Juvenile Dermatomyositis (JDM) is a rare autoimmune inflammatory disease of muscles affecting children and adolescents with soft tissue calcification and varying systemic involvement. Though diagnosis is primarily by clinical, biochemical and histopathological tests, Imaging has unique significance from characterizing the calcinosis, detecting early changes in muscle in active phase of the disease, diagnosing potential complications,rule out other important differentials, guide biopsies ,and assessing the progress on follow up. Four distinct patterns of calcinosis have been described in relation to dermatomyositis which need to be differentiated from other aetiologies of soft tissue calcification and myopathies.
Case Report
A 16-year-old non-alcoholic non smoker male presented with gradually progressive weakness and tautening of the muscles of bilateral thighs and arms since last two years with pain on active movements. He was unable to ascend stairs, sit himself in a chair or raise objects overhead. There was associated complaint of painful hard swellings in bilateral axilla with extrusion of white particulate materials through a nonhealing ulcer in right axilla [Table/Fig-1]. There was a history of rash two months back, which was erythematous, non-itchy, non-scaly over face, mainly around the eyes which disappeared within a month leaving behind residual hyperpigmentation. There was no history of dysphagia, other systemic complaints, any significant history in past or similar complaints among first degree relatives in family.
Extrusion of calcified white lumps seen in right axilla

Clinical examination revealed decreased power in bilateral thigh (2/5) and upper arm muscles (3/5). Symmetrical tenderness was seen involving the extensor compartment muscles in both thighs with preserved deep tendon reflexes. Few hyperpigmented spots seen in perioral region and in trunk .Biochemical investigations revealed highy raised levels of CPK-MB,LDH and SGOT enzymes with mild anaemia [Table/Fig-2]. Other blood parameters like levels of calcium, phosphate, vitamin D, parathormone, TSH and uric acid were within normal limits [Table/Fig-2]. He tested negative for HIV and other viral serological markers. NCV test was normal.EMG showed short-duration, low-amplitude polyphasic units on voluntary activation and increased spontaneous activity with fibrillations suggesting features of myopathy.
Blood Biochemistry Results on Admission and at 1 Month Interval
| Blood Parameters | On admission | At 1 month interval post therapy |
|---|
| Hb | 11.5 g/dl | 12.2 g/dl |
| ESR | 39 mm/hr | 14 mm/hr |
| UREA/CREATININE | 20/0.7 mg/dl | 19/0.5 mg/dl |
| URIC ACID | 5.1 mg/dl | 4.8 mg/dl |
| Ca/PO4 | 8.3/4.5 mg/dl | 7.8/2.9 mg/dl |
| Na/K | 144/4.8 mmol/L | 139/ 3.7 mmol/L |
| RBG | 112 mg/dl | 110 mg/dl |
| LDH | 3966 U/L | 180 U/L |
| AST/ALT | 344/150 U/L | 35/38 U/L |
| CK | 10375 U/L | 200 U/L |
| AMYLASE | 35 U/L | 30 U/L |
| TSH | 2.72 mIU/L | 1.55 mIU/L |
| PTH | 32.1 ng/L | 35 ng/L |
List of Abbreviations:Hb=Haemoglobin,ESR=Erythrocyte sedimentation Rate,Ca= calcium, PO4=inorganic phosphate,Na=sodium,K-potassium,RBG=random blood glucose,LDH=Lactate dehydrogenase,AST/SGOT=Aspartate aminotransferase,ALT/SGPT=Alanine aminotransferase, CK=Creatine kinase(total),TSH=thyroid stimulating hormone,PTH=Parathyroid hormone
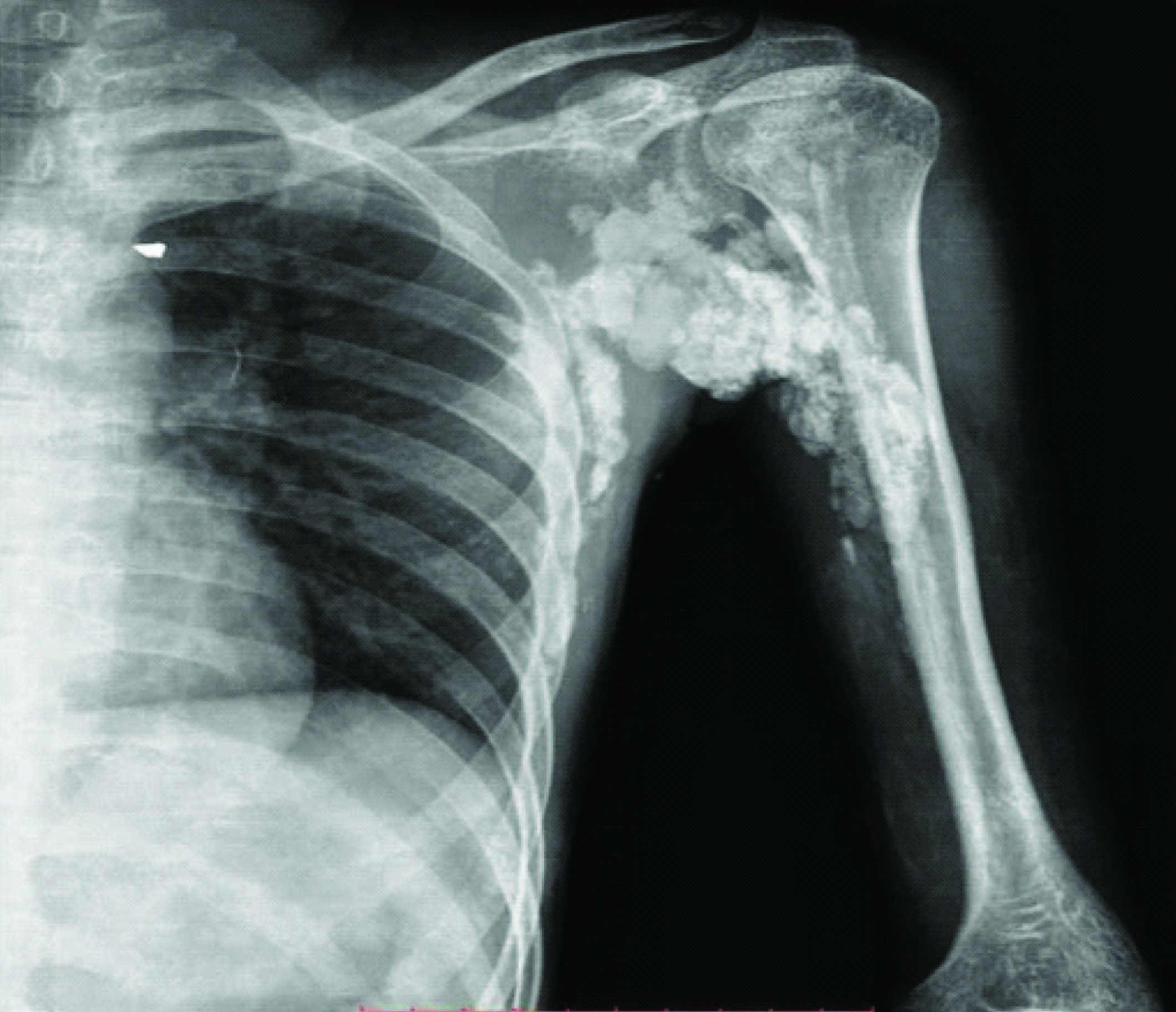
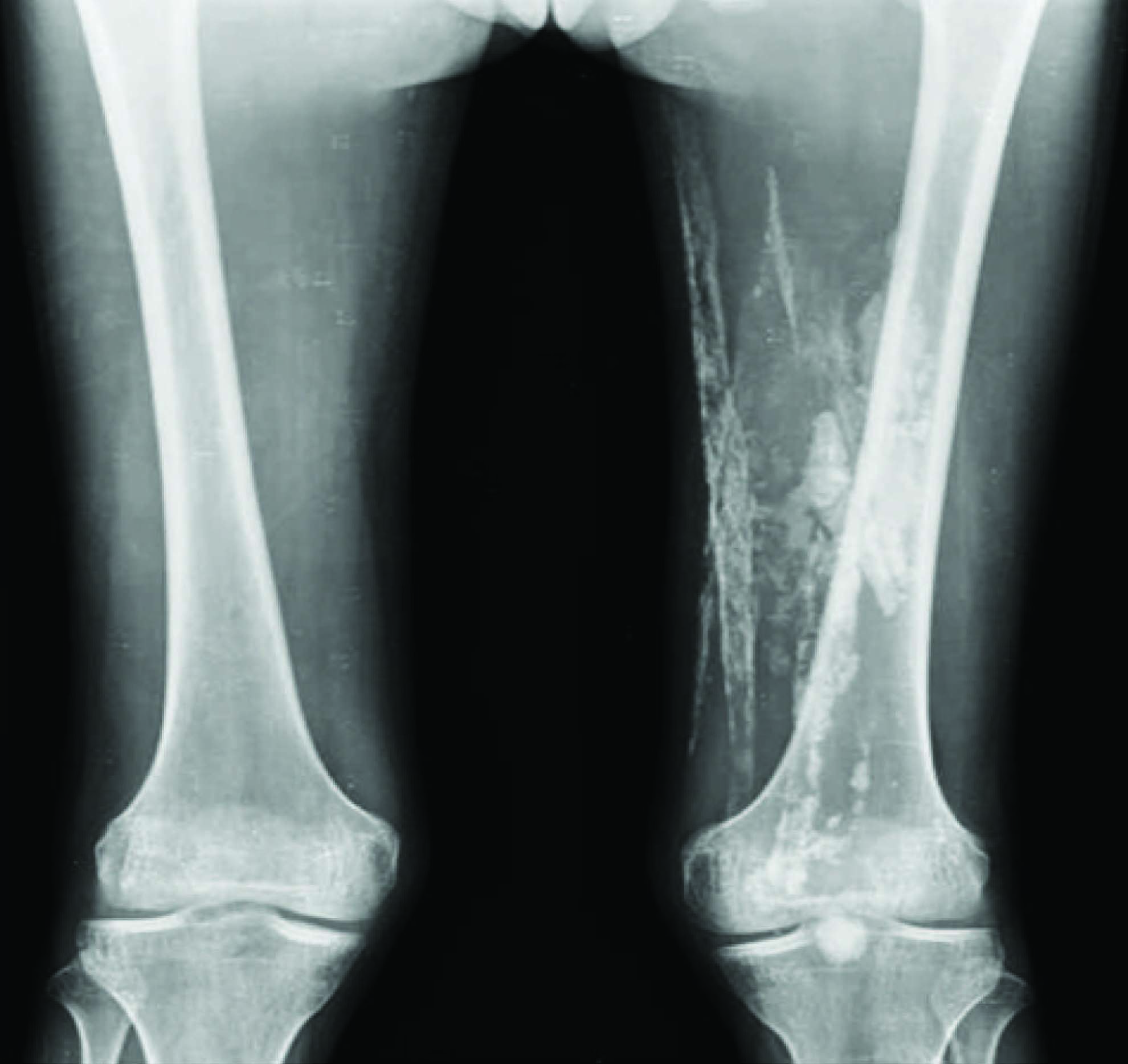
Routine radiography of the chest and bilateral upper limbs and lower extremities were done. Chest X-Ray revealed clumped masses and sheet-like calcifications in bilateral axilla and lateral chest wall. Radiography of upper limbs [Table/Fig-3a,b] and bilateral thighs [Table/Fig-3c] revealed clumped and sheet-like calcification seen in soft tissue of bilateral upper arms and left thigh muscles.
X-ray of right arm (AP view) shows clumped and sheet-like calcification seen in soft tissue of upper arm and axilla

X-ray of left arm (AP view) shows clumped and sheet-like calcification seen in soft tissue of upper arm and axilla
X-ray of bilateral thighs (AP view) shows clumped and sheet-like calcification seen in soft tissue of left thigh muscles
X-Ray of both hands revealed no evidence of acro osteolysis or soft tissue calcifications.
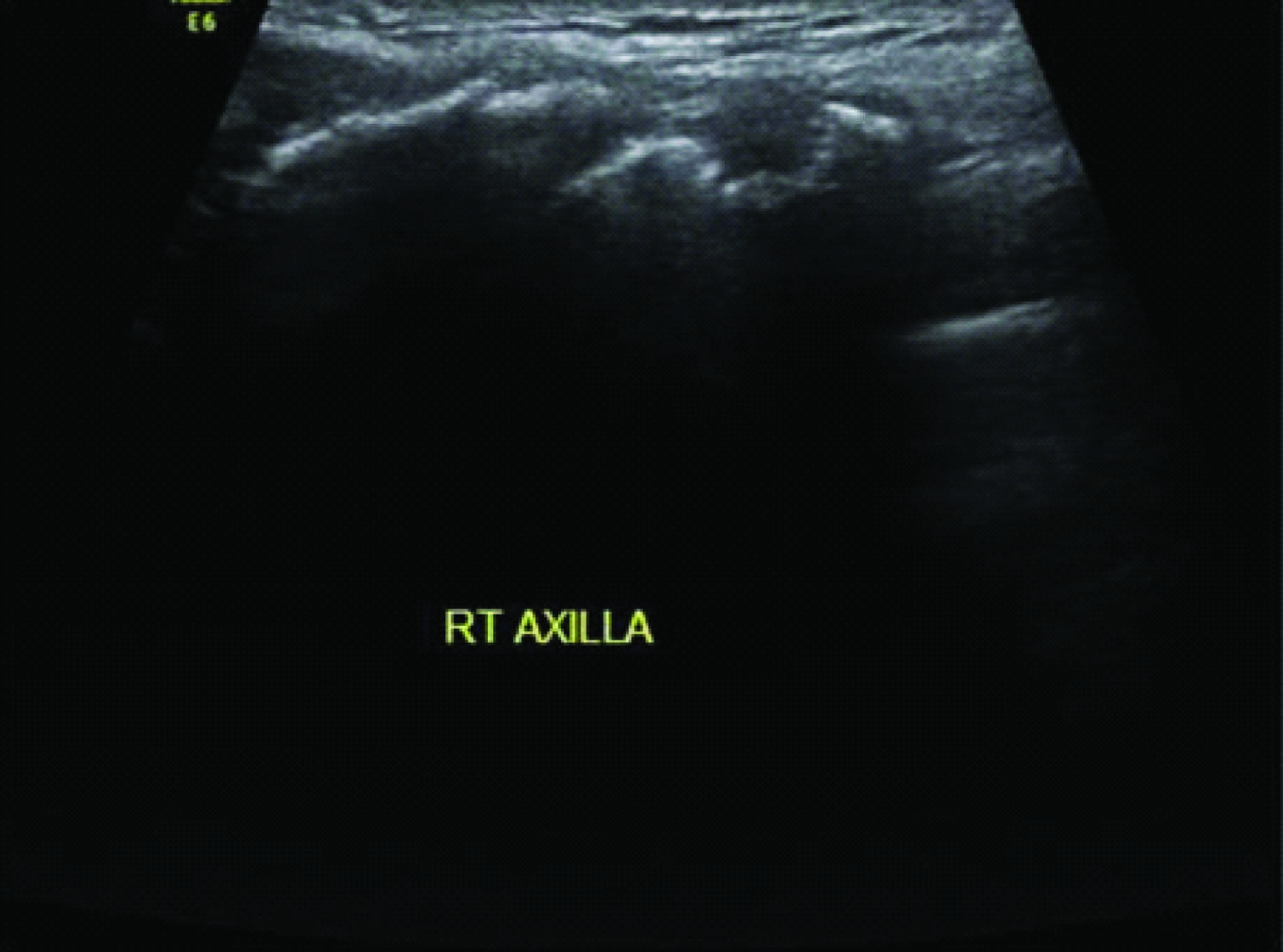
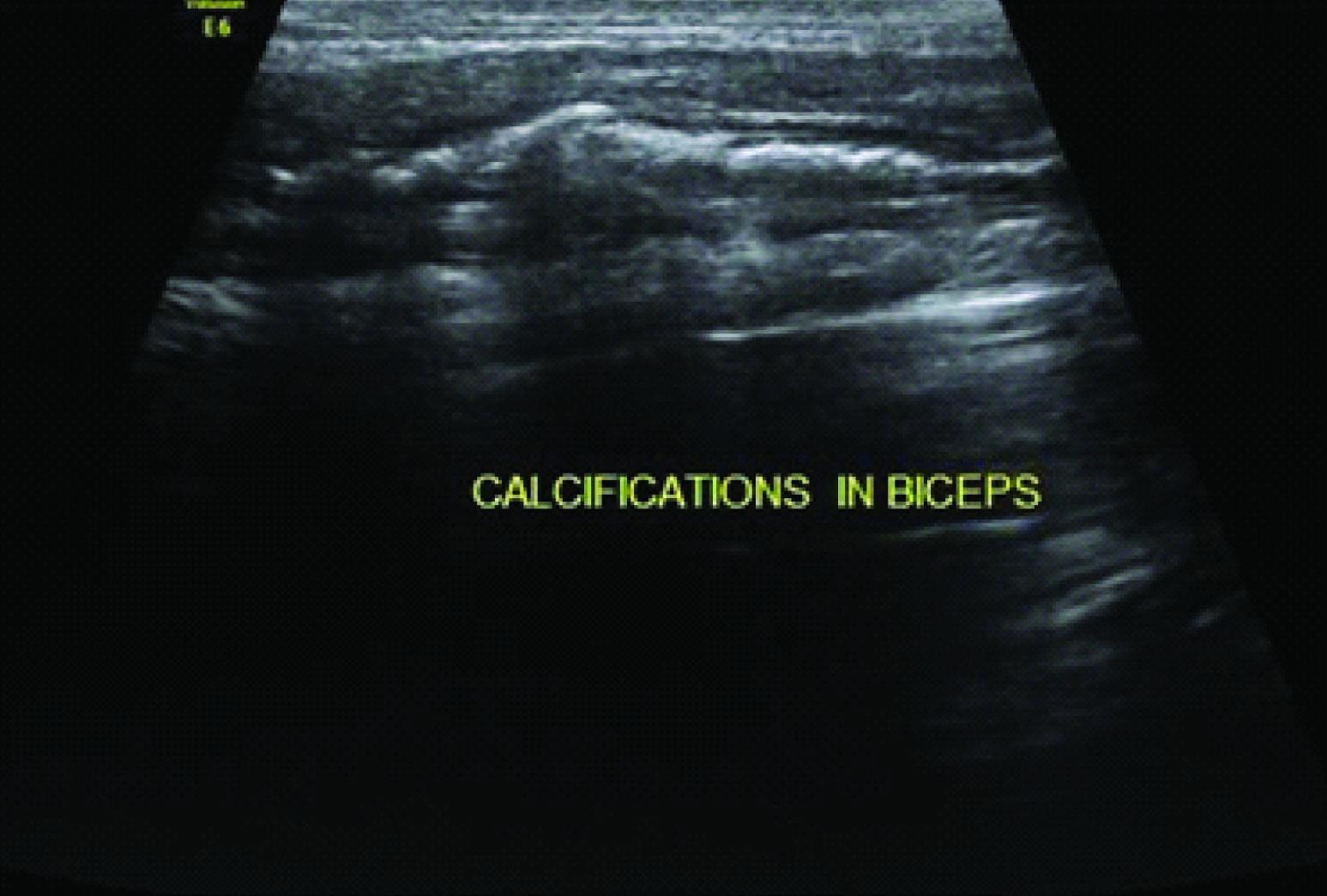
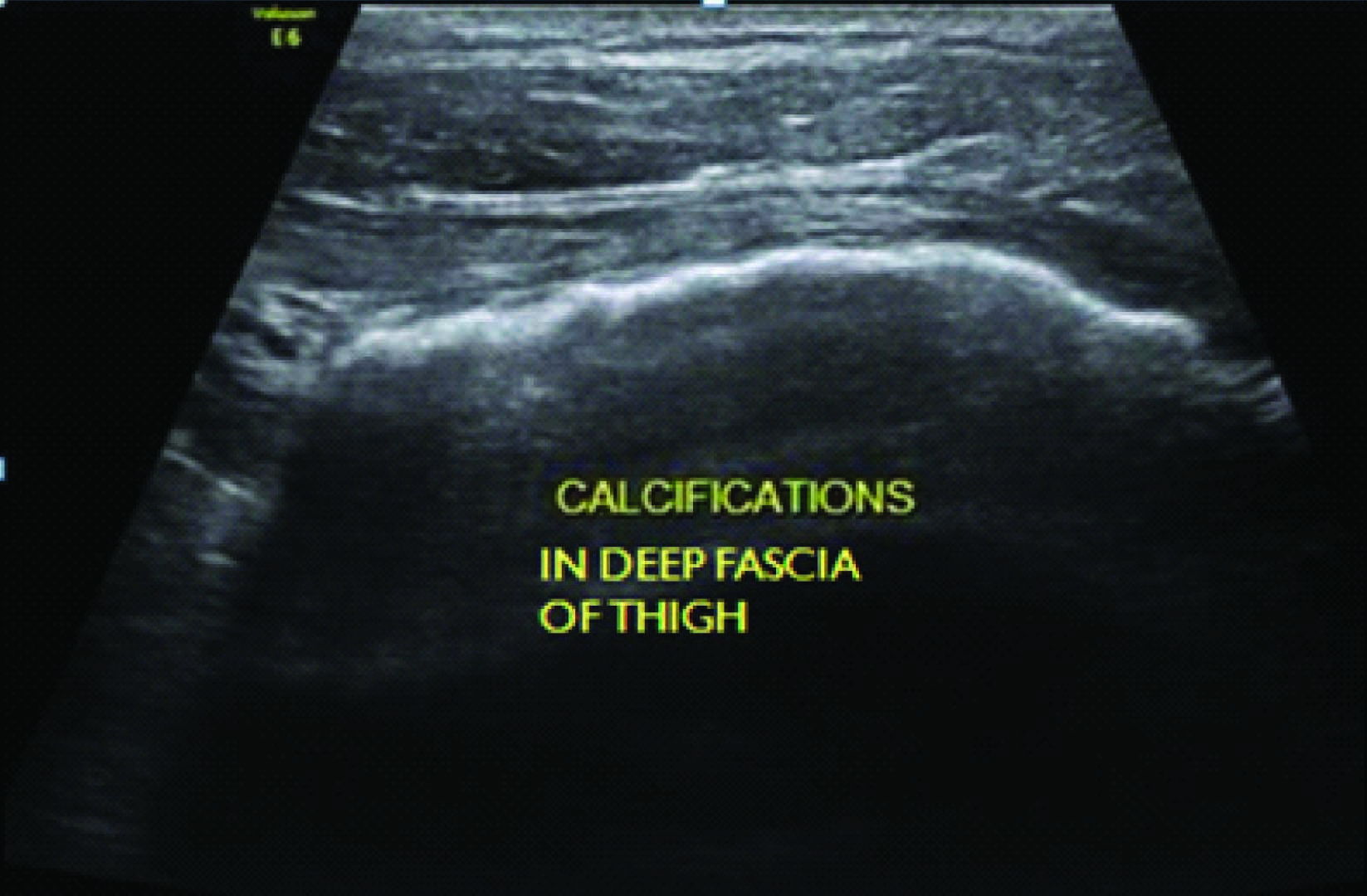
Sonography of affected sites revealed clumps of calcific masses both in subcutaneous [Table/Fig-4a] and deep intermuscular planes [Table/Fig-4b] along with linear sheet like calcification in deep fascial planes in thigh [Table/Fig-4c]. No obvious evidence of subcutaneous oedema or lace like reticular calfications seen in subcutaneous plane.
USG shows clumps of calcified masses in superficial subcutaneous plane in right axilla
USG shows clumps of calcified masses in deep muscular plane within biceps muscle
USG shows linear sheet like calcification in deep fascial plane of thigh
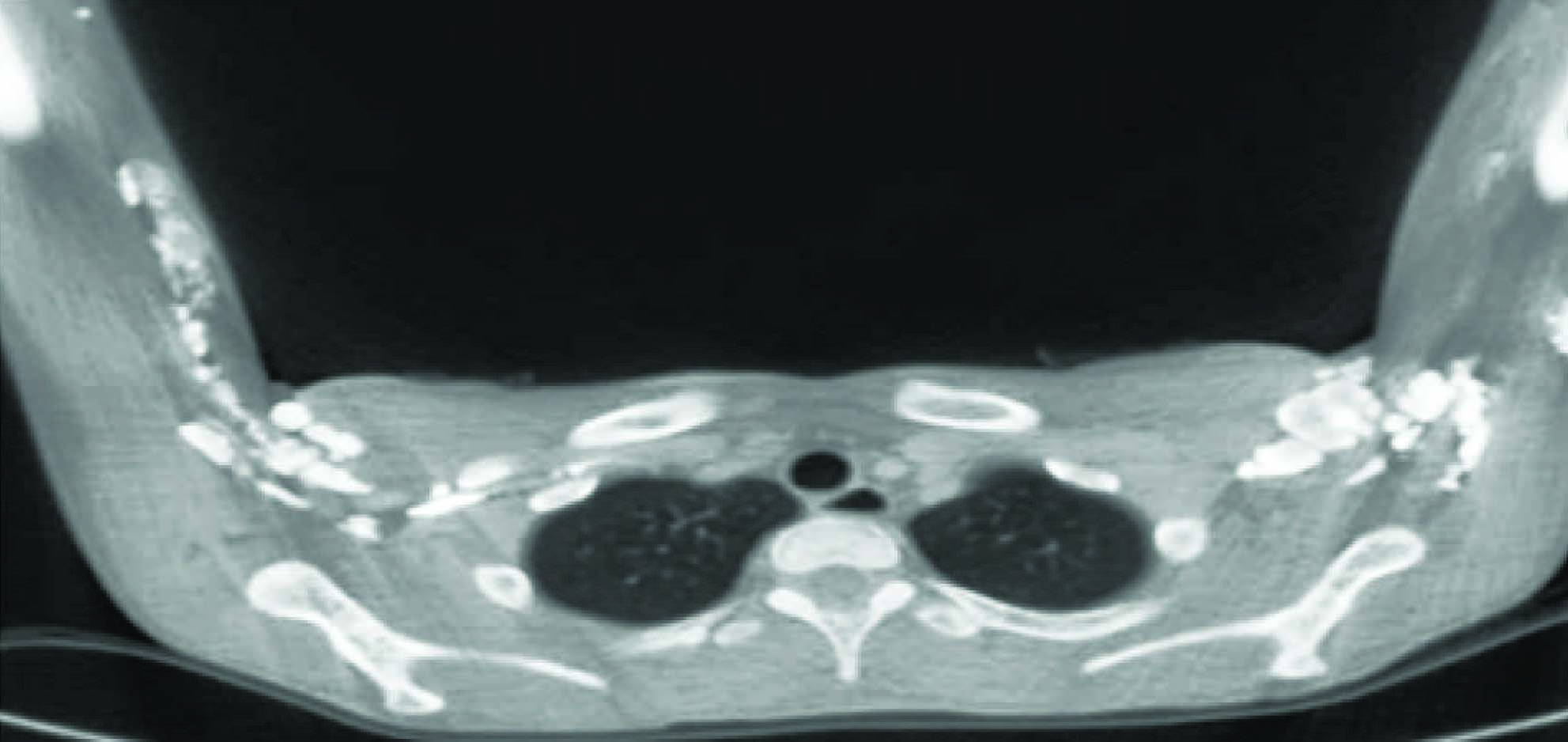
A low dose HRCT scan of Chest was undertaken to rule out associated interstitial lung disease. CT scan demonstrated dystrophic clumpy masses and sheet-like calcifications seen in the inter muscular and fascial planes of bilateral axilla, lateral chest wall and arm [Table/Fig-5]. Lung parenchyma otherwise was unremarkable with no evidence of interstitial lung disease.
CT scan of Chest axial section demonstrates dystrophic clumpy calcified masses and sheet-like calcifications seen in the inter muscular planes of bilateral axilla, lateral chest wall and arm
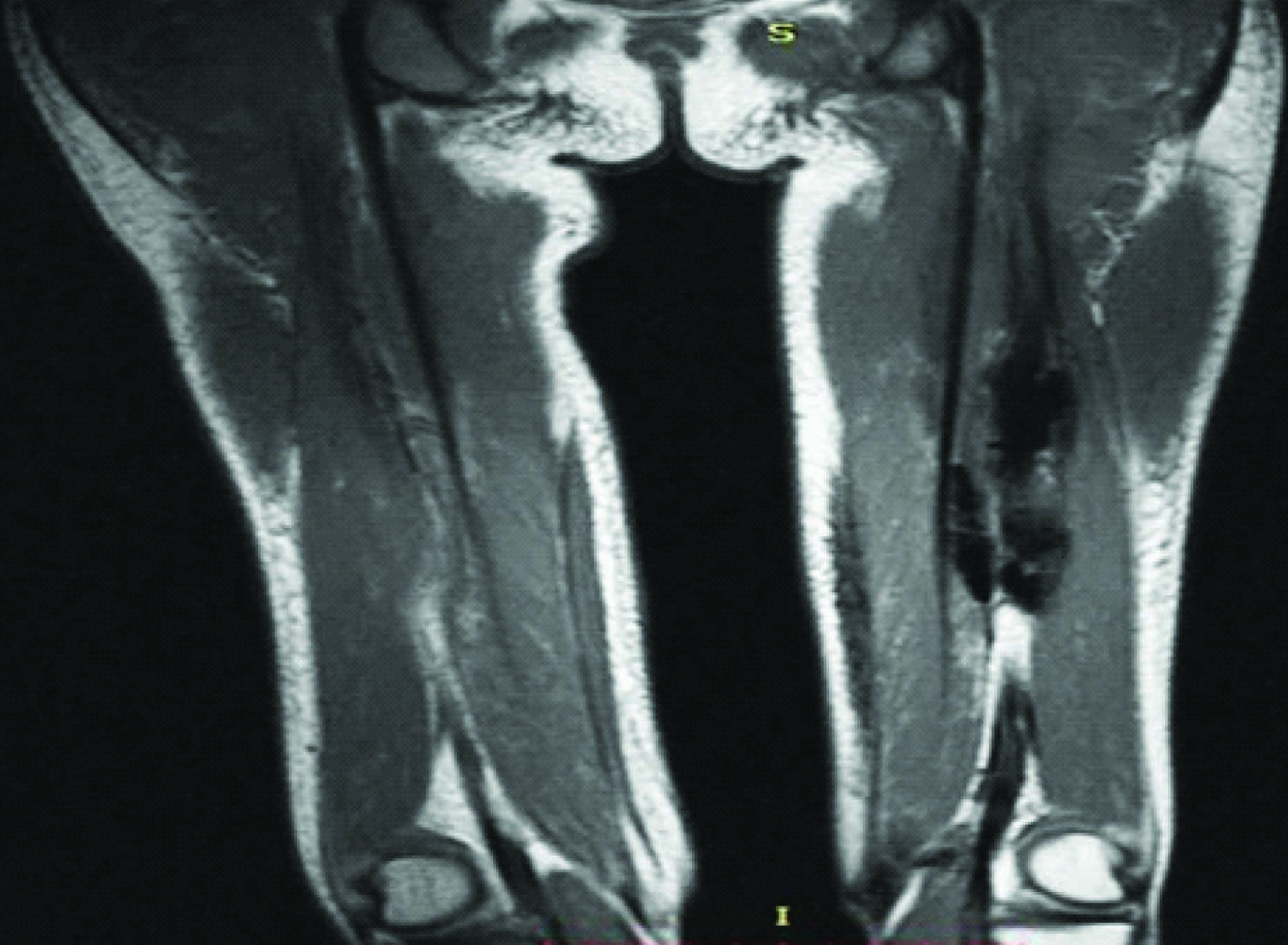
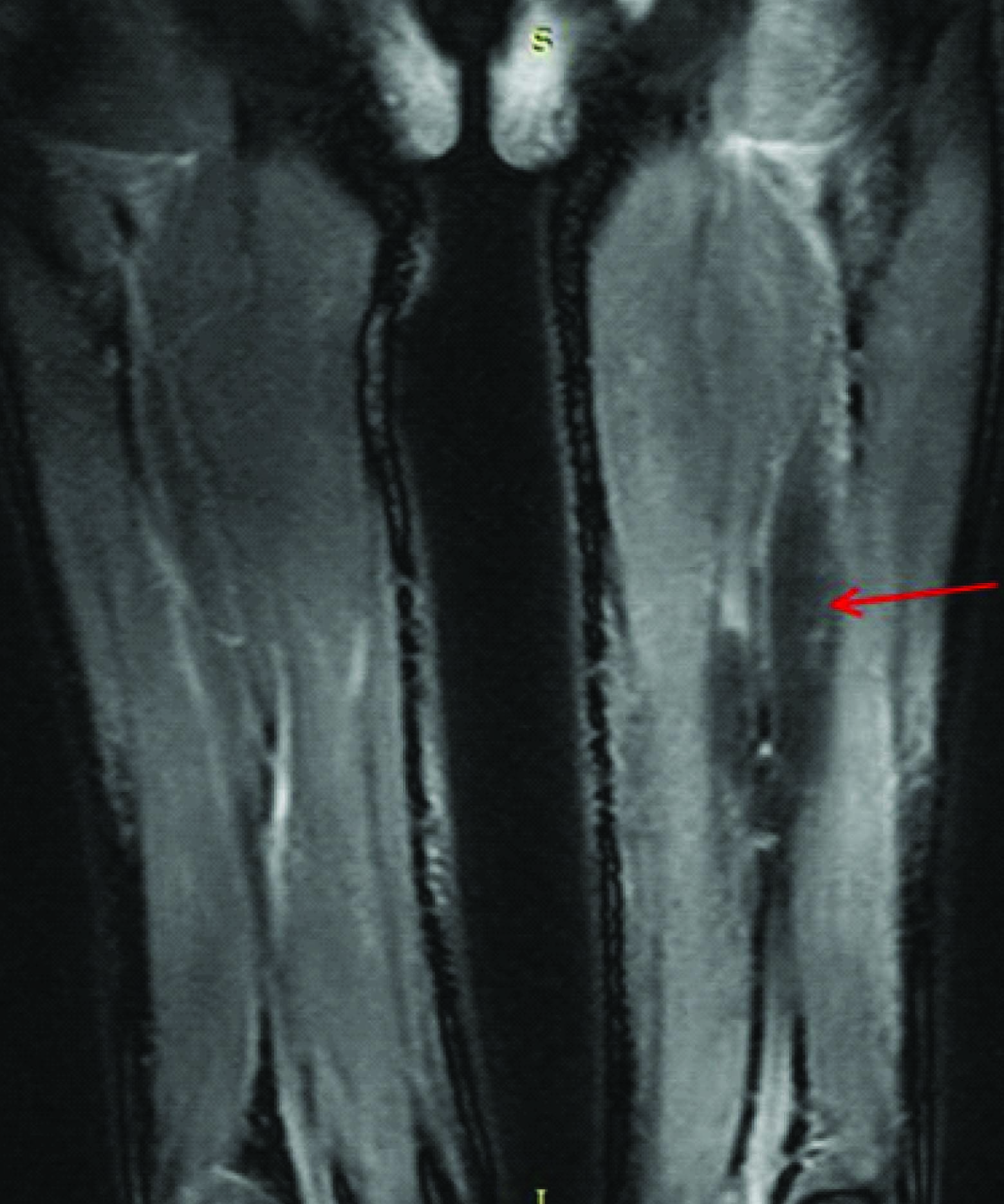
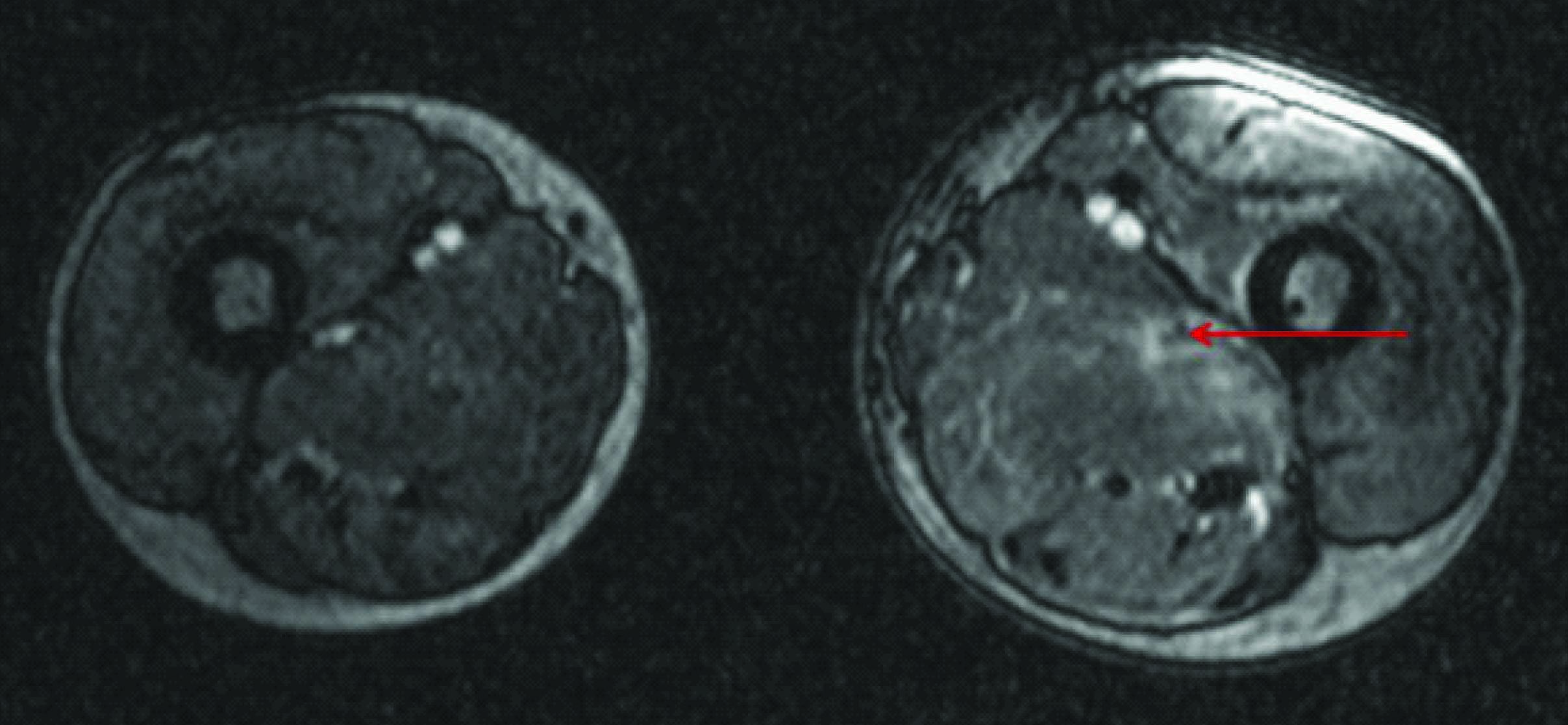
MRI of bilateral thighs was done to further characterize the calcifications and see any features of ongoing disease activity. Nodular and linear areas of T1,T2 dark signals blooming on gradient sequence seen in the muscles of posterior compartment of left thigh [Table/Fig-6a,b]. Hyperintensity seen in STIR images along muscle fibres of in left limb with variable patchy areas of enhancement on post contrast study [Table/Fig-6c].
CoronalT1WMR image shows calcifications as dark signal nodular masses in left thigh
Coronal STIR image shows calcifications (red arrow) as dark signal masses in left thigh with hyperintensity in muscle fibres suggest oedema
Axial Post contrast T1FS image shows patchy enhancement (red arrow) in the posterior compartment muscle of left thigh
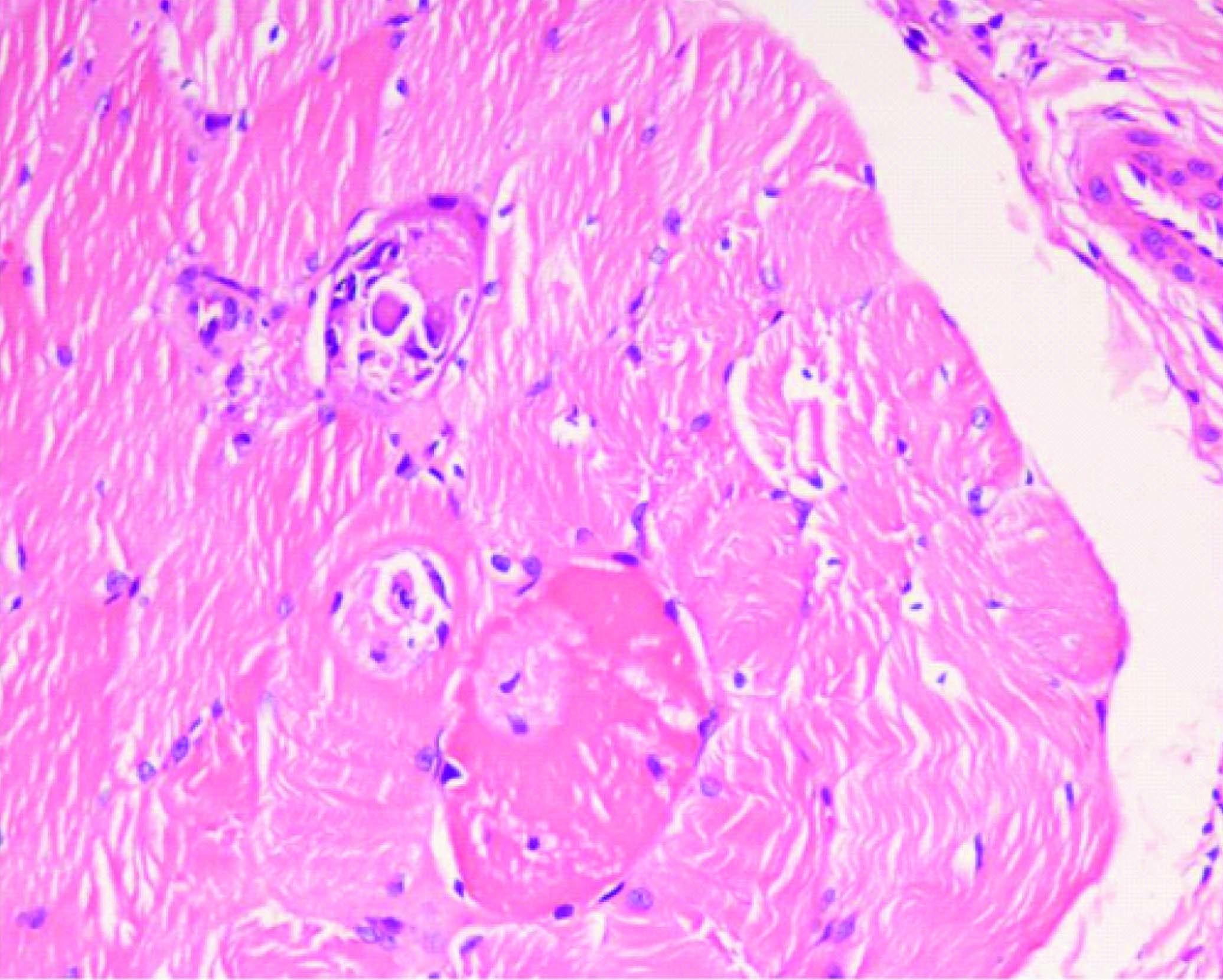
Histopathology from muscle biopsy revealed myophagocytosis with interfascicular and perivascular chronic inflammatory infiltrate and focal areas of endomysial inflammation [Table/Fig-7].
High power microscopy images show myophagocytosis with interfascicular and perivascular chronic inflammatory infiltrate and focal areas of endomysial inflammation
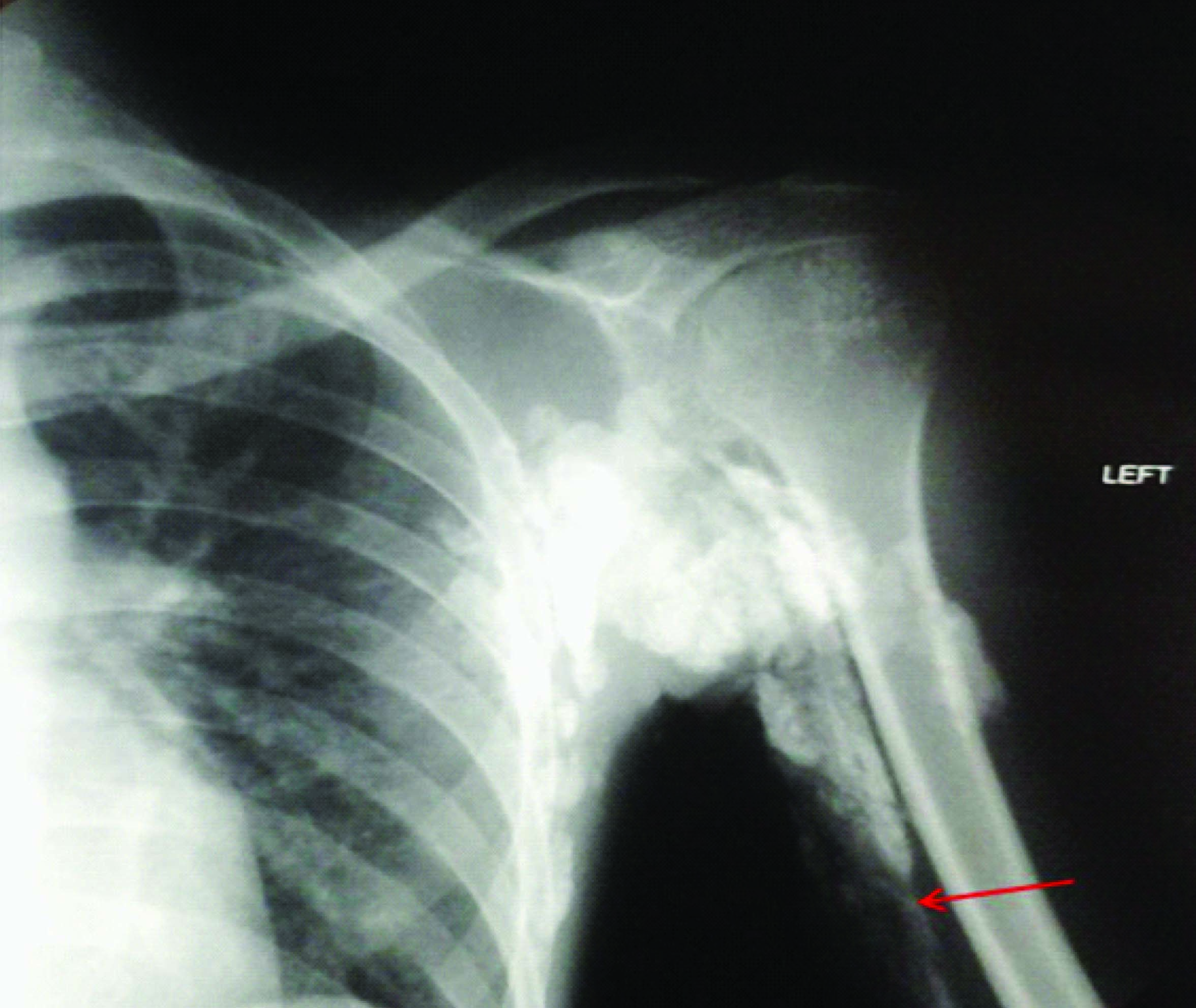
Patient was treated with high dose prednisolone with adequate hydration and Alendronate, a bisphosphonate was used to treat the calcifications. On one month follow up though patient’s power improved in all limbs (3/5 in lower and 4/5 in upper) and serum enzymes returned to normal levels [Table/Fig-2]. No significant change in calcifications was seen on imaging with development of joint contracture in bilateral shoulder joints. There was evidence of development of some more calcification in intramuscular plane seen on radiography of the left shoulder [Table/Fig-8] compared to the earlier X-ray [Table/Fig-3b].
One month follow up X-ray of left shoulder shows some more calcific plaques(red arrow) in deep muscular plane compared to [Table/Fig-3a]
Discussion
Juvenile dermatomyositis is a rare multisystemic autoimmune inflammatory disease involving the striated muscle and skin [1]. A variable incidence of JDM reported in different literatures across the globe with approximately 3.2 per million children under 16 y per year affected in USA and 1.9 per million children in UK and other European areas. Though most western literatures document a higher incidence in female population with female: male ratios reported from 2.3:1 to 5:1, in contrast Japan, India and Saudi Arabia show female to male ratio 1:1.3,1.7 [1–3]. Dermatomyositis has a bimodal distribution in the age of onset, occurring in two peaks, one at 5–14 y and the other at 45–64 y of life [4]. The diagnostic criteria was originally proposed by bolan and peter in 1975 remains the standard criteria for diagnosis [4].
An estimated 30-70% of children with JDM exhibit calcinosis [5,6] The pathological dystrophic calfications seen in chronic phase of the disease is more commonly seen in children and adolescents in comparison to adults affected with this disease [3,5,7]. Perifascicular destruction of muscles by CD4T cells due to activation of membrane attack complexes by autoantibodies against endothelial cells and subsequently lysosomal damage of tissues leading to release of alkaline phosphatase, which in turn acts on organic phosphates thus precipitating calcium deposits have been considered as the possible pathogenesis for calcinosis in these patients though exact aetiology is still unknown [1,6,8].
The disease course can be divided into an acute inflammatory phase and a chronic healing phase with varying episodes of remissions and relapses [8,9]. In the acute phase the radiographic features are those of myositis and oedema with obliteration of normal tissue planes and swelling of the muscles predominantly involving the thigh, arms, chest wall [9]. The earliest changes in acute phase are notably seen as patchy or diffuse areas of hyperintensity in the affected muscles on STIR sequence in MR with evidence of restriction on diffusion weighted sequence and variable enhancement on post Gadolinium administration.MRI thus helped us to localize the acutely inflamed muscles and hence guide biopsy.
Calcifications in JDM usually develop in the chronic phase at the sites of necrosis involving the skin, subcutaneous tissue, fascial planes and muscles [10]. Any cause of trauma or inflammation (like surgery) may precipitate calcinosis in the affected site in these group of patients [11] though such inciting factor was not present in our patient. In a particular limb the proximal muscles are more often involved with relative sparing of the distal muscles (unlike scleroderma) [7,10]. The location and extent of calcification varies proportionately to the site and severity of myositis seen in acute phase [10].
Calcinosis in JDM patients can cause more incapacity and complications than the myopathy itself [5]. Soft tissue calcification can be anywhere including superficial skin (calcinosis cutis), around joints (calcinosis circumscripta) or deep fascial planes (calcinosis universalis). There are four patterns of calcification described with dermatomyositis cases namely: superficial nodular/clump like calcific masses, deep calcareal masses, deep linear/sheet like calcifications within the fascial planes and a rare diffuse superficial lace like /reticular calcification which involves almost the entire body surface [6,12]. The last pattern has been linked with a chronic severe non remitting course in patients of dermatomyositis and needs to be differentiated from myositis ossificans progressive [12]. The calcinosis in dermatomyositis is essentially dystrophic calcification without formation of bone/ossification,hence no evidence of zoning is seen in these calcareal masses unlike in myositis ossificans progressive [13]. Superficial calcific masses may lead to non healing ulcer formations with extrusion of calcareal masses as seen in our case. In our patient joint contracture, chronic pain which developed subsequently is likely related to severe deep muscular and interfascial calcifications.
Though conventional radiography is ideal for imaging soft tissue calcifications, Ultrasound (USG) and Computed tomography (CT) are more sensitive in picking up early subtle calcification and specifically localizing the exact anatomical plane. 99m Tc MDP Scintigraphy has been reported to be more sensitive in assessing the total load of calcinosis and follow up of these patients [6].
A wide variety of drugs from bisphosphonates (like alendronate), calcium channel blockers (dilitazem) to high dose steroids have been used for treating calcinosis with variable results. Surgical removal, carbon dioxide laser have been used to remove larger chunks of calcifications [5,8].
The present article highlights the need and importance of radiography in diagnosis as well as screening of the disease by detecting soft tissue calcifications. The reasons for calcinosis are delay in diagnosis and initiation of treatment, longer duration of disease activity, polycyclic or unremitting course, local trauma, therapy refractoriness and poor treatment adherence [14]. Calcifications occur in JDM often within six months of onset and may go unnoticed by the patient. Calcinosis occurs in a significant proportion of young patients with dermatomyositis and increases with disease duration [15–17], hence the load of calcinosis on first radiography (when the child presents) can be used as an indirect evidence of the duration of the disease prior to diagnosis. Patients with a chronic polycyclic course of the disease tend to develop more diffuse calcinosis than those with monocyclic course, hence the extent and pattern of calcinosis also predicts the disease course and serve as an indirect evidence of prognosis [14,16]. Cutaneous ulceration signifies a poor prognosis in JDM. Given the fact that calcification is dystrophic in nature and most therapies aim at preventing further calcinosis but not resolving existing lesions [17], hence it cannot be a dynamic predictor of the variable disease course or the therapeutic response. However, Radiography can help to avoid delay in diagnosis of such patients as recognizing subtle cutaneous signs in Indian population and early muscle weakness in an already sick child may be challenging for the paediatrician. While muscle enzyme study and contrast enhanced MRI of the affected extremity determine ongoing disease activity, Radiography can be used as a baseline primary investigation and for future follow up to predict the long term course in our resource limited nation complementary to more invasive and costly investigations like muscle biopsy or EMG.
Conclusion
Though imaging is not primarily required for diagnosis, radiology plays an important role to rule out other important differential diagnoses, understanding and recognizing the different patterns of calcinosis in dermatomyositis patients will help to exclude other differentials. As calcinosis is proportionately related to the severeity of muscle damage, hence assessment of the total load of calcinosis is directly related to the chronicity of the disease process and can be used as a baseline for follow up imaging, besides the pattern of involvement in soft tissue planes is an indirect predictor for development of long term complications and morbidity in these patients .
List of Abbreviations:Hb=Haemoglobin,ESR=Erythrocyte sedimentation Rate,Ca= calcium, PO4=inorganic phosphate,Na=sodium,K-potassium,RBG=random blood glucose,LDH=Lactate dehydrogenase,AST/SGOT=Aspartate aminotransferase,ALT/SGPT=Alanine aminotransferase, CK=Creatine kinase(total),TSH=thyroid stimulating hormone,PTH=Parathyroid hormone
[1]. Faller Gail, Juvenile dermatomyositisCurrent Allergy & Clinical Immunology 2010 23(3):101 [Google Scholar]
[2]. Symmons DP, Sills JA, Davis SM, The incidence of juvenile dermatomyositis: results from a nation-wide studyBr J Rheumatol 1995 34:732-36. [Google Scholar]
[3]. Singh S, Bansal A, Twelve year experience of juvenile dermatomyositis in north IndiaRheumatol Int 2006 26:510-55. [Google Scholar]
[4]. Bohan A, Peter JB, Polymyositis and dermatomyositis [second of two parts]N Eng J Med 1975 292:403-07. [Google Scholar]
[5]. Zoilo Morel Ayala, Rogelio Martínez Ramírez, Samara Mendieta Zerón, Enrique Faugier Fuentes, Rocío Maldonado Velázquez, Juvenile Dermatomyositis and Extensive Calcinosis Treatment With Methylprednisolone and MethotrexateReumatol Clin 2008 4(6):248-50. [Google Scholar]
[6]. Agarwal Vikas, Sachdev Atul, Dabra Ajay Kumar, Calcinosis in Juvenile DermatomyositisRadiology 2007 242:307-11. [Google Scholar]
[7]. Kaliyadan Feroze, Venkitakrishnan S, Late onset calcification following juvenile dermatomyositis: response with weekly alendronateIndian J Dermatol 2011 56(3):357-59. [Google Scholar]
[8]. Brawnwald Fauci, Hauser Kasper, Jameson Longo, Loscalzo Harrison’s principles of internal medicine 2008 17th editionMc-Graw HillsNerve and Muscle disorders, Chapter 383 [Google Scholar]
[9]. Alicioglu B, Karakas HM, Firat AK, Magnetic Resonance Imaging of Muscular Involvement in Juvenile Dermatomyositis:Case ReportPrague Medical Report 2008 109(4):315-20. [Google Scholar]
[10]. Steiner Robert M, Glassman Leonard, Schwartz M William, Vanace Peter, The Radiological Findings in Dermatomyositis of ChildhoodRadiology 1974 111:385-93. [Google Scholar]
[11]. Presley Bradley C, Bush Jeffrey S, Watson Simon C, Dermatomyositis with Extensive Calcification in an AdultWestern Journal of Emergency Medicine 2012 XIII(1) [Google Scholar]
[12]. BIane Caroline E, White Susan J, Braunstein Ethan M, Bowyerı Suzanne L, Sullivan Donita B, Patterns of Calcification in Childhood DermatomyositisAJR 1984 142:397-400. [Google Scholar]
[13]. Dermatomyositis: Case of the Week 207[Internet], June 18,2006[updated April 2014, cited,May2014]. Available from:http://www.learningradiology.com/toc/tocsubsection/tocarchives2006.htm [Google Scholar]
[14]. Gleice Clemente, Daniela Gerent Petry, Piotto Cássia Barbosa, Octávio Augusto Peracchi, High frequency of calcinosis in juvenile dermatomyositis: a risk factor studyRev Bras Reumatol 2012 52(4):545-53. [Google Scholar]
[15]. Chickermane Pranav R, Mankad Deepali, Khubchandani Raju P, Disease Patterns of Juvenile Dermatomyositis From Western IndiaIndian Pediatrics 2013 50(10):961-63. [Google Scholar]
[16]. Demircin Gulay, Erdogan Ozlem, Bulbul Mehmet, Baysun Sahika, Calcinosis; a Difficult Problem in Juvenile DermatomyositisAnn Paediatr Rheum 2012 1(1):65-70. [Google Scholar]
[17]. Bowyer SL, Blane CE, Sullivan DB, Cassidy JT, Childhood dermatomyositis: factors predicting functional outcome and development of dystrophic calcificationJ Pediatrics 1983 103:882-88. [Google Scholar]