MRI is a noninvasive, radiation free modality with a better ability to asses soft tissues [1]. Arthroscopy has a diagnostic accuracy of 64 to 94% but is an invasive procedure and is associated with complications. Anterior cruciate ligament (ACL) is commonly injured ligament in knee [2] and usually associated with Meniscal injures [3]. Kean et al., in 1980’s used MRI in knee [4] The accuracy of MRI is very high in diagnosing knee lesions and has a sensitivity of 80% to 100% [5]. The purpose of our study was correlate MRI and arthroscopy in evaluation of knee injuries.
Materials and Methods
This is a prospective analytical study done from June 2012 to July 2014 in our institution. All patients of knee trauma with ACL and meniscal injuries of any age group were included in the study. The patients with associated fracture of femoral condyle, tibial plateau and dislocation, contraindications for MRI imaging and previous knee surgeries were excluded. The sensitivity, specificity, positive predictive values (PPV) and negative predictive values (NPV) was calculated from patients in whom the arthroscopy was done.
MRI technique: An informed consent was obtained prior to study after explaining the procedure of the examination to the patient. The examinations were carried out in a GE 1.5 TESLA MRI machine. The patient was placed in supine position on the MRI table. The knee was kept in the coil in extension and ten to fifteen degree external rotation (gives better imaging of ACL). The knee was secured in the coil by centering the joint. MRI scan was done using saggital (T2 FSE, PDFAT SAT, STIR, T2 FRFSE fatsat) Coronal PD FATSAT and Axial STIR sequences using the standard imaging protocol [Table/Fig-1].
Standard Imaging Protocol
| Sequences | Flip angle | TE | TI | TR | Slice thickness/ space | FOV | Matrix | NEX | Time |
|---|
| T2 FSE (Saggital) | 90 | 120 | NA | 4290 | 3.0/1.0 | 22x22 | 320x224 | 2 | 1:45 |
| PD FATSAT (Saggital) | 90 | 45.1 | NA | 2200 | 3.0/1.0 | 22x22 | 320x160 | 4 | 2:24 |
| STIR (Saggital) | 90 | 42.9 | 150 | 6258 | 3.0/1.0 | 22x22 | 256x160 | 4 | 3:00 |
| T2 FRFSE Fatsat (Saggital) | 90 | 82.6 | NA | 2281 | 3.0/1.0 | 22x22 | 320x256 | 3 | 2:22 |
| PD FATSAT (coronal) | 90 | 47.7 | NA | 2243 | 3.0/1.5 | 22x17.5 | 320x256 | 2 | 2:05 |
| STIR (Axial) | 90 | 47.3 | 150 | 6620 | 3.0/1.0 | 18x12.6 | 256x256 | 2 | 2:36 |
T2 FSE: T2 Weighted Fast Spin Echo, PD FATSAT: Proton Density Fat Saturation, STIR: Short Term Inversion Recovery, TE: Echo Time, TI: Time Of Inversion, TR: Repetition Time, FOV: Field Of Veiw, NEX: Number Of Excitations, NA: Not Applicable
Interpretation of images: All MRI images were acquired digitally with the use of a picture archiving and communication system (PACS) in DICOM (digital imaging and communications in medicine) format. The assessment of images was subsequently performed by the use of software by the radiologist blinded to the clinical diagnosis. The ACL was evaluated on saggital, coronal & axial images and categorized as intact or torn. It was a normal ACL was considered when a hypointense band like structure was seen. The presence of focal discontinuity or complete absence of ligament, abnormal signal intensity of the ligament, wavy contour or poor definition of its ligamentous fibres were all considered as ACL tear [Table/Fig-2a,b]. A hypointense meniscus without any altered signal intensity was considered normal. Presence of an intrameniscal high signal intensity was regarded as a tear and its grading was done according to weather it reaches to the articular surface or not [Table/Fig-3a,b].
Complete ACL tear:- (A) Saggital PDFAT SAT image showing complete non visualization of the ligament suggestive of complete ACL tear (B) Saggital T2WI showing complete ACL tear giving typical “question mark configuration” of PCL

Grades of meniscal tears on coronal PDFAT SAT sequence (A) Grade 1 tear of anterior horn of medial meniscus (B Grade 2 tear of anterior horn of medial meniscus

The degree of anterior tibial subluxation (ATS) was evaluated only on saggital images. On the selected image, a vertical line was drawn tangent to the posterior cortical margin of the mid-lateral femoral condyle excluding the overlying articular cartilage. The distance between the vertical line and posterior cortical margin of the lateral tibial condyle was determined as degree of subluxation (in millimeters) [Table/Fig-4a,b]. Accordingly ATS was measured with the increments of 5mm, patient with no subluxation were considered grade 0; those with 0 to 5mm of displacement were categorized under grade 1; and greater than 5mm under grade 2, and so forth.
Measurements of ATS , Saggital MRI images showing measurements taken at the level of mid-lateral femoral condyle (A) ATS measuring 5mm suggestive of grade 1 subluxation (B) ATS of 18mm suggestive of grade 4 subluxation

The amount of the fluid was measured quantitatively by obtaining antero-posterior distance of the effusion at its widest point in the midline and lateral aspect of suprapatellar pouch on saggital image [Table/Fig-5a,b]. An antero-posterior measurement of 10mm or less was a reasonable threshold value for distinguishing physiological from the pathological amount of fluid.
Fluid Measurement in Suprapatellar bursae, Saggital T2WI image showing antero-posterior diameter effusion in the midline of the lateral aspect of suprapatellar bursae (A) less than 10mm (B) more than 10mm

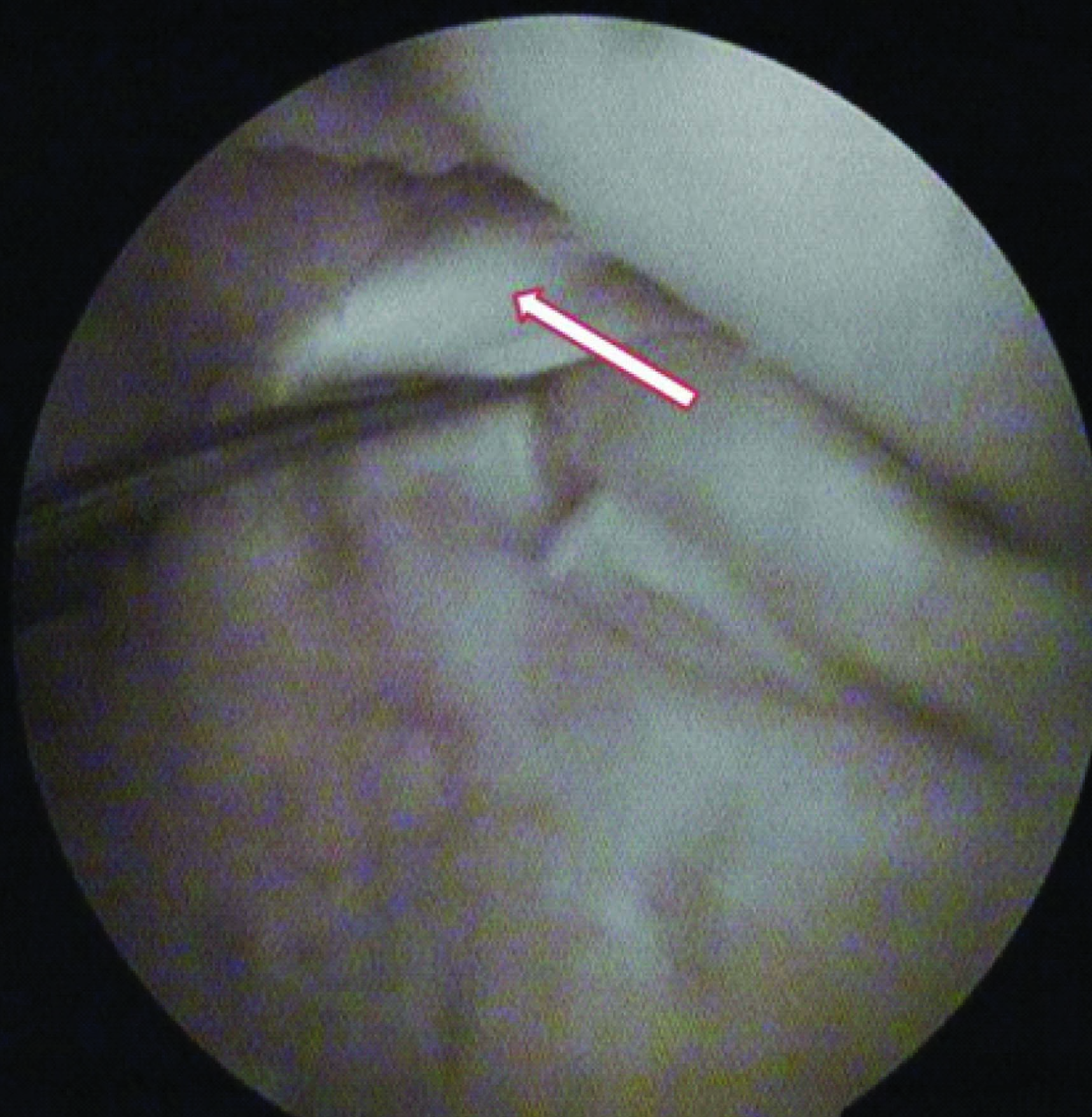
Arthroscopic examination: The arthroscopic examination was done by the orthopaedic surgeon of our hospital. All the arthroscopies were performed under spinal anaesthesia. They routinely divide the knee into following compartments i.e the suprapatellar pouch, patellofemoral joint, medial gutter, medial compartment intercondylar notch, posteromedial compartment, lateral compartment, lateral gutter and posterolateral compartment. A thorough examination of the knee was performed and the pathologic structure was identified. Further surgical intervention was carried out accordingly, ACL reconstruction for ACL tears [Table/Fig-6] and partial/subtotal menisectomy for meniscal tears [Table/Fig-7]. In isolated cases of ACL tears, ACL reconstruction was done using semitendinous gracilis graft (STG) or patellar tendon bone (PTB) graft.
Arthroscopic picture of 26 year old sportman showing ACL tear
Arthroscopic picture of 31year old male with RTA showing grade 4 tear of posterior horn of medial meniscus

Statistical Analysis
The results were presented in number and percentage for dichotomatous data in table and figures. MRI findings were compared with the arthroscopic findings to identify true positive, true negative, false positive and false negative pathologies. True positive were the cases in which the MRI findings were all comparable with the arthroscopic findings. True negative were the patients in whom the lesion was neither identified on MRI nor on arthroscopy. False positive were the patients in whom the lesion was identified on MRI but was not seen on arthroscopy and false negative were the patients in whom pathology was not identified on MRI but found on arthroscopy.
Statistical analysis was done by using descriptive and inferential statistics using Chi square test and predictive values. The Spearman correlation coefficient was calculated to correlate the findings of MRI with arthroscopy by using statistical software SPSS 17.0.
Results
A total of 230 patients of knee injuries with 71 having arthroscopic co-relation were studied. The decision of arthroscopy (diagnostic or therapeutic) was taken by the orthopedic surgeon. In remaining 159 patients arthroscopy was not done because some were managed conservatively when there was mild to moderate injuries. Also, as our institute is a tertiary center situated in a rural area, many of them were not able to afford. The incidence, degree of subluxation and knee joint effusion was calculated from all the 230 patients.
The correlation of MRI findings with arthroscopic findings was done in 71 patients and was categorized into true positive, true negative, false positive and false negative cases [Table/Fig-8]. The sensitivity, specificity, PPV and NPV were calculated (in%) [Table/Fig-9]. Using spearman co-relation test the MRI were correlated with arthroscopy and for ACL it was 0.577, for MM 0.805 and for LM it was 0.746 which showed a significant correlation between both the investigations [Table/Fig-10].
True positive, true negative, false positive and false negative of MRI and arthroscopic findings as the reference data
| Test | True positive | True negative | False positive | False negative |
|---|
| ACL MRI findings | 29 | 31 | 7 | 4 |
| MM MRI findings | 29 | 35 | 5 | 2 |
| LM MRI findings | 21 | 36 | 8 | 6 |
Sensitivity, Specificity, PPV and NPV aspects of MRI and arthroscopic diagnosis of ACL, MM and LM tears
| Accuracy of MRI findings using Arthroscopic findings as the reference data |
|---|
| Component Test | ACL % | MM % | LM % |
|---|
| Sensitivity | 87.87 | 93.54 | 77.77 |
| Specificity | 81.57 | 87.50 | 81.81 |
| Positive Predictive Value | 80.55 | 85.29 | 72.41 |
| Negative Predictive Value | 88.57 | 94.59 | 85.71 |
Correlation of MRI findings with arthroscopy using spearman correlation,
| MRI |
|---|
| ACL | MM | LM |
|---|
| Arthroscopy | 0.577** | 0.805** | 0.746** |
Note : Spearman Correlation was used, **. Correlation is significant at the 0.01 level
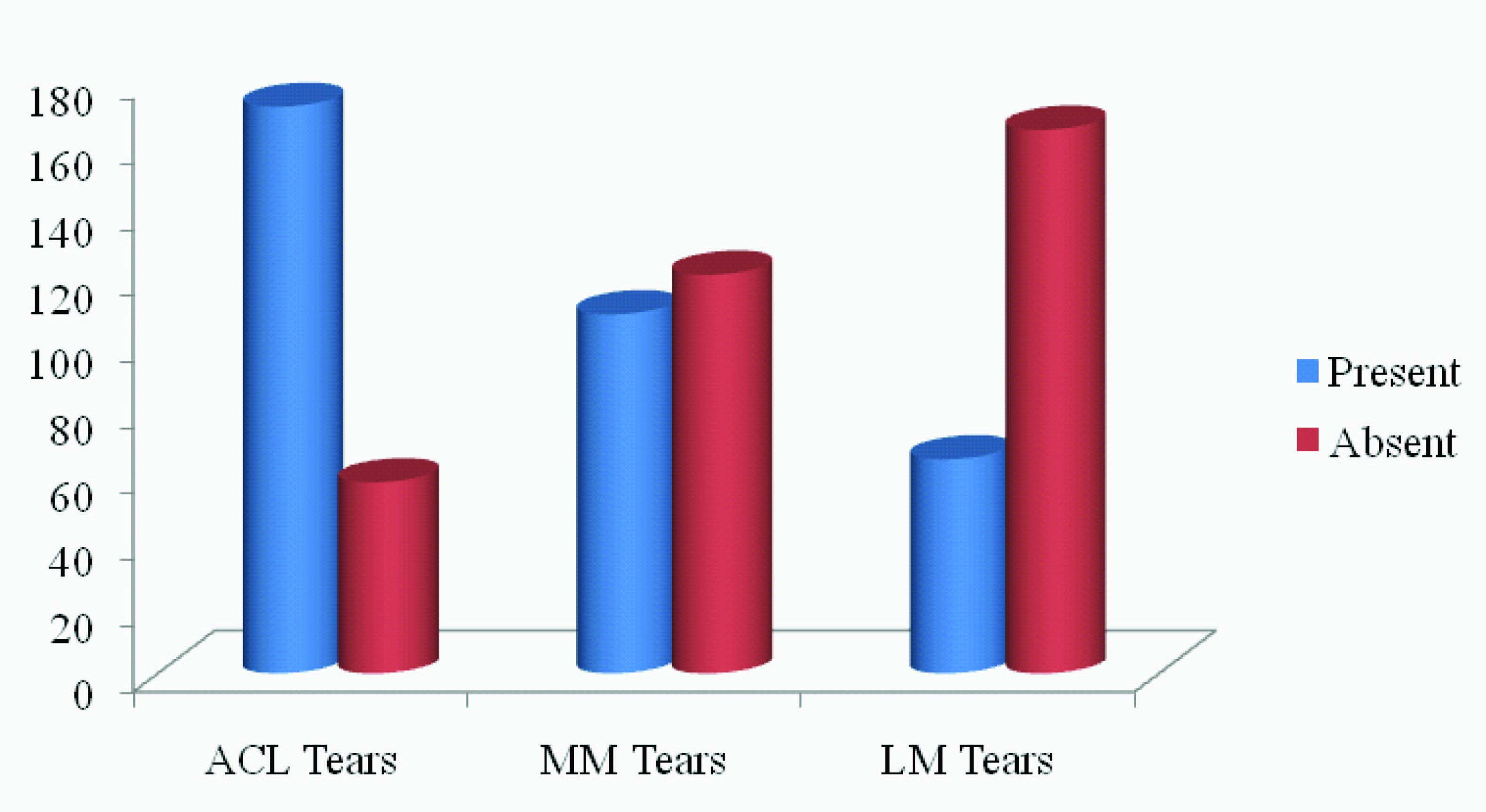
The incidence of ACL tear was 74.7% that of the medial meniscus (MM) and lateral meniscus (LM) was 47.3% and 28.2% of respectively [Table/Fig-11].
Graph showing Incidence of ACL, MM and LM tears
The presence and absence of ACL tear was 172(74%) and 58(25%), MM was 109 (47%) and 121(52%), LM was 65(28%) and 165 (71%) respectively
We found 35.6 % incidence of ATS with maximum patients having grade 1 category subluxation [Table/Fig-12]. Patients with grade 2 or more were more commonly associated with complete ACL tear.
Graph showing the frequency of subluxation of the tibia and its grading, The grade 1 subluxation was seen in 34 patients (41%) , Grade 2 in 24 patients (29%), Grade 3 in 23 patients (28%) and grade 4 in 1 patient (1%).

The threshold value to distinguish physiological from pathological amount of fluid was 10mm in lateral aspect of suprapatellar pouch in our study. Patients with 10mm or more fluid in lateral suprapatellar pouch were more frequently associated with ACL tears, meniscal tears, bone bruise and tibial subluxation [Table/Fig-13].
showing the internal derangement of knee joint in presence of knee joint effiusion, Chi Square = 1.535 p Value = 0.215
| Amount of fluid (knee effusion in suprapatellar bursae) | Fluid | Total (%) |
|---|
| With internal derangement (%) | Without internal derangement (%) |
|---|
| Less than 10 mm | 62 (30.8) | 12 (6.0) | 74 (36.8) |
| More than 10 mm | 114 (56.7) | 13 (6.5) | 127 (63.2) |
| Total | 176 (87.6) | 25 (12.4) | 201 (100.0) |
Discussion
The role of MRI has steadily increased and now it has become the investigation of choice for most of the lesions of knee. It is also being used for pre and post operative evaluation. It is a non-invasive technique that does not require contrast administration and is not operator dependant. Complete evaluation of all the internal structures of the knee is not possible with other modalities like radiography, arthrography and ultrasonography. Even with arthroscopy lesions such as peripheral meniscal tears, inferior surface tears and osteochondritis dessicans without articular cartilage damage are mostly not detected.
Meniscal injuries are a common cause of knee dysfunction and leads to two-third of all knee disturbances [6]. Similiarly ACL tears also leads to significantly unstable knee joint. Despite being the most frequently injured ligament of the knee, its clinical diagnosis remains difficult. MRI, a noninvasive and radiation free diagnostic modality is commonly used for these internal derangements [7].
Our study included 230 patients clinically suspected as having some form of internal derangement of knee. Maximum were young subjects in the age group of 21-30 y (32.2%). Also, 77% of subjects were males outnumbered females in all age groups of this study.
Out of total 230 patients, ACL tear was most common finding affecting 172 patients (74.8%), followed by Medial meniscus tear in 109 (47.4%) and lateral meniscus tear seen in 65 patients (28.3%). In a similar study by Singh et al., 45.08% showed ACL tear, among which 66.67% were partial and 21.13% were complete ACL tear. The authors concluded ACL tears to be more common than other ligamentous injuries [8].
There was preponderance of MM over LM in our study which was again correlated with the study done by Singh et al., [8]. Out of 173 they found 57(32.9%) patients showed MM tear and 28 (16.1%) patients showed LM tear.
M.Schurz et al., [9] reviewed patients with the clinical diagnosis of meniscal tears and recommended MRI as a clarifying diagnostic tool for the evaluation of meniscal tears, especially LM ruptures.
In our study, we have correlated the MRI finding with arthroscopy in 71 patients and sensitivity, specificity, PPV and NPV was calculated [Table/Fig-14]. There were few false positive and false negatives cases in our study. As the accuracy in the diagnosis of menisci and cruciate ligaments depend on quality of imaging equipment and the skills and experience of clinical examiner, radiologist and arthroscopist [10]. It also depends on technical factors (imaging parameters, coil strength, surface coil use and planes of image). The diagnosis of partial tears of ACL may not be accurate due to overlying synovial reaction. The MRI sensitivity for menisci also differs, many tear may be missed or overdiagnosed. A good clinical experience is therefore required in the presence of normal MRI [11].
Comparision of sensitivity and specitivity with other studies: our results were in agreement with those of the authors of recent publications
| Studies | Sensitivity | Specificity |
|---|
| ACL % | MM% | LM% | ACL % | MM% | LM% |
|---|
| Ali Akhbar Esmaili et al., [10] | 78.3 | 75 | 66.6 | 95.7 | 94.7 | 86.2 |
| F. Rayan et al., [12] | 81 | 76 | 61 | 96 | 52 | 92 |
| Ruth Crawford et al., [13] | 86.5 | 91.4 | 76.0 | 95.2 | 81.1 | 93.3 |
| Vaz CE et al., [14] | - | 97.5 | 91.9 | - | 92.9 | 93.6 |
| Noha et al., [15] | 77.8 | 47 | 100 | 100 | 95 | 75 |
| Our study 2014 | 87.8 | 93.5 | 77.7 | 81.5 | 87.5 | 81.8 |
We have compared the sensitivity and specificity of our study by various similar studies done in last 10 y and made comparative chart [Table/Fig-14] [10,12–15].
In our study ATS was found in 82 patients, with 34 patients categorized under grade 1 and 48 patients showed a subluxation of grade 2 or more. Patients with complete ACL tear showed grade 2 or higher ATS, thus suggesting that significant ATS is existent with complete ACL tears. In a study done by Chan et al., [16], the presence of torn ACL was established on the basis of measurements of the position of the lateral tibial plateau relative to the lateral femoral condyle on a saggital image. Routine MRI examination is performed with full extension and fifteen degree of external rotation. The extended position of knee is ideal for measuring anterior laxity as the ACL is taut in extension. In their study ATS of more than five mm was exhibited in 86% of patients with a complete tear of ACL. This compared well with the sensitivity of conventional MR imaging criteria. However the MR criterion of tibial subluxation (>5mm) was better than conventional criteria (focus on morphology of the ligament without considering joint alignment) for distinguishing partial from complete ACL tear as the conventional MRI criteria results into overestimation of degree of ACL tear. Whereas significant (>5mm) ATS occurs only when there is complete ACL tear. Hence they concluded that the presence of ATS >5mm i.e. grade two or more relative to the femur on MR images of the knee is a helpful adjunctive sign of complete ACL tear. Proper use of this sign requires little experience yet it provides sensitivity for identifying complete ACL tear.
We have also calculated the fluid in the affected knees and its association with internal derangements. According to the study done by Kolman et al., [17] measurements were taken in the lateral aspect of the suprapatellar pouch or lateral gutter which are more sensitive than measurements obtained in the midline suprapatellar pouch and are more reliable area than the para-ACL compartment. The patients were positioned in the extremity coil with five to fifteen degree of external rotation ideal for the measurements of lateral suprapatellar pouch. The major limitation in their study was the method of measurement. As the saggital plane alone is not the precise method for measurement, axial planes or some volumetric measurement would have been more accurate for the measurements. Hence, they concluded that, MRI is very sensitive in detecting joint effusions. Patients in whom there was no significant effusion in the lateral aspect of the suprapatellar pouch were free of internal derangements. So the threshold value for distinguishing physiologic and pathologic amount of fluid is less than ten mm in the lateral suprapatellar pouch on MRI.
The major limitation in our study was inadequate co-relation of MRI and arthroscopy. A large number of co-relation with arthroscopy would have been ideal. Orthopedicians had access to MRI scans and reports at the time of arthroscopy, therefore this was not a double blind study.
Conclusion
MRI is a non-invasive, radiation free and an excellent imaging modality to evaluate ligaments of the knee joint and surrounding soft tissue. The diagnostic yield is increased with appropriate use of sequences and proper analysis of images in all planes. Almost all the ligamentous and meniscal injuries can be diagnosed with high level of confidence. Pathological entities should be carefully differentiated from normal variants, pitfalls and artifacts of imaging. In traumatic setting in post-traumatic knee, MRI evaluation before arthroscopy has been proved as cost-effective. Despite the fact that arthroscopy has altered the management of knee pathologies, most orthopeadicians admit the limitations of the procedure in the evaluation of extra-articular pathology, its invasiveness, cost and uncommon but possible complications associated with it.
T2 FSE: T2 Weighted Fast Spin Echo, PD FATSAT: Proton Density Fat Saturation, STIR: Short Term Inversion Recovery, TE: Echo Time, TI: Time Of Inversion, TR: Repetition Time, FOV: Field Of Veiw, NEX: Number Of Excitations, NA: Not Applicable
Note : Spearman Correlation was used, **. Correlation is significant at the 0.01 level