Non Traumatic Spinal Epidural Haematoma in a Woman with HELLP Syndrome: A Case Report
Juhi Bansal1, Ravishankar Pillenahalli Maheshwarappa2, Amit Gupta3, Alka Goyal4
1 Senior Resident, Department of Radio-diagnosis, Sawai Mann Singh Medical College, Jaipur, India.
2 Assistant Professor, Department of Radiodiagnosis, Adichunchanagiri Institute of Medical Sciences, Bellur, Karnataka, India.
3 Fellow in Neuroradiology, Department of Neuroradiology, University Hospitals Case Medical Center, Cleveland, Ohio.
4 Senior Resident, Department of Radio-diagnosis, Sawai Mann Singh Medical College, Jaipur, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ravishankar Pillenahalli Maheshwarappa, Room No. 24, Kalpataru Bhavan, Adichunchanagiri Institute of Medical Sciences, Bellur, Nagamangala taluk, Mandya, Karnataka, India. Phone : +919900767588, E-mail : ravi_spm@yahoo.co.in
Spinal epidural haematomas (SEH) is a potentially reversible cause of spinal cord and nerve root compression which needs prompt surgical decompression for satisfactory neurological recovery. SEH occurs very rarely in pregnant woman with HELLP syndrome (hemolysis, elevated liver enzyme levels, and low platelet levels). Most of the SEH cases reported in HELLP syndrome in the literature are due to iatrogenic interventions. We report a still rarer case of non traumatic spinal epidural haematoma in a pregnant woman with HELLP Syndrome.
HELLP syndrome, Non traumatic, Spinal epidural haematoma
Case Report
A 30-year-old pregnant female with 36 wk of gestation presented to the Department of Obstetrics with sudden onset of paraplegia and back pain. 12 h before her admission the patient experienced sudden onset of severe neck pain and progressive weakness in extremities along with sensory loss in her legs and torso which was not associated with any physical activity. She was on iron and vitamin supplementation. Her past medical history was unremarkable.
On admission, the patient’s neurological examination was remarkable for weakness in lower extremities. The patient had sensory loss in her lower extremities. On hematological testing, her platelet count was markedly reduced to 1.5 × 104 cells/μL. Liver function impairment was also detected (glutamic-oxaloacetic transaminase, 645U/L; glutamic- pyruvic transaminase, 284U/L; total bilirubin, 8.6 mg), while her lactate dehydrogenase and cytokeratin levels were elevated. HELLP syndrome was diagnosed based on the above laboratory test findings.
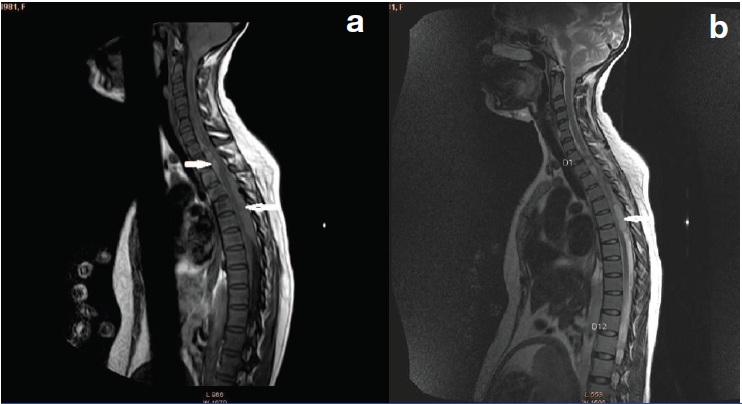
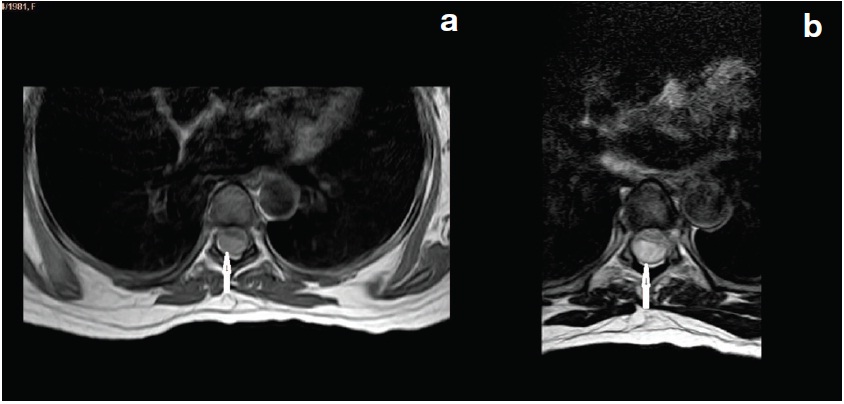
An emergency MRI scan was performed to assess her bilateral lower limb paralysis. Two space-occupying lesions were detected in her spinal canal, one in her lower cervical [Table/Fig-1a&b] and second one in her upper thoracic level [Table/Fig-2a&b]. The lesions were diagnosed as epidural hematomas based on the MRI findings at this time. Emergency caesarean section was performed to bring the pregnancy to an end on the same day. Later emergency decompression was performed and the diagnosis of epidural haematomas was confirmed. The weakness of her lower limbs improved gradually over few months. The patient was followed up for two years. No recurrence or residual weakness was found.
Sagittal T1W and T2W images show two space-occupying lesions in the epidural compartment of the spinal canal, one in the lower cervical and upper thoracic level, second one in the lower thoracic and lumbar region
On axial T1W images the lesion is isointense and on corresponding Axial T2W images [Table/Fig-2b] the lesion is hyperintense suggesting its hyperacute nature
Discussion
Spinal epidural hematoma (SEH) associated with pregnancy is a rare cause of spinal cord compression and spontaneous spinal epidural hematoma (SSEH) associated with pregnancy is even more uncommon. Haemorrhagic disorders such as hematoma were originally believed to not develop easily during pregnancy because blood coagulability is increased in pregnant women [1]. Because of its rarity and atypical symptoms, its prompt diagnosis is difficult and its aetiology remains unclear. There were few studies discussing the aetiology, presentation and treatment of spontaneous spinal epidural hematoma (SSEH) during pregnancy where the clotting profile was normal. There have only been nine previously published cases of SSEH occurring during pregnancy [1–3]. However in HELLP syndrome only one case of idiopathic spinal subarachnoid haematoma has been reported by Fujimaki et al., [4]. To our best knowledge ours is the first case report of idiopathic spinal epidural haematoma presenting in a pregnant woman with HELLP syndrome.
The most important aetiologies of SSEH are clotting disorders, which may be acquired (anticoagulant therapy, haematological malignancies) or congenital (haemophilia). Vascular malformations are rarely responsible for SSEH (4% in a series of 158 cases and 6.5% in a series of 199 cases). In about 40-50% cases however no cause could be identified [5,6]. Other less common predisposing factors for SSEH include: systemic lupus erythematosus, ankylosing spondylitis, rheumatoid arthritis, Paget’s disease, disc herniation and hypertension. The hypothesis for the pathogenesis of SSEH is rupture of epidural veins situated in the low-pressure epidural space secondary to sudden increases in intra-abdominal or intrathoracic pressure; this is usually associated with bleeding disorders [7]. The aetiology of SSEH during pregnancy (a state of hypercoagulability) remains unclear. The changes in hemodynamics during pregnancy may increase epidural venous pressure and cause rupture and hemorrhage [1,2].
The first symptom of SSEH is usually severe localized back pain, often with a radicular component. The onset of pain is occasionally related to minor straining such as defecation, lifting, coughing or sneezing, but in majority of cases the onset of pain is spontaneous. Signs of spinal cord and nerve root dysfunction appear rapidly and may progress to paraparesis or tetraparesis, depending on the level of the lesion. When neurological abnormalities develop, MRI of the spinal cord and a coagulation profile should be performed [3]. MRI is recommended for identifying the level of injury, presence of haemorrhage and oedema, and degree of cord compression [8]. The most appropriate treatment is emergency caesarean section under spinal anaesthesia. The anaesthesia of choice for caesarean section is combined spinal epidural anaesthesia [9]. This should be followed by with surgical decompression of the spinal cord [2,3]. If the condition is not promptly treated in time permanent neurological deficits can occur. Cases of Brown-Sequard syndrome have also been described [10].
Postoperatively, a rehabilitation specialist should be involved in establishing the rehabilitation objectives and plans to ensure optimal recovery
Conclusion
Non traumatic spontaneous spinal epidural haematoma rarely occurs in pregnant women with HELLP syndrome. Imaging plays a major role in the early diagnosis of this condition. Emergency caesarean section followed by evacuation of the haematoma is the treatment of choice.
Consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
[1]. Carrol SG, Malhotra R, Eustace D, Sharr M, Morcos S, Spontaneous spinal extradural hematoma during pregnancyJ Matern Fetal Med 1997 6:218-19. [Google Scholar]
[2]. Jea A, Moza K, Levi AD, Vanni S, Spontaneous spinal epidural hematoma during pregnancy: case report and literature reviewNeurosurgery 2005 56:1156-60. [Google Scholar]
[3]. Kelly ME, Beavis RC, Hattingh S, Spontaneous spinal epidural hematoma during pregnancyCan J Neurol Sci 2005 32:361-65. [Google Scholar]
[4]. Fujimaki H, Nakazawa T, Ueno M, Imura T, Saito W, Takahira N, Spinal subarachnoid hematoma in a woman with HELLP syndrome: a case reportJ Med Case Rep 2012 6(1):152doi: 10.1186/1752-1947-6-152 [Google Scholar]
[5]. Kong JK, Mak KH, Spontaneous spinal epidural haematoma--an unusual cause of spinal cord compressionHong Kong Med J 2003 9(1):55-57. [Google Scholar]
[6]. Chen C, Fang W, Chen C, Spontaneous spinal epidural hematomas with repeated remission and relapseNeuroradiology 1997 39:737-40. [Google Scholar]
[7]. Lonjon MM, Paquis P, Chanalet S, Grellier P, Nontraumatic spinal epidural hematoma: report of four cases and review of literatureNeurosurgery 1997 41:483-86. [Google Scholar]
[8]. Neuroimaging CommitteeNeuroimaging in traumatic spinal cord injury: an evidence-based review for clinical practice and researchJ Spinal Cord Med 2007 30:205-14. [Google Scholar]
[9]. Dhama SS, Malhotra S, Kumar M, Jain G, HELLP Syndrome - A Therapeutic Challenge – Case Report With Review of LiteratureNational Journal of Medical and Dental Research 2013 1(3):62-65. [Google Scholar]
[10]. Mahieu X, Kridelka F, Pintiaux A, Hematome extradural spontane de la femme enceinteJ Gynecol Obstet Biol Reprod 1994 23:99-102. [Google Scholar]