Mounier-Kuhn syndrome (MKS) - Pathognomonic Findings
Saurabh Kumar1, Alok Kumar Mittal2
1 Consultant Radiologist, Department of Radiology, Star Imaging and Pathological Lab, New Delhi, India.
2 Consultatnt Radiologist, Department of Radiology, Star Imaging and Pathological Lab, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr Saurabh kumar, F-7 Bali nagar, New delhi -110015, India. Phone : 9868628034, E-mail : sunny_mamc911@yahoo.com
Computed tomography, Tracheobronchomegaly
Case Report
A 34-year-old male patient was referred for chest CT evaluation in our department, with history of long history chronic cough, episodic shortness of breath, now having acute exacerbation of symptoms for past few days with chest pain. Patient was non smoker with average built.
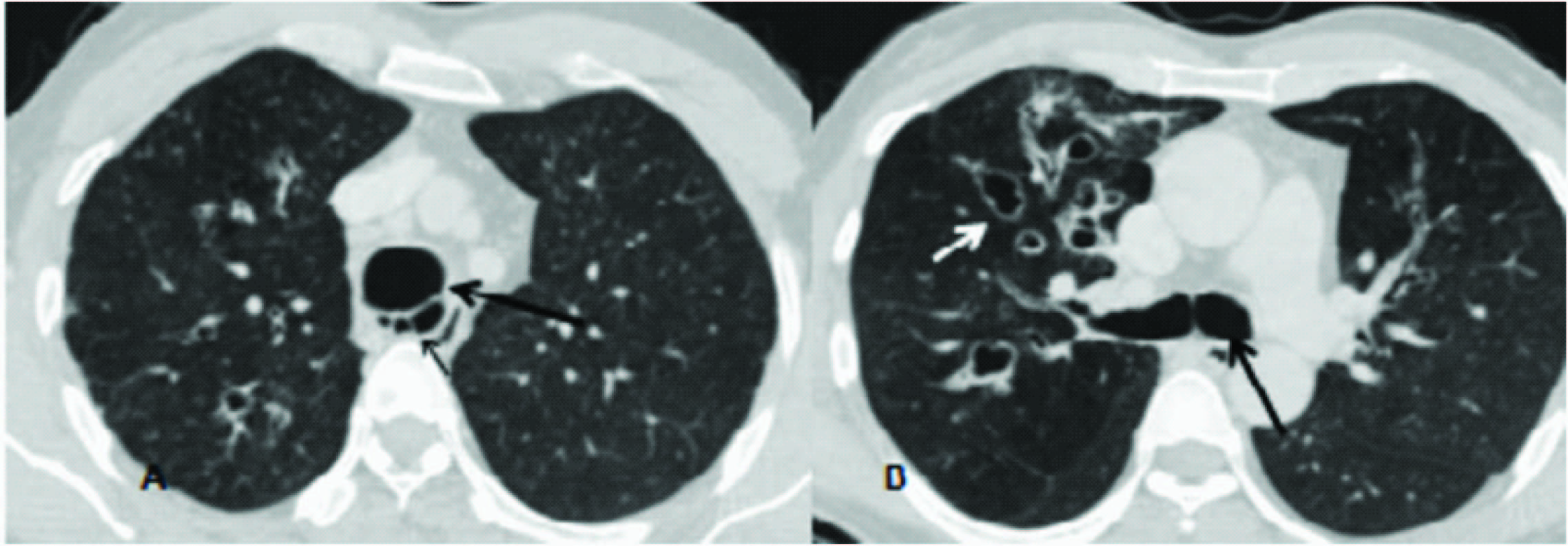
Computed tomography revealed abnormally dilated trachea and bilateral main stem bronchus.The transverse diameter of trachea (2 cm proximal to arch of aorta) was 30 mm, with diameter of right and left main bronchus being 19.5 mm and 18.5mm respectively. There were associated multiple diverticulae/sacculations seen arising from intrathoracic trachea and proximal main stem bronchus with bilateral cystic broncheictasis [Table/Fig-1,2,3] and mosaic attenuation in bilateral lung fields. The post processed thick minimal intensity images (MinIP [Table/Fig-2] were particularly useful in demonstrating dilated tracheobronchial tree and also mosaic attenuation in bilateral lung fields which can either be due to associated small airway disease or pulmonary artery hypertension. Thus based on imaging findings the diagnosis of Mounier-Kuhn syndrome was given. Fibero-optic bronchoscopy further confirmed the diagnosis of abnormally dilated tracheobronchial tree and patient was started on chest physiotherapy and oral antibiotics.
Axial CT chest sections –lung window (A,B) showing abnormal dilatation of tracheobronchial tree(large arrows) with small arrow in A showing tracheal wall diverticulae and small arrow in B showing cystic bronchiectasis,
Saggital Thick minimal intensity projection(MinIP) (image A and B) demonstrating tracheal wall diverticulae with mosaic attenuation and perfusion abnormality in bilateral lung fields

Coronal CT chest sections lung window showing corrugated appearance of tracheobronchial wall due to multiple small diverticulae and sacculation in trachea and proximal main stem bronchi in image B with central cystic bronchiectasis is shown in image A

Mounier-Kuhn syndrome (MKS) or tracheobronchomegaly is frequently seen in middle age men [1]. The basic pathophysiology is defective tracheobronchial wall [1] which lack or has atrophic smooth muscle and elastic leading to development of diverticular projections of memberanous tissue between the cartilaginous rings with resultant defective mucociliary clearance leading to mucous stagnation and recurrent infection and bronchiectasis.
Diagnosis is generally made radiographically [2] by chest radiography which shows abnormally dilated trachea however clinical examination and chest radiography may be misleading in patients with Monier-Kuhn Syndrome as tracheobronchomegaly can be easily overlooked on radiographs, however CT scan remain the mainstay modality for diagnosing the disease. It helps in accurate measurement of tracheobronchial tree and associated diverticulosis. The diameter of trachea, right and left mainstem bronchus which exceed 3 cm, 2,4 cm, 2.3 cm on standard chest radiography [3] or bronchography is virtually diagnostic for tracheobronchomegaly. CT further provides information regarding associated findings of bronchiectasis [2] mostly central and cystic variety with pulmonary fibrosis and pulmonary artery hypertension in chronic cases. With help of post processing techniques in CT like MinIP images one can get a wholesome idea of tracheobronchial tree in few images and lung perfusion abnormalities with areas of mosaic attenuation can be readily picked upon which are generally seen in patients with this disease. Studies have further shown the importance of MinIP images in determining lung perfusion abnormalities in patients with chronic pulmonary hypertension [4]. Differential diagnoses include connective-tissue disorders [2]. Ehlers-Danlos syndrome, Marfan syndrome and cutis laxa in which secondary tracheobronchial enlargement is seen.
Treatment is generally controlling acute exacerbations with antibiotics and postural drainage, while surgical treatment by resection or stenting [5] has limited benefits due to widespread nature of disease.
Thus CT is mainstay modality of choice in reaching diagnosis of Mounier-Kuhn syndrome.
[1]. Brant William E, Clyde A Helms, Fundamentals of diagnostic radiology 2007 Lippincott Williams and Wilkins [Google Scholar]
[2]. Menon B, Aggarwal B, Iqbal A, Mounier-Kuhn syndrome: Report of 8 cases of tracheobronchomegaly with associated complicationsSouth Med J 2008 101:83-87. [Google Scholar]
[3]. Katz I, Levine M, Herman P, Tracheobronchiomegaly. The Mounier-Kuhn syndromeAm J Roentgenol Radium Ther Nucl Med 1962 88:1084-94. [Google Scholar]
[4]. Rossi A, Attina D, Borgonovi A, Evaluation of mosaic pattern areas in HRCT with Min-IP reconstructions in patients with pulmonary hypertension: could this evaluation replace lung perfusion scintigraphy?European Journal of Radiology 2010 81(1):e1-6. [Google Scholar]
[5]. Ernst A, Majid A, Feller-Kopman D, Guerrero J, Boiselle P, Loring SH, Airway stabilization with silicone stents for treating adult tracheobronchomalacia: A prospective observational studyChest 2007 132:609-16. [Google Scholar]