Prescribing Pattern of Anti-malarial Drugs with Particular Reference to the use of Artesunate in Complicated Plasmodium Vivax Cases
Ashutosh Kumar Singh1, Mohd Sajid Khan2, Farhan Ahmad Khan3
1 Assistant Professor, Department of Pharmacology, Gold Field Institute of Medical Science & Research Centre, Faridabad, India.
2 Assistant Professor, Department of Pharmacology, Gold Field Institute of Medical Science & Research Centre, Faridabad, India.
3 Associate Professor, Department of Pharmacology, Teerthanker Mahaveer Medical College & Research Centre, Moradabad, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Farhan Ahmad Khan, Associate Professor, Department of Pharmacology, Teerthanker Mahaveer Medical College & Research Centre, Delhi Road, Moradabad-244001, U.P, India. Phone : 9759468300, E-mai : Dr.farhan.k@gmail.com
Background: In developing countries, Malaria has been found to be one of the most common cause of fever and morbidity, particularly among infants and young children. Therefore, its drug utilization studies should be carried out to know the rationality of treatment.
Aim: To evaluate the use of antimalarial agents in children with a diagnosis of Malaria and visited to OPD & IPD Paediatric department of a tertiary care teaching hospital.
Materials and Methods: This was a prospective six months study based on a Medication Utilization Form, which has been designed in consultation with the paediatrician. One hundred eighty three children <12 y of age were selected on the basis of inclusion and exclusion criteria.
Results: Out of 183 patients, 110 were infected with Plasmodium falciparum (60.10%) and 73 with Plasmodium vivax (39.89%). Most of the patients were male, 56.83% and 43.16% were female patients. Most of the complicated cases were found from Plasmodium falciparum (n = 110) than Plasmodium vivax (n=15). In prescriptions with monotherapy, Artesunate (n=101) was found to be the most commonly prescribed drug and in prescriptions containing more than one drug, Artesunate – lumefantrine (n=125) combinations were frequently used. Most of the drugs were prescribed by oral route (n=285), than the parenteral route (n=140). The average number of drugs per encounter was 2.32 and only 4.50% drugs were prescribed by generic name. Average drug cost per prescription in complicated cases was found to be higher (185.5 INR) than uncomplicated cases (115 INR).
Conclusion: Artemisinin were used as first line drugs irrespective of the causative agent for malaria, which is not recommended, however has been found to be effective in complicated cases of Plasmodium vivax also. The cost of the prescription was higher. Interventions to rectify over prescription of injectables necessary to further improve rational drug use in our facility. Also, there should be an awareness program, especially in slum areas to cut down the transmission of disease.
Artesunate, Drug utilization study, Essential drugs, Lumefantrine, Malaria
Introduction
Malaria is a mosquito-borne infectious disease of humans and other animals caused by a parasite called Plasmodium, which is transmitted via the bites of infected mosquitoes. Malaria causes symptoms that typically include fever, fatigue, vomiting and headaches. In serious cases it can cause yellow skin, seizures, coma or death [1].These symptoms usually begin ten to fifteen days after being stung.
Granting to the World Health Organization (WHO), instances of malaria rising worldwide year by year [2]. Approximately 1.5 million occur in India [2].
The cases of malaria appear to be growing in those areas where malaria control has declined lead to the increase risk of transmission, increasing prevalence of drug-resistant strains of parasites (e.g. Chloroquine resistance) and in a relatively few cases, because of increasing international travel. Although the majority of instances of malaria worldwide are mild and can be handled with oral drugs, but in some instances where there is a delay in diagnosis or treatment, may produce complicated, life-threatening disease requiring parenteral therapy. These cases may present with prostration, any impairment of consciousness, convulsions or any manifestation of shock, decreased urinary output, respiratory distress or abnormal bleeding.
P. Falciparum is mainly responsible for virtually all the severe cases and deaths. The other species, P. vivax, P. ovale and P. malarial, cause mainly a febrile illness and only rarely lead to severe disease [3]. Most of the complicated patient presents with Cerebral malaria.
Children often present with convulsions (sometimes recurrent). They may exhibit flaccid muscle tone and abnormalities of the brainstem reflexes (oculocephalic, oculovestibular, pupillary and corneal).These manifestations probably result from raised intracranial pressure which appears to be an important feature in cerebral malaria in children rather than in adults. As the instances of malaria in children are more eminent in our region, so it was necessary to do a drug utilization study on anti-malarials prescribed. Evenly, we know that Drug utilization studies aims to evaluate factors that are tied up to the prescribing, dispensing, administering and taking of medication, and its associated events [4]. Our work also aims at to analyse the drugs prescribed in children suffering from malaria and also to split down the influence of malaria on the socioeconomic status of patients.
Materials and Methods
Setting
This prospective study was carried out in the OPD & IPD Paediatric department of the Teerthanker Mahaveer Medical College, a tertiary care teaching hospital in the northern part of India.
Study design
This was a prospective study and was based on a Medication Utilization Form. The present study followed some WHO/INRUD indicators in addition to some other useful indicators [5]. It included patient particulars, diagnosis, anti-malarial drugs details. The information was compiled and analysed in consultation with a paediatric specialist.
Duration of study
The duration of study was 6 months (Aug 2013 to Jan 2014). The study was approved by the Institutional Ethical Committee. An oral and written consent was obtained from the patients before their participation in the study.
Study population
The present study was conducted on 183 patients aged less than 12 y suffering from Malaria who visited the OPD and IPD of Paediatric department during the 6-month period. The patients were enrolled on the basis of inclusion and exclusion criteria.
Results
During the six month study period, 183 patients (<12 y) were enrolled on the basis of inclusion & exclusion criteria. Out of 183, 56.83 % (n=104) were male patients and 79 (43.16%) were female patients [Table/Fig-1]. Most of the patients were from 8-12 y (n=97) age group, followed by 4-8 y (n=78) age group and least in 2-4 y age group (n=8) [Table/Fig-1]. The incidence of Malaria was found more in Non-School going (n=102) than School going children (n=81). [Table/Fig-1]. Also cases of Malaria were found more in children belonging to rural area (n=112) than urban areas (n=71) [Table/Fig-1].
Demographic characteristics of the patients
| Variables | No. of Patients (n=183) |
| Male | 104 |
| Female | 79 |
| Total | 183 |
| Age (years) wise distribution |
| 2-4 | 8 |
| 4-8 | 78 |
| 8-12 | 97 |
| School going/ Non-School going |
| School going | 81 |
| Non-school going | 102 |
| Variables | No. of Patients (n=183) |
| Area |
| Rural | 112 |
| Urban | 71 |
| OPD/IPD | |
| Treated in OPD only | 58 |
| Treated in IPD only | 125 |
| Routes of drug administration (425) |
| Oral | 285 |
| Parenteral | 140 |
Most of the patients were found to be infected with Plasmodium falciparum (n = 110, 60.10%) than Plasmodium vivax (n = 73, 39.89%) as shown in [Table/Fig-2].
Pattern of uncomplicated and complicated malarial parasite infection
| Cases | Clinical diagnosis | Total |
|---|
| P.falciparum (n=110) | P.vivax (n=73) |
|---|
| Uncomplicated | - | 58(100%) | 58 |
| Complicated | 110 (88%) | 15 (12%) | 125 |
| Total | 110 | 73 | 183 |
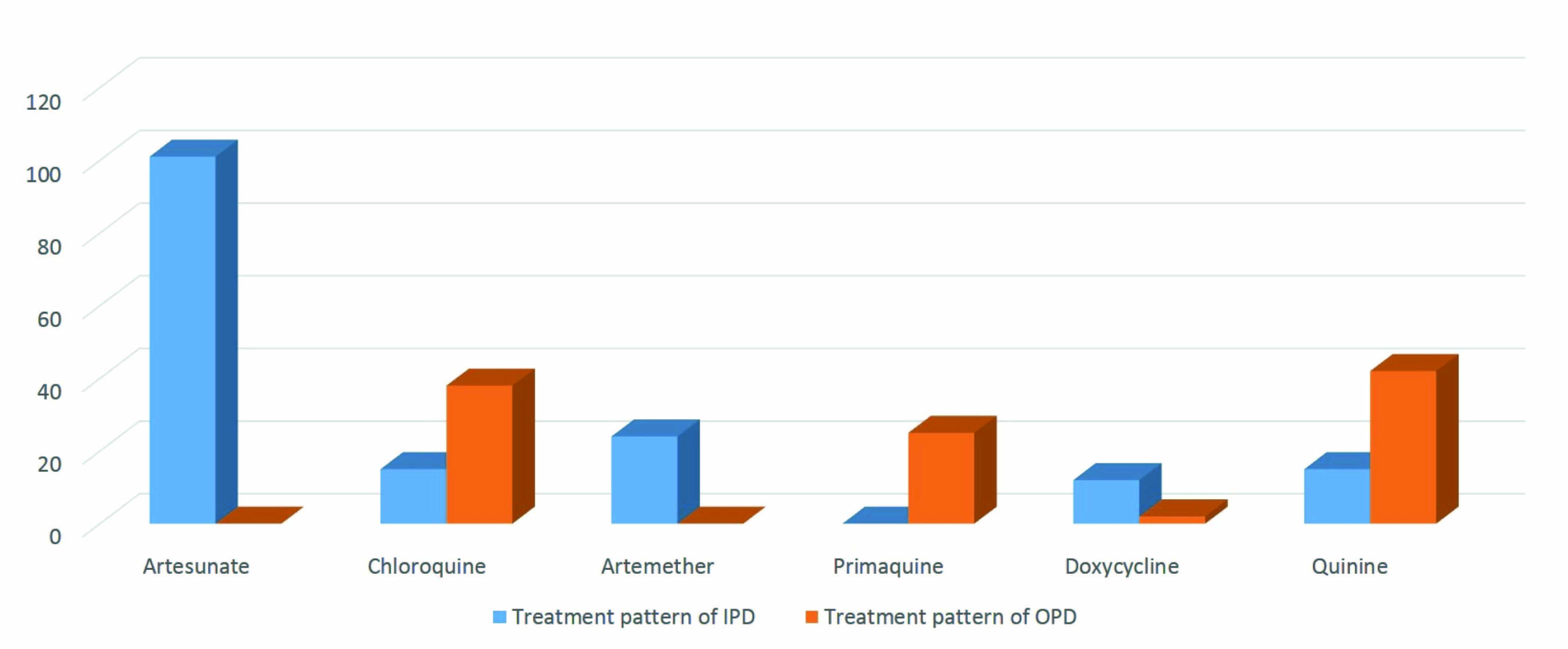
Highest number of complicated cases were found in patients infected with Plasmodium falciparum (n = 110), admitted in IPD department, whereas patients affected with Plasmodium vivax have only n=15 patients that presented as Complicated case [Table/Fig-2]. Whereas most of the cases of P.vivax treated only in OPD [Table/Fig-3]. All the complicated cases of Plasmodium falciparum were admitted in IPD department. Complicated vivax malaria was treated like falciparum malaria using artemisinin based combination therapy (ACT) [Table/Fig-4].
Prescribing pattern of antimalarials in OPD & IPD patients (n=183)
| Drugs | Treatment pattern of IPD Complicated cases P.falciparum n=110 P. vivax n=15 | Treatment pattern of OPD un Complicated cases P.vivax n=58 | Total N=274 |
|---|
| Artesunate | 101(100%) | - | 101 |
| Chloroquine | 15 (28.30%) | 38 (71.69%) | 53 |
| Artemether | 24 (100%) | - | 24 |
| Primaquine | - | 25 (100%) | 25 |
| Doxycycline | 12 (85.71%) | 2 (14.28%) | 14 |
| Quinine | 15 (26.31%) | 42 (73.68%) | 57 |
| Total | 167(60.94%) | 107(39.05%) | 274 |
Drug utilization on the basis of WHO indicator
| Indicators | Variables |
|---|
| Average no. of drugs per prescription | 2.32 |
| Percentage of drugs prescribed by generic name | 4.50% |
| Number of encounters resulting in prescription of an injection | 32.94% |
| Average drug cost per encounter in complicated cases | 185.5 INR |
| Average drug cost per encounter in uncomplicated cases | 115 INR |
Most of the drugs were prescribed with oral route (n=285, 67.05%), than the parenteral route (n=140, 32.94%) [Table/Fig-1,5].
Prescribing pattern of anti-malarials
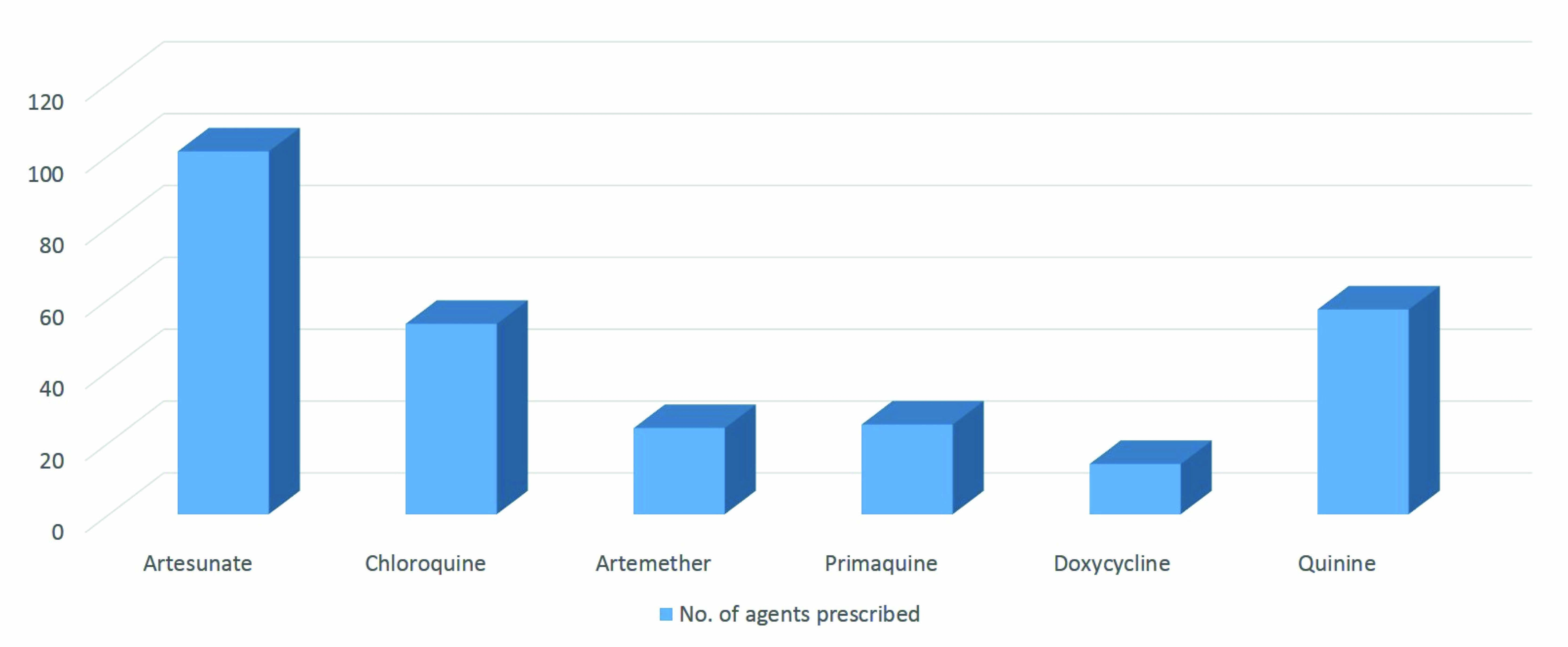
Artesunate (n=101) was found to be the most commonly prescribed drugs followed by Quinine (n=57), Chloroquine (n=53), Primaquine (n=25), Artemether (n=24) [Table/Fig-3,6]. Artemisinin resistance was seen in 14 cases where Doxycycline was prescribed and showed good results [Table/Fig-3,6]. [Table/Fig-3] also depicts, prescribing patterns according to type of Malaria and OPD/IPD treatment. In IPD with most of the Plasmodium falciparum infected patients and less number of P. vivax cases (n=15), Artesunate (n=101) was the most commonly prescribed agent, followed by Artemether (n=24), Quinine (n=15), Chloroquine (n=15), and Doxycycline (n=12). Whereas the majority of patients suffered from P. vivax infection treated in OPD only (n=58), and were given Quinine (n=42), followed by Chloroquine (n=38), Primaquine (n=25) and Doxycycline (n=2) [Table/Fig-3]. In patients with complicated malaria Artesunate (n=101), Artemether (n=24) were administered for first 3-5 d as an injectable form followed by oral formulation. In combination of drugs, most common combination prescribed by the doctors was Artesunate – lumefantrine (n=125), followed by Artesunate – mefloquine (AS/MQ) (n=18), and least prescribed was the combination of Artesunate +sulfadoxine + pyrimethamine (AS/S/P) (n=8), [Table/Fig-7].
Prescribing pattern of anti-malarials in OPD/IPD patients
Multidrug regimen (n=183)
| Drugs | Number (%) |
|---|
| Artesunate +mefloquine (AS/MQ) | 18(11.92%) |
| Artesunate +sulfadoxine + pyrimethamine (AS/S/P) | 8 (5.29%) |
| Artesunate+lumefantrine | 125 (82.78%) |
| Total | 151 |
It was observed that out of the 425 drugs which were prescribed to the patients, only 19 (4.50 %) were of the generic form [Table/Fig-4]. Average drug cost per prescription in complicated cases was found to be higher (185.5 INR) than uncomplicated cases (115 INR) [Table/Fig-4].
Our results revealed that Plasmodium falciparum was more prevalent than P. vivax in this area. Also the percentage of cases presenting as complicated case were mainly from Plasmodium falciparum infection.
Discussion
Approximately 80% of India’s population live in malaria risk areas [2]. Our area also comes under endemic region for Malaria as confirmed by the number of cases (n=183) reported during the six month study period. Most of the patients were found to be infected with Plasmodium falciparum (n=110). This is in accordance with Kumar A et al., that there is a rampant rise in the proportion of Plasmodium falciparum in India, the more deadly parasite, rising from 44% of all confirmed cases in 2005 to 54% in 2009 [6], and it may soon reach 59% [7].
Kumar A et al., also found that in spite of a rise in malaria cases, India is making really slow progress regarding control of malaria in comparison to other countries [7]. As suggested by higher number of cases found in our study. There are also other reasons for higher number of cases in our study as our hospital is closer to rural areas as compared to urban areas. Also, most of the villages are nearer to rivers which get full by the time of the rainy season.
Earlier Malaria was considered as a disease of rural areas but now malaria is spreading in urban population also [8,9]. May be associated with construction activity and migrant workers. Our study also supports this data as 38.79% of our cases were belongs to urban areas [Table/Fig-1].
In this study the use of Artemisinin-based Combination Therapy (Artesunate n=101, Artemether n=24) was comparatively more than chloroquine (19.34% vs. 18.51%) as monotherapy and, this corresponds well with the national drug policy on malaria, 2007 guidelines [10], However the guidelines also state that ACT should be given only to confirmed Plasmodium falciparum cases found positive by microscopy or Rapid Diagnostic kits [10]. We found that this was not followed in many of the cases, and patients with P. Vivax infection also received ACT. In our study Primaquine was not prescribed in children affected with P. Falciparum as suggested by guidelines, where its use is not needed, as the parasite does not have a hepatic stage [11]. Whereas in the similar study conducted in another part of India by Mubeen F, et al., noticed increased prescription of primaquine to all the patients, including those suffering from Plasmodium falciparum [12].
We know that Artemisinin-derivatives are highly efficacious against multidrug-resistant Plasmodium falciparum malaria. But, we recently found that Artesunate as a monotherapy and in combination with sulfadoxine-pyrimethamine to be highly effective (98%) in Complicated cases of Plasmodium vivax (n=15) also. Our findings are in accordance with Tjitra E, et al., that also showed good efficacy of ART in Plasmodium vivax cases [13]. We used modified World Health Organization criteria to evaluate the efficacy of ART-SP for the treatment of vivax malaria in our region and found useful. Another reason for using Artesunate in Vivax cases as Artemisinin-based combination therapy (ACT) may slow the development of resistance and reduce malaria transmission [14].
Most of the drugs were prescribed by brand names. This is mainly because of the fact that doctors are often influenced by the drug companies for prescribing drugs and the patient who is at the receiving end of the spectrum bears the cost of the expenditure and the inappropriate medical treatment most of the time.
Also, Average drug cost per prescription in complicated cases was found to be higher (185.5 INR) than uncomplicated cases (115 INR)[Table/Fig-4]. This may be because of the high use of injectable in complicated cases. Also the duration of treatment is higher in complicated cases.
Therefore, with the help of drug utilization research, we can facilitate the rational use of drugs in populations.
Conclusion
Our region is more endemic for Plasmodium falciparum malaria than for P. vivax and there is an emergence of chloroquine resistant Plasmodium falciparum malaria also. Our study shows that first-line therapy for falciparum malaria was in accordance with the guidelines. The only irrationality seen was the use of Artemisins in patients of P. vivax as per the WHO guidelines, but the results were good. Use of artemisinin should be rational. Our study pointed out that the incidence of Malaria was more in children from rural area as well as in non-school going children. There should be an awareness program, especially in slum areas. May be that will cut the transmission of Malaria. Also, the less number of drugs were prescribed by generic name. These results should inform the education of health professionals and rational drug use policies to emphasize on rational prescribing. Although the average number of drugs prescribed per prescription was within the limits, but the number of drugs prescribed with generic name was very low.
[1]. WHO. March 2014. Retrieved 28 August 2014 [Google Scholar]
[2]. Caraballo H, "Emergency department management of mosquito-borne illness: malaria, dengue, and west nile virus"Emergency Medicine Practice 2014 16(5) [Google Scholar]
[3]. WHO: World Malaria Report. Geneva, Switzerland: World Health Organization; 2011 [Google Scholar]
[4]. WHO: World Malaria Report. Geneva, Switzerland: World Health Organization; 2010 [Google Scholar]
[5]. Sjoqvist F, Birkett D, Drug Utilization, in Introduction to Drug Utilization Research 2003 WHO publications:76-84. [Google Scholar]
[6]. Kumar A, Chery L, Biswas C, Dubhashi N, Dutta P, Dua VK, Malaria in South Asia: prevalence and controlActa Trop 2012 121:246-55. [Google Scholar]
[7]. Kochar DK, Saxena V, Singh N, Kochar SK, Kumar SV, Das A, Plasmodium vivax malariaEmerg Infect Dis 2005 11:132-34. [Google Scholar]
[8]. Gama H, Drug utilization studiesArquivos De Medicina 2008 22(2):69-74. [Google Scholar]
[9]. Sharma VP, Re-emergence of malaria in IndiaIndian J Med Res 1996 103:26-45. [Google Scholar]
[10]. Sharma VP, Battling malaria iceberg incorporating strategic reforms in achieving millennium development goals & malaria elimination in indiaIndian J Med Res 2012 136:907-25. [Google Scholar]
[11]. Guidelines for the diagnosis and treatment of malaria in India. National Institute of Malaria Research (NIMR) and National Vector Borne Disease Control Programme. 2009;3-17 [Google Scholar]
[12]. Mubeen F, Pandey DK, Jaheer M, Drug Utilization Pattern Of Antimalarial Drugs At A Tertiary Care Hospital: A Retrospective StudyIJMPS 2012 3(5):01-05. [Google Scholar]
[13]. Tjitra E, Baker J, Suprianto S, Cheng Q, Anstey NM, Therapeutic efficacies of artesunate- sulfadoxine- pyrimethamine and chloroquine-sulfadoxine-pyrimethamine in vivax malaria pilot studies: relationship to Plasmodium vivax dhfr mutationsAntimicrob Agents Chemother 2002 46(12):3947-53. [Google Scholar]
[14]. White NJ, Olliaro PL, Strategies for the prevention of antimalarial drug resistance: rationale for combination chemotherapy for malariaParasit Today 1996 12:399-401. [Google Scholar]