package for social science) version 16.00. Level of significance was set up at p < 0.05. T-test for equality of means was applied. Level of significance was set up at p < 0.05.
Results
General and qualitative microscopic analysis indicated that periapical cysts exhibit greater mean number of mast cells than the periapical granuloma where as mean number of inflammatory cells appear to be more in periapical granuloma group than in the cyst group (as indicated in [Table/Fig-1] shows comparison of mean and standard deviation of total number of mast cells, 3.15±1.39 in the granuloma group and 4.43±1.91 in the cyst group and comparison of mean and standard deviation of total number of inflammatory cells, 67.11±1.2 in the granuloma group and 52.66±0.8 in the cyst group. Thus the mean number of mast cells is more in the cyst group than the granuloma group whereas reverse is the case with mean number of inflammatory cells. They are more in the granuloma group, and, as shown in [Table/Fig-1], the results are significantly different. These cells were counted in 10 consecutive high power fields (100X) using the binocular microscope from Motic attached to a computer with Motic Advanced Images 3.2 software in each of the 30 periapical lesion slides, thus N= 150 in each group. Degranulated mast cells were found only in 8 slides of periapical cysts which were counted in 10 consecutive high power fields (100X), thus n= 80 in [Table/Fig-1]. Numerous degranulated mast cells have been observed in the fibrous wall than the inflammatory infiltrate of the periapical cysts. [Table/Fig-2] shows mean and standard deviation of degranulated mast cells between the fibrous and inflammatory zone within the cyst group, being 1.68±1.34 and 0.95±1.10 respectively. The values varied significantly between the two zones [Table/Fig-2]. [Table/Fig-1] depicts a correlation of mean of total number of mast cells and inflammatory cells between the two groups, showing greater number of mast cells and lesser number of inflammatory cells in the cyst group. Indicates a significant difference of the mean number of degranulated mast cells between the inflammatory and fibrous zones within the cyst group, being higher in the fibrous zone.
Comparison of total number of mast cells and inflammatory cells between the two groups
| Group | n | Mean±SD | Std. Error Mean | p-value |
|---|
| Mast cells | Apical Granuloma | 150 | 3.15±1.39 | .113 | .001** |
| Periapical Cyst | 150 | 4.43±1.912 | .156 | .001** |
| Inflammatory cells | Apical Granuloma | 150 | 67.11±1.2 | .11 | .002** |
| Periapical Cyst | 150 | 52.66±0.8 | .12 | .001** |
(mean and standard deviation of total number of mast cells and inflammatory cells) (cells were counted in 10 consecutive high power fields (100X) using the binocular microscope from motic attached to a computer with motic advanced images 3.2 software in each of the 30 periapical lesion slides, thus n= 150 in each group) correlation is significant at the 0.05 level (2-tailed t-test)
Comparison of degranulated mast cells in fibrous and inflammatory zone of periapical cyst group
| Group | n | Mean±SD | Std. Error Mean | p-value |
|---|
| DMC | Fibrous wall | 80 | 1.68±1.394 | .156 | .001** |
| Inflamed Zone | 80 | .95±1.101 | .123 | .001** |
(mean and standard deviation of number of degranulated mast cells in the fibrous and inflammatory zone) (degranulated mast cells were found only in 8 slides of periapical cysts which were counted in 10 consecutive high power fields (100x), thus n= 80) correlation is significant at the 0.05 level (2-tailed t-test)
Discussion
Based on immunohistochemical analysis, author observed periapical cyst shows more percentage of mast cell and less percentage of inflammatory cell than periapical granuloma as seen in [Table/Fig-1]. It is possible that mast cells are more frequently found in cysts as these longstanding lesions are composed of fibrous capsule which contain more mast cells than granulomas. Therefore, the number of inflammatory cells in the cyst group is less and total number of mast cells in the cyst group is more which may account for the more percentage (as percentage=MC/MC+IC*100) of mast cells in cysts. In a similar study carried by Mansata et al., it was found that cysts contained more mast cells than the granulomas [6].
The presence of degranulated mast cells in the periapical cyst, as recorded in the present study may be responsible for the release of various mediators such as heparin, histamine, proteolytic and hydrolytic enzymes. One of the mediators is TNF-α which has been implicated as an important factor in promoting the chronicity of the lesion [7].
The degranulation of mast cells result in the release of primary and secondary mediators. Primary mediators are those which are preformed and are stored in the granules. They are responsible for immediate reactions. Secondary mediators are either synthesized after target cell activation, or are released by the breakdown of membrane phospholipids during degranulation process [8].
The histamine released on degranulation of mast cells promote contraction of smooth muscle and vascular permeability, thereby facilitating transudation of serum proteins and their subsequent entry into the luminal fluid [9]. These observations, taken together, lead to the fact that degranulated mast cells are involved in the expansion of the cyst as well as granulomas but their increased number in the cyst group definitely suggests a more exaggerated response than the periapical granulomas and hence a larger size of the cyst. Another factor is the promotion of inflammation and therefore chronicity of the lesion (through TNF-α).
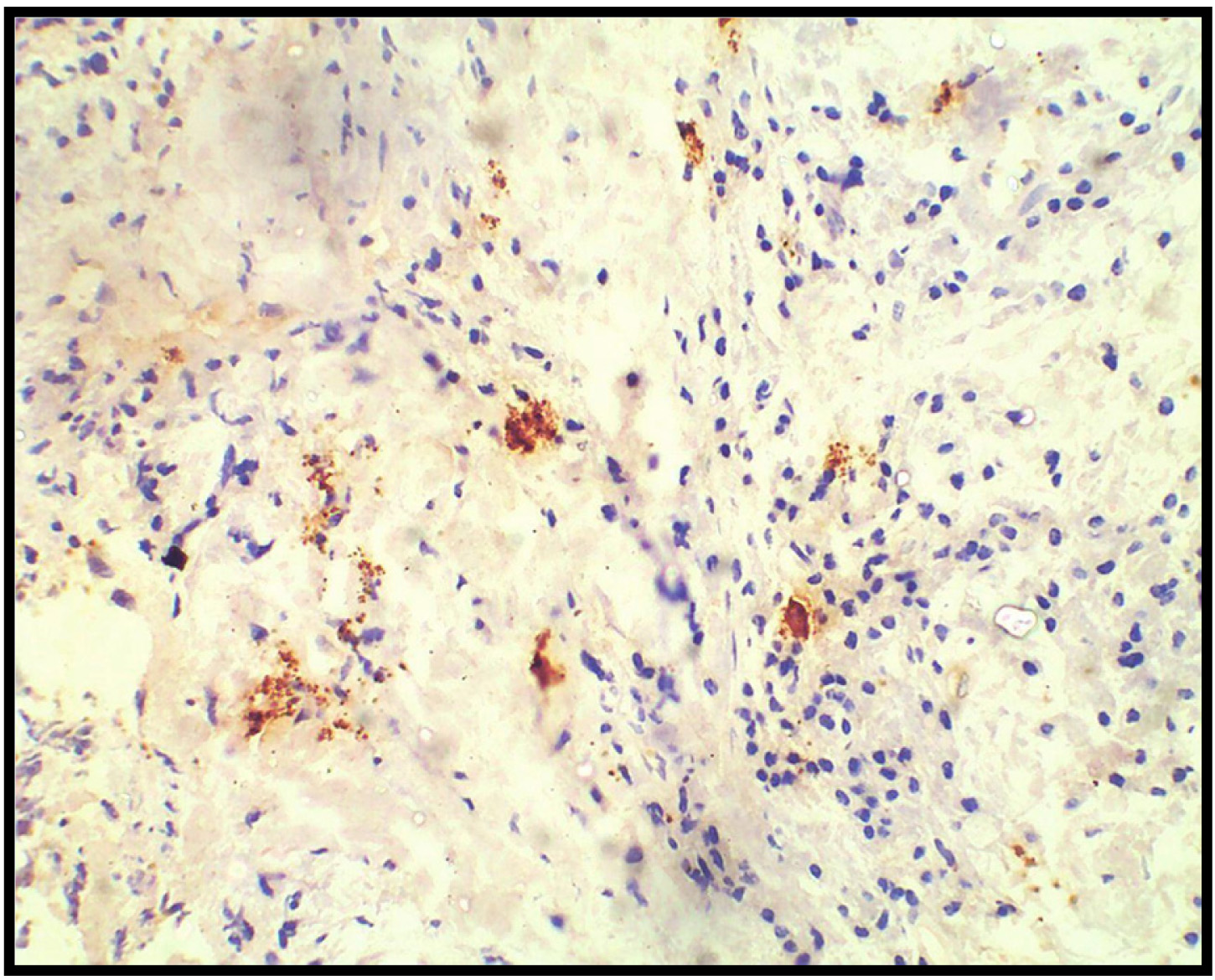
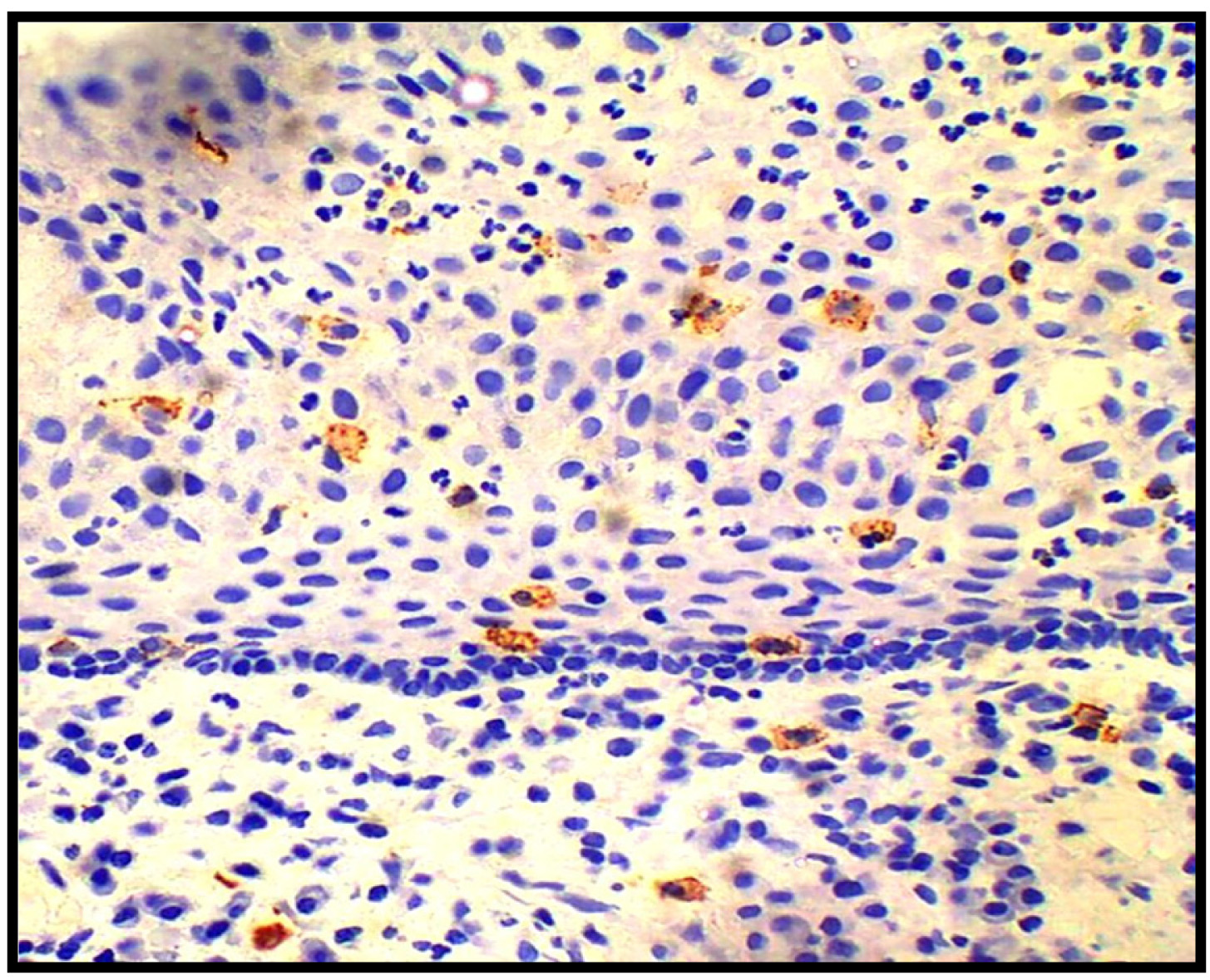
Numerous degranulated mast cells have been observed in the fibrous wall than the inflammatory infiltrate of the periapical cysts [Table/Fig-3,4] in the present study [Table/Fig-2], indicating that the mast cells are active in these areas. These findings agree with those reported by Kontianen et al., but disagree with those of Ledesma Montis et al., [4,10]. It is considered that mast cells contribute to a fibrous tissue formation by production of hyaluronic acid. In addition, there are presumptions that mast cells intensify the growth of collagen fibers by effects of heparin. It has been shown that mast cells activate fibroblasts through tryptase that stimulate collagen mRNA synthesis and promotes collagen formation by fibroblast. Mast cells, like fibroblasts can adhere to fibronectin. This interaction may have possible roles in processes such as fibrosis. Moreover, it has been shown that the administration of mast cell stabilizers can delay or attenuate fibrous tissue formation in peritoneal adhesions. Tryptase, chymase, histamine, heparin, TNF-α, and TGF-β have been shown to influence lung or skin fibroblast proliferation. In addition, TNF-α has been found to be fibrogenic factor for human fibroblasts. Mast cells are reported to specifically influence granulation tissue organization during wound repair [5]. All these findings support the fact that degranulation promotes fibrosis but at the same time other products of degranulation such as tryptase also play a role in the degradation of connective tissue [11]. Thus, the increase in collagen detected after tryptase treatment must reflect an increase in the net biosynthetic rate of type I collagen. Release of collagenase activity concomitant with the deposition of new collagen could be an important process in matrix remodeling [12]. The presence of degranulated mast cells in our study suggests us to speculate about their possible role in fibrous tissue formation as well as degradation. The presence of more number of degranulated cells on the periphery (fibrous area) may suggest that there is continous remodeling of the connective tissue capsule and the net effect seen is fibrosis.
Degranulated mast cells (40X) (100X)
Distribution of mast cells in Periapical Cyst Group (40X)
Another effect of the presence of degranulated mast cells in the periphery of the lesion may suggest their role in the resorption of bone thus promoting cyst growth. Mast cell tryptase, heparin and prostaglandins have been implicated in the process. In addition many of the cytokines produced by activated mast cells, such as IL-1, IL-6 and TNF-α in particular have been shown to increase local osteolytic activity. Furthermore, in systemic mastocytosis, which is characterized by an abnormal proliferation of mast cells, approximately 60-70% of the patients develop radiographically detectable lesions. Inhibition of mast cell mediator release with ketotifen was shown in one case to lead to reversal of bone changes [13]. So, more number of degranulated mast cells in the cyst group suggests more resorption of the bone and hence expansion of the lesion.
Conclusion
The degranulated cells were quantified in the cyst group and they were higher in the fibrous area of the cysts than the inflammatory zone. This study could support the fact that the various mediators released on degranulation play a role in the connective tissue remodeling, chronicity and expansion of the periapical lesion.
(mean and standard deviation of total number of mast cells and inflammatory cells) (cells were counted in 10 consecutive high power fields (100X) using the binocular microscope from motic attached to a computer with motic advanced images 3.2 software in each of the 30 periapical lesion slides, thus n= 150 in each group) correlation is significant at the 0.05 level (2-tailed t-test)
(mean and standard deviation of number of degranulated mast cells in the fibrous and inflammatory zone) (degranulated mast cells were found only in 8 slides of periapical cysts which were counted in 10 consecutive high power fields (100x), thus n= 80) correlation is significant at the 0.05 level (2-tailed t-test)
[1]. Liptas S, Nakou M, Rontogianni D, lnflammatory infiltrate of chronic periradicular lesions: an immunohistochemical studyInternational Endodontic Journal 2003 36:464-71. [Google Scholar]
[2]. Leonardi R, Caltabiano R, Loreto C, Collagenase-3 (MMP-13) is expressed in periapical lesions: an immunohistochemical studyInternational Endodontic Journal 2005 38:297-301. [Google Scholar]
[3]. Radojica Draži, Jelena Sopta, Arsa J, Mini. Mast cells in periapical lesions: potential role in their pathogenesisJ Oral Pathol Med 2010 39(3):257-62. [Google Scholar]
[4]. Perrini N, Fonzi L, Garcés-Ortíz M, Rosales-García G, Hernández-Guerrero JC, Importance of Mast Cells in Human Periapical Inflammatory LesionsJ Endod 2004 30(12):855-59. [Google Scholar]
[5]. Camila de Oliveira Rodini C, Batista AC, Lara VS, Comparative immunohistochemical study of the presence of mast cells in apical granulomas and periapical cysts: possible role of mast cells in the course of human periapical lesionsOral Surg Oral Med Oral Pathol Oral Radiol Endod 2004 97(1):59-63. [Google Scholar]
[6]. Mansata AV, Parikh N, Nandini C, Joshi H, Barad JJ, Dave G, Evaluation of Mast Cells in Periapical Cyst and Periapical Granuloma using Toluidine Blue StainJournal of Research Advancement in Dentistry 2014 3(2):57-63. [Google Scholar]
[7]. Walsh LJ, Davis MF, Xu LJ, Savage NW, Relationship between mast cells degranulation and inflammation in the oral cavityJ Oral Pathol Med 1995 24:166-272. [Google Scholar]
[8]. Singh H, Kumar P, Nanra R, Bhatia A, Mast Cell-A Gatekeeper Of The Microvasculature In The Oral Cavity: A ReviewThe Internet Journal of Pathology 2012 13(2) [Google Scholar]
[9]. Smith G, Smith AJ, Basu MK, Mast cells in human odontogenic cystsJ Oral Pathol Med 1989 18:274-78. [Google Scholar]
[10]. Kontiainen S, Ranta H, Lautenschlager I, Cells infiltrating human periapical inflammatory lesionsJ Oral Pathol 1986 15:544-46. [Google Scholar]
[11]. Ignacio Fajardo, Gunnar Pejler, Human Mast Cell -Tryptase is a gelatinaseJ Immunol 2003 171:1493-99. [Google Scholar]
[12]. Cairns Jennifer A, Walls Andrew F, Mast Cell Tryptase Stimulates the Synthesis of Type I Collagen in Human Lung FibroblastsJ Clin Invest 1997 99:1313-21. [Google Scholar]
[13]. Teronen O, Hietanen J, Lindqvist C, Salo T, Sorsa T, Eklund KK, Mast cell-derived tryptase in odontogenic cystsJ Oral Pathol Med 1996 25(7):376-81. [Google Scholar]