Bullous Lichen Planus treated with Oral Minipulse Therapy: A Rare Case Report
Kotya Naik Maloth1, K Sunitha2, Ramanaryana Boyapati3, Shravan Kumar D.R.4
1 Senior Lecturer, Department of Oral Medicine and Radiology, Mamata Dental College and Hospital, Khammam, Telangana, India.
2 Senior Lecturer, Department of Oral Medicine and Radiology, Mamata Dental College and Hospital, Khammam, Telangana, India.
3 Senior Lecturer, Department of Periodontics, Mamata Dental College and Hospital, Khammam, Telangana, India.
4 Senior Lecturer, Department of Oral and Maxillofacial Pathology, Sri Sai College of Dental Surgery, Vikarabad, Telangana, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Kotya Naik. Maloth, Senior Lecturer, Department of Oral Medicine and Radiology, Mamata Dental College and Hospital, Giriprasad Nagar, Khammam-507002, Telangana, India. Phone : 91-9885617131, E-mail : dr.kotyanaik.maloth@gmail.com
Oral Lichen planus (OLP) is a common mucocutaneous disorder with a multifactorial aetiology, affecting the women more commonly than men. Most OLP are asymptomatic, except the atrophic and erosive forms.Till date many treatment modalities are implicated to treat this disorder, but no therapy is considered as the single most effective, without side-effects and remission of the lesion. As the treatment of OLP is challenging to the oral practitioners, here we report a case of successful management of extensive, symptomatic bullous and erosive oral lichen planus with a novel treatment protocol- oral minipulse therapy with betamethasone.
Alopecia, Auto-immune disease, Betamethasone, Reticular, Wickham striae
Case Report
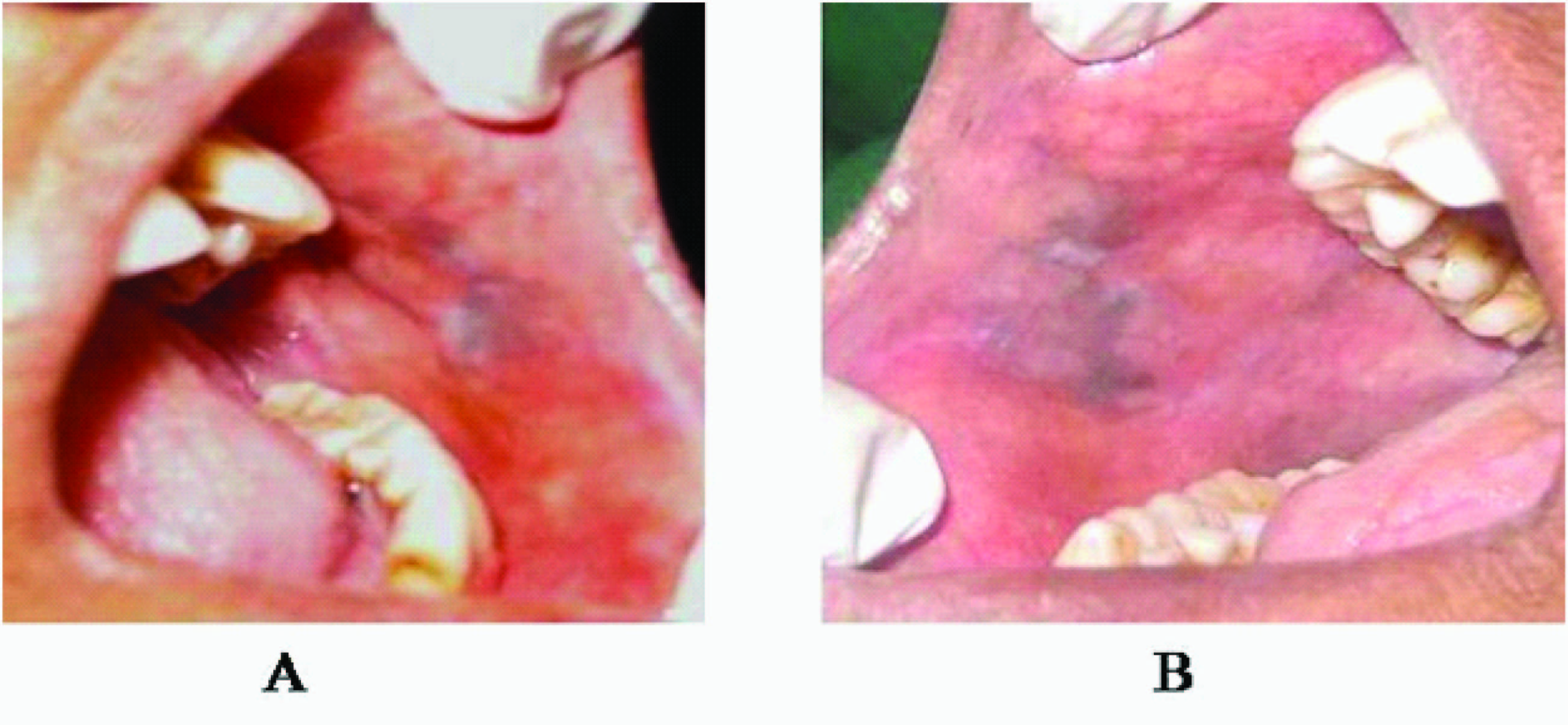
A 35-year-old female patient reported to the department with a chief complaint of burning sensation of the oral cavity since four months. The burning sensation was continuous and preceded by eruption of fluid filled blisters that used to burst with in few seconds. Her medical history was non contributory and on general examination multiple papules were seen on the face and scalp, which were associated with itching and loss of hair on the scalp. Black healed pigmented lesions of varying sizes were also evident on the face [Table/Fig-1&2]. On intraoral examination diffuse white linear striae with areas of erosions and pigmentation were seen on the right and left buccal mucosa [Table/Fig-3]. Fine linear striae and areas of erosions were seen on the right & left lateral borders of the tongue, with intact bullae seen on the left lateral and ventral aspect of the tongue [Table/Fig-4]. Based on the clinical findings, a provisional diagnosis of bullous lichen planus was considered with the differential diagnosis of pemphigus vulgaris and bullous pemphigoid. The patient’s haematological investigations, renal and liver function tests were within the normal limit. Following written informed consent, an incisional biopsy was performed and histopathological report was suggestive of lichen planus.The patient was evaluated and was advised betamethasone oral minipulse therapy comprising 5mg of betamethasone taken as a single daily dose orally for two consecutive days every week for three months, followed by tapering the dose from 5mg to 4 mg in the fourth month, 3mg in the fifth month, and 2mg in the sixth month.Treatment was stopped after six months and patient was followed up for the next three months.The visual analogue scale (VAS) score was recorded on every visit of the patient. Following the therapy there was remission of the lesions on the face, scalp, buccal mucosa and tongue [Table/Fig-5,6,7]. The patient is currently under follow up since 1½ year with no recurrence of the lesions.
Multiple papules and pigmentation on the face

Multiple papules on the scalp with alopecia

Erosions on the buccal mucosa with white straie

Bullous lesions with white straie seen on the lateral border of tongue

Post-treatment picture after 3-months. (A) on left buccal mucosa, (B) on right buccal mucosa and (C) right lateral border of tongue

Post-treatment picture after 6-months. (A) complete remission of the lesion on the face.(B) Complete remission of the lesion on the scalp

Post-treatment picture after 6-months. (A) complete remission of the lesion on the right buccal mucosa.(B) Complete remission of the lesion on the left buccal mucosa
Discussion
Lichen Planus (LP) is a relatively common chronic inflammatory, papulosquamous and presumably autoimmune disease that affects the skin, mucous membranes, nails, and the scalp [1]. The term “Lichen planus” was first introduced by Erasmus Wilson in 1869 [2]. It is derived from the Greek word “leichen”- tree moss and Latin word “planus”- flat [1]. The oral lesions of the disease was first observed by Louis Frederick Wickham and he gave a clear and detailed description of the peculiar striae and dots found on the surface of a lichen planus papule named as Wickham striae in 1895 [3]. Darier gave the first formal description of the histopathologic characteristics of the disease [1]. 0.5-1% of the world’s population and 1-1.5% of Indian population were affected by the lichen planus lesions [4]. It is mostly seen in the 5th and 6th decade of life and has a predominance of women over men [2]. The different aetiological factors considered for LP are genetic background, dental materials, drugs, infectious agent, autoimmunity, immunodeficiency, food allergy, stress, habits, trauma, diabetes, hypertension, malignant neoplasm and bowel diseases [5]. The pathogenesis of LP is thought of from four mechanisms antigen specific cell-mediated immune response (heat shock proteins, CD4+ T-helper cells, CD8+ cytotoxic T-cells) non-specific mechanism (epithelial basement membrane, mast cells, chemokines, matrixmetaloproteinases) autoimmune response, humoral immunity (circulating autoantibodies to desmoglin 1 and 3) [6]. Patients with OLP frequently have concomitant disease in one or more extra–oral sites. Approximately 15% of patients develop cutaneous lesions. The classic appearance of skin lesions described by the six P’s: planar, plaque, pruritic, purple,polygonal, and papular. Typically cutaneous lesions develop after the appearance of oral lesions and severity of oral lesions does not correlate with cutaneous lesions. Lichen planopilaris represents LP involvement of scalp and hair follicles causing a scarring alopecia. The combination of follicular LP with scarring alopecia of scalp and no scarring alopecia of axilla and pubis or other areas is known as Graham Little syndrome. Intra-orally the red and white components of lesion can be part of reticular, papular, plaque-like, atrophic, erosive and bullous types [6]. In the present case the patient presented with reticular, erosive and bullous forms.
The characteristic clinical aspects are sufficient to make a correct diagnosis if classic lesions are present. An oral biopsy with histopathologic study is recommended to confirm clinical diagnosis and also to exclude dysplasia and malignancy. The value of direct immunofluorescence for confirmation of disease is well accepted, especially with non-diagnostic histopathologic features and for desquamative gingivitis [6].
To date no cure for OLP or dermal counterpart. The treatment goal is 2–fold, that is, alleviation of symptoms, monitoring of dysplastic changes [6]. It has a chronic remitting and relapsing course with little tendency for spontaneous remission thereby making management of OLP a challenge for clinicians. Corticosteroids are considered the most effective agents in the treatment of OLP, with topical agents being preferred over systemic drugs except during acute exacerbations [7].
Topical corticosteroids when applied for a short duration are safe, but prolonged use can produce side effects such as secondary candidiasis and rarely, atrophy of the oral mucosa. It is also uncomfortable for the patient to apply medication frequently [8]. Currently, systemic corticosteroids are recommended during acute exacerbations and for persistent erosions, in high dose (Prednisolone 30-80 mg/d) for a short duration (2-3 wk) [7]. However, such regimens are also not free of side effects. To overcome or minimize these limitations without compromising efficacy, the concept of oral minipulse (OMP) therapy was designed. In the form of OMP therapy, corticosteroids have shown efficacy with few and acceptable side effects, in diseases such as vitiligo and alopecia areata [9].
Few studies and case reports revealed the efficacy of betamethasone OMP therapy in lichen planus. Joshi et al., [10] treated a patient suffering from generalized and bullous lichen planus with OMP therapy consisting of 5mg betamethasone orally once daily for two consecutive days in a week and within two weeks he observed that fresh lesions has stopped appearing completely and older lesions subsided rapidly. Mittal et al., [11] conducted a study in ten patients, six males and four females were treated with betamethasone 5 mg orally on two consecutive days in a week for three months. There was an excellent (75-100%) response in six (60%) patients and a good (50-75%) response in four (40%) patients. Al-Mutairi et al., [12] treated acute generalised lichen planus with 5mg betamethasone oral mini pulse therapy for 13 wk. Complete arrest of progression, control of itching and flattening of lesions was achieved within three weeks, followed by tapering of the dose of betamethasone by 0.5 mg every two weeks over the next ten weeks. Malhotra et al., [9] compared the efficacy of 5mg betamethasone OMP therapy orally on two consecutive days per week (group A) with topical triamcinolone acetonide (0.1%) application thrice daily (group B) for a total period of six months in 49 patients with moderate to severe oral lichen planus. A good to excellent response was seen in group A patients, as compared with group B at six months and Rashid et al., [13] compared the efficacy of 5mg betamethasone OMP therapy orally on two consecutive days per week (group A) with loratadine tablet daily (group B) for a total period of six weeks in 40 patients with lichen planus. A complete decrease of the lesion was seen in group A patients, as compared with group B at six weeks.
Above studies found the use of 5mg betamethasone oral mini pulse therapy to be more effective in the treatment of lichen planus with no side-effects during the treatment.
The present case was treated with 5mg betamethasone OMP therapy, orally once daily for two consecutive days in a week for a period of three months followed by tapering the dose for next three months.
The main advantage of OMP therapy is its easy administration without hospital admission, unlike pulse therapy. But the drawback of OMP therapy is that its success depends on patient compliance [8]. In our case, a proper dose schedule was explained to the patient so, that medication is taken without any confusion.
Conclusion
The OLP is a common mucocutaneous disease affecting the heterogeneous group of people with multifactorial aetiology, so as a oral physician identifying and eliminating the various etiological agents associated with the disease is essential. Although various treatment modalities are available for the disease, steroids in topical or in combination with systemic form considered as gold standard treatment modality for the disease. This case provides further evidence that OMP therapy improves the clinical outcome in patients with moderate to severe oral lichen planus and though the treatment was equally effective as topical triamcinolone acetonide, the response is earlier, especially in erosive and bullous forms of the disease.
[1]. Gupta SB, Chaudhari ND, Gupta A, Talanikarint HV, Lichen planus – An updateJ Pharm Biomed Sci 2013 4(2):59-65. [Google Scholar]
[2]. Rajendran R, Oral Lichen planusJ Oral MaxillofacPathol 2005 9:3-5. [Google Scholar]
[3]. Wickham L, F. Sur un signepathognomiquedelichen du Wilson (lichen plan) stries et punctuations grisatres Ann Dermatol Syph 1895 6:17-20. [Google Scholar]
[4]. Daoud MS, Pittelkow MR, Lichen PlanusIn: Fitzpatrick’s dermatology in general medicine. Eds. Freedberg IM, Eisen AZ, Wolf K, Austen KF, Goldsmith LA, Katz SI 2003 6th EdnMcGraw Hill Publication:463-77. [Google Scholar]
[5]. Roopashree MR, Gondhalekar RV, Shashikanth MC, George J, Thippeswamy SH, Pathogenesis of oral lichen planus-a reviewJ Oral Pathol Med 2010 39:729-34. [Google Scholar]
[6]. Patil A, Prasad S, Ashok L, Sujatha GP, Oral bullous lichen planus: Case report and review of managementContemporary Clinical Dentistry 2012 3(4):344-48. [Google Scholar]
[7]. Mollaoglu N, Oral lichen planus: a reviewBr J Oral Maxillofac Surg 2000 38:370-77. [Google Scholar]
[8]. Premkumar Oral Mini Pulse Therapy: Report of A Case and Review of the LiteratureOHDM 2013 12(2):112-18. [Google Scholar]
[9]. Malhotra AK, Khaitan KB, Sethuraman G, Sharma VK, Betamethasone oral minipulse therapy compared with topical triamcinolone acetonide (0.1%) paste in oral lichen planus: A randomized comparative studyJournal of American Academy of Dermatology 2008 58:596-602. [Google Scholar]
[10]. Joshi A, Khaitan KB, Verma KK, Sing Generalised and bullous lichen planus treated successfully with oral mini-pulse therapyIndian Journal of Dermatology Venereology Leprology 1999 65:303-304. [Google Scholar]
[11]. Mittal R, Manchanda Y, Lichen planus treated with betamethasone oral mini pulse therapyIndian Journal of Dermatology Venereology Leprology 2000 66:34-35. [Google Scholar]
[12]. Al-Mutairi N, Joshi A, Zaki A, Sharma AK, Nour-Eldin O, Acute generalized lichen planus treated with weekly betamethasone 5-mg oral mini-pulse therapyJournal of Drugs Dermatology 2005 4:218-220. [Google Scholar]
[13]. Rashid MM, Khan AU, Sikder A, Ali E, Akhtar N, Betamethasone oral mini-pulse therapy in the treatment of lichen planusIran Journal of Dermatology 2008 11:99-102. [Google Scholar]