Minor oral surgical procedures are routinely carried out under local anaesthesia. However, favourable conditions for the operator and patient are seldom achieved. The feeling of fear and anxiety is not a unifactorial entity but is an emotional state, which has a direct pertinence on the psychological and physiological make up of an individual. Factors such as apprehension and poor motivation need to be considered while carrying out minor oral surgical procedures [1].
In routine practice we do not encounter certain circumstances which do not empower the practitioner to use general anaesthesia nor is it advisable to carry out the procedure under local anaesthesia alone. The technique of anaesthesia in the form of “conscious sedation” has been developed to overcome the drawbacks of operating under local anaesthesia alone and to avoid the risks associated with general anaesthesia [1].
We proposed to use two sedative agents independently (Propofol and Midazolam: both these drugs have similar sedative efficacy, with propofol a faster onset of action and rapid recovery) along with local anaesthesia and compared the results to those patients undergoing the surgical removal of impacted third molars under local anaesthesia alone.
The aims and objectives of the study were to compare vital parameters during impacted third molar removal under local anaesthesia, with or without sedative agents. The study conducted with the aim to study following objectives.
Materials and Methods
For standardization of the sample, we used the following clinical criteria: 1) age between 18 and 50 y (ASA I and II), 2) impacted third molars in the horizontal position (Winter’s classification), Class II and position B, according to the Pell and Gregory classification, 3) a single experienced surgeon has performed the surgical procedure. Exclusion criteria were: patient’s refusal for consent, bleeding disorder, patients allergic to the study drugs, uncontrolled hypertension, pregnancy, ischemic heart disease, hepatic or renal disorders, patients with gastro-esophageal reflex, morbid obesity, reactive airway disease, a history of nasopharyngeal surgery or drug abuse and a long term use of sedatives.
Ninety patients having impacted third molars undergone the surgical removal were divided into three groups of 30 volunteers each at Bharati Vidyapeeth Dental College and Hospital, Pune from June 2005 to December 2007. In Group A: 30 patients (Propofol along with Local anaesthesia); Group B: 30 patients (Midazolam along with Local anaesthesia); Group C: 30 patients (Local anaesthesia only). All the patients undergone for routine blood and urine analysis, RBS, HIV, HBsAg, Electrolytes-Na; K, along with chest x-ray and the patients included in our study shown the normal reports. The proposed study was clinically oriented with active involvement of patients with informed written consent being obtained from them before their inclusion in trial study with the approval from ethical committee. The procedure was explained to them regarding the nature and benefit of the study. Instructions were given to the patients to remain nil by mouth for 4-6 h prior to the procedure. No premedication were given to any of the patients.
Preoperative baseline vital signs (SpO2, Pulse rate, and Blood pressure) of all patients were recorded 10 min before the procedure and thereafter every 5 min. Vital signs (SpO2, Pulse rate, and Blood pressure) were recorded for 10 min after conclusion of the procedure and were recorded by the individual conducting the study.
All patients were operated in an operation theatre and were monitored by an anaesthesiologist during the procedure. All facilities for securing and maintaining a patent airway, providing O2, artificial ventilation and cardiopulmonary resuscitation were available. All patients were breathing spontaneously and received 3 L/min oxygen supplementation if there was hypoxia/apnea while monitored with pulse oximeter and noninvasive blood pressure (NIBP).
At this point, patients were randomly assigned by a concealed envelope method into one of three groups (each group had 30 patients); in the propofol group (Group A) an infusion pump with IV doses of Propofol (20 μg/kg/min) to maintain a constant level of anaesthesia closer to "conscious” sedation. In Midazolam (Group B), 1.5 mg initial dose IV then titrate, give over 2 minutes; wait 2 min after each dose: max total dose of 5 mg. Local anaesthesia was administered following the administration and initiation of the effect of sedative agents (30 sec after administration of propofol and 3 min after the administration of midazolam). Administration of sedative agents was ceased immediately following conclusion of procedure. Average procedure time for the removal of impacted third molar was one hour. However, we have not included the procedure time in our study.
The ideal sedation scale should provide a data that are easy to calculate and record, precisely describe the degree of sedation or agitation within well-defined categories, guide the titration of therapy, and have validity and reliability in the patients. Various scales are existing but not a single scale provides all the necessary information [2]. The aim to measure a patient’s sedation level may be helpful in very deep sedation or under therapeutic neuromuscular blockade. BIS (Bispectral Index) is probably useful in deep comatose or under neuromuscular blockade, however, routine use of this device cannot recommend until the value and validity is confirmed.
However, sedation level was assessed by using the Ramsay scale in our study because it had shown to reduce the duration of mechanical ventilation and length of stay [3,4] Score 1 = Anxious or restless or both, Score 2 = Cooperative, oriented and tranquil (calm), Score 3 = Responding to command, Score 4= Brisk (quick) response to stimulus, Score 5= Sluggish (slow moving) response to stimulus, Score 6 = No response to stimuli.
Operator’s comfort was evaluated by Co-operation of the patient at the end of the surgery by two distinct parameters. The first one was according to the bleeding in the surgical field (Grade 1: bloodless field not hampering the surgery; Grade II: mild bleeding requires occasional suction; and Grade III: excessive bleeding hampers the surgery in spite of suction) and the second one was according to the movement of the patient and unavoidable talking.
All patients treated using sedative agents were kept indoors under medical supervision for a minimum period of 2 h following conclusion of procedure. Patients’ satisfaction was recorded postoperatively for all patients. A questionnaire, to rate the overall pain experience for all patients was done (0 = no pain; 1 = mild; 2 = moderate; or 3 = severe) and their degree of overall satisfaction with the management of their pain (0=poor; 1= adequate; 2= good; or 3= excellent) after the procedure [4].
Duration of recovery (Modified post-anaesthesia discharge scoring system) [5]:
Vital signs- 2: within 20% of preoperative value, 1: 20-40% of preoperative value, 0: 40% of preoperative value.
Ambulation and mental status-2: steady gait/ no dizziness, 1: with assistance, 0: no ambulation/ dizziness.
Nausea/ vomiting- 2: minimal, 1: moderate, 0: severe.
Pain- 2: minimal, 1: moderate, 0: severe.
Bleeding- 2: minimal, 1: moderate, 0: severe.
Results
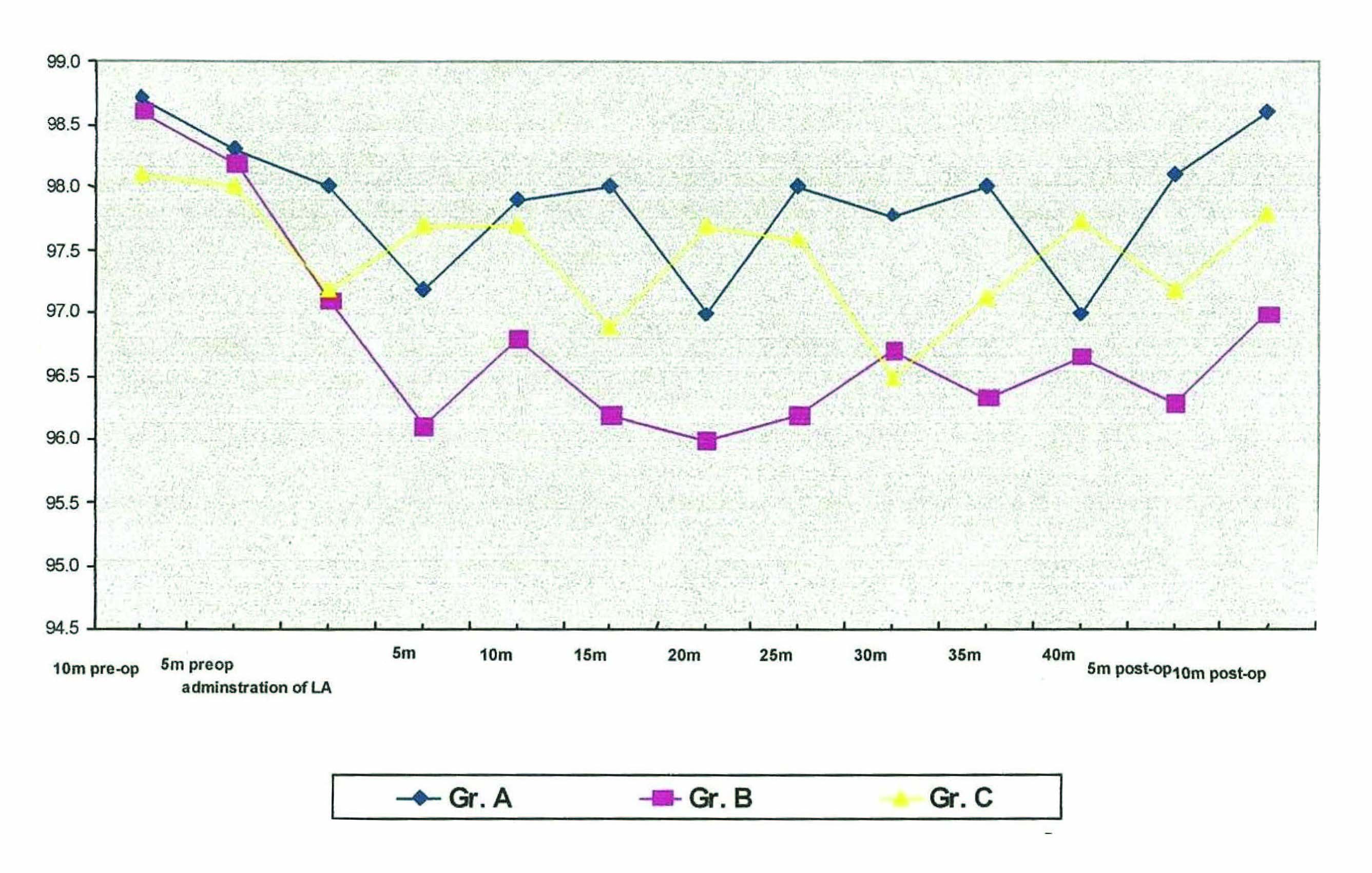
Ninety patients were recruited for this study (30 in each group). There were no statistically significant differences between the three groups regarding to age, sex, body weight, as well as duration of surgery. Oxygen saturation, pulse, systolic and diastolic blood pressure were comparable among the groups and during all recorded times [Table/Fig-1,2,3,4].
Comparison of SpO2 at various time intervals
Comparison of pulse at various time intervals

Comparison of Systolic Blood Pressure at various time intervals

Comparison of Diastolic blood pressure at various time intervals

All patients showed a decrease in the intraoperative plasma oxygen saturation during the surgical removal of impacted third molar was performed. Lowest oxygen saturation with propofol group was 97%, midazolam 96% and local anaesthesia 96.5% intraoperatively. Although propofol, midazolam and local anaesthesia showed a tendency to reduce oxygen saturation from 10 minute preoperative value, midazolam had a marked effect in this regard [Table/Fig-1].
In all the three groups ten minute preoperative records showed an average pulse rate of 80 beats/ min. Both midazolam and local anaesthesia group the pulse rate was increased and reached 120 beats/min during procedure. In the propofol group it remained equivalent to the preoperative value. Ten minutes postoperatively the pulse rate of the patients was at higher level in midazolam (96 beats/min) and local anaesthesia (92 beats/min) group as compared to the propofol group (82 beats/min) [Table/Fig-2].
Average blood pressure of all patients at ten minutes preoperative was 124/82 mmHg. Blood pressure during the procedure was increased and reached at 138/90mm Hg in local anaesthesia group while in midazolam and propofol group it was decreased and reached 116/78 mmHg. Thus both the systolic and diastolic blood pressure in propofol and midazolam group remained similar without much significant changes to the baseline level as compared to local anaesthesia alone. Ten minutes postoperatively the blood pressure remained equivalent to preoperative value (124/82 mmHg) in propofol and midazolam group while it was at higher level in local anaesthesia group (134/84mmHg) [Table/Fig-3&4].
Operating surgeon had commented that the operating conditions during the procedure were comparatively better in propofol group as compared to midazolam group and local anaesthesia group. In midazolam it was due to drowsiness and in local anaesthesia group it was due to anxiety [Table/Fig-5].
| Propofol (Group A) N=30 | Midazolam (Group B) N=30 | LA (Group C) N=30 |
|---|
| Grade 1 | 16 (53.33%) | 12 (40%) | 05 (16.66%) |
| Grade 2 | 13 (43.34%) | 13 (43.34%) | 16 (53.34%) |
| Grade 3 | 01 (3.33%) | 05 (16.66 %) | 09 (30%) |
Patients’ satisfaction was recorded post-operatively after the questionnaire to them regarding the pain experience during the surgery and the data suggested that patients in Group A had more satisfaction compared to Group B and Group C [Table/Fig-6].
| Propofol (Group A) N=30 | Midazolam (Group B) N=30 | LA (Group C) N=30 |
|---|
| Excellent | 23 (76.66%) | 13 (43.34 %) | 03 (10 %) |
| Good | 06 (20 %) | 05 (16.66 %) | 07 (23.34 %) |
| Adequate | 01 (3.34 %) | 09 (30 %) | 14 (46.66 %) |
| poor | 0 (0 %) | 03 (10%) | 06 (20 %) |
None of patients among the groups studied had experienced any form of allergic reaction and had required mechanical ventilation because patient’s sedation level was under control yet we had not compared in our study.
Nausea was present in 9 patients with midazolam group while in local anaesthesia and propofol group no patient reported nausea. Vomiting was present in 3 patients with midazolam group, 1 with propofol group while there were no patients had been reported with local anaesthesia group. Confusion and giddiness was present in propofol group in 1 patient, midazolam 17 patients and in local anaesthesia 2 patients. Pain on arm was found in propofol group in 9 patients while in midazolam only 1 patient.
All (N=30) patients in propofol group recovered from sedative effects completely within 2 hours while in midazolam group (N=30) recovery was not complete in 14 of 30 patients even after 2 h following completion of the procedure.
Discussion
Fear, anxiety and pain are common reasons for patients to delay dental care. In addition to these factors, apprehension and poor motivation are responsible for fluctuations in parameters such as plasma oxygen saturation (SpO2), pulse rate and blood pressure. Sedation in combination with local anaesthesia is being increasingly used as an alternative to local anaesthesia alone for control of perioperative pain and anxiety in oral surgery.
Intravenous midazolam by A. Richards [6] in doses of 0.07 – 0.1 mg/kg has been recommended according to the anxiety level. Intravenous propofol in sedative doses was 10-50μg/kg/min by Joseph E Cilio [7] and 35μg/kg/min by Chandra R [8]. Local anaesthesia was administered following the administration and initiation of the effect of sedative agents (30 sec after administration of propofol and 3 min after the administration of midazolam). Administration of sedative agents was ceased immediately following conclusion of procedure. Midazolam was administered every 10 min whereas propofol was administered every 5 min.
In our study, although propofol, midazolam and local anaesthesia showed a tendency to reduce oxygen saturation, midazolam had a marked effect in this regard. Clinically no patients had shown any signs of hypoxia [Table/Fig-1]. John H. Hardeman [9] concluded that the use of supplemental oxygen administration in the recovery room can significantly reduce the hypoxic episodes and avoid any related complications. Stokes and Hutton [10] were able to demonstrate a lower incidence of apnea in patients who received slow induction doses of sedative agents compared with patients who received a rapid induction dose. M. R. C. Rodrigo and J. B. Rosenquist [11] found after studying a randomized cross-over study with 32 healthy patients, between the ages of 18 and 40 y who had undergone for bilateral symmetrically impacted lower third molar surgery at the rate of 1 mg/min with midazolam, no significant desaturation attributable to midazolam sedation was observed.
Blood pressure and pulse rate were measured in our study was every 5 min starting 10 min preoperatively and continued upto 10 min postoperatively. The result of the study [Table/Fig-1–4] clearly shows the effect of midazolam, propofol and local anaesthesia alone on the cardiovascular system. It is evident from the values that all the three drugs cause certain changes on the pulse rate and blood pressure during procedure. Throughout the study, the systolic and diastolic blood pressure in patients undergoing minor oral surgery using sedative agents remained almost unchanged compared to patients with local anaesthesia alone. The pulse rate of the patients was at higher level in Group B (Midazolam) and Group C (Local anaesthesia) than Group A (Propofol). Dionne RA and Goldstein DS [12] found that when lidocaine with epinephrine was administered for third molar removal, systemic epinephrine levels increased approximately fivefold in a group of patients who did not receive concomitant sedation and eightfold in a group that did receive sedation. Although the primary event that occurs at the site of injection beneath the oral mucosa is vasoconstriction, the relatively low systemic levels achieved after lidocaine with epinephrine can cause increases in pulse rate and systolic blood pressure, yet actually reduce diastolic blood pressure. Joseph E Cilio [7] found that midazolam at equal sedation levels produced more respiratory depression than propofol.
Nausea, confusion, giddiness and pain at injection sites were common with sedative agents. In the midazolam group the side effect of drowsiness, confusion persisted even after 2 h in 17 patients. Nausea was not found in Group A (Propofol) and Group C (Local anaesthesia). Vomiting was there in three patients in midazolam group compared to one patient in propofol. Pain on arm was found in propofol group in 9 patients while in midazolam only one patient. Except giddiness in two patients there were no other complications with local anaesthesia group. Thus, the side effects of the study drugs were higher with Group B (Midazolam).
Conclusion
The study was designed to assess the effect on physiological parameters during the surgical removal of impacted third molar using local anaesthesia alone or with sedative agents (Propofol and Midazolam). The advantages of propofol (Group A) reflected over midazolam (Group B) and local anaesthesia alone (Group C) on most measures including vital parameters, anxiolysis, operator’s comfort and patient’s satisfaction. Recorded data evaluated provided a greater insight into the use of sedative/ anxiolytic drugs in routine minor oral surgical procedures in terms of statistical significance in all the parameters that were studied, which were relevant clinically.
Human Rights Statement and Informed Consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and the Helsinki Declaration of 1975 that was revised in 2000. Informed written consent was obtained from the patient before their inclusion in study with the approval from ethical committee. The procedure was explained them regarding the nature and benefit of the study.