Introduction and Objectives: Strokes are caused by disruption of the blood supply to the brain. This may result from either blockage or rupture of a blood vessel. Yearly 15 million people worldwide suffer a stroke. India ranks second worldwide in terms of deaths from stroke. The incidence of stroke increases with age affecting the economically productive middle aged population. Hypertension and male sex are other risk factors for stroke.
C-Reactive Protein (CRP) is an acute phase protein whose concentration rises in blood following inflammation. Formerly, assays for CRP detected its rise only after significant inflammation. However, recently developed high sensitivity assays (hsCRP) enable the measurement of CRP in individuals who are apparently healthy. Several studies indicate that hsCRP is elevated in individuals who are at risk of developing Coronary Artery Disease or Cerebrovascular events, the elevation may be found years before the first detection of vascular problems.
In the absence of other biochemical markers, the present study aimed to evaluate the predictive and diagnostic role of hsCRP in stroke.
Materials and Methods: The study consisted of 50 patients of acute stroke admitted in Gauhati Medical College and Hospital. The control population consisted of two groups – 50 age and sex matched controls with hypertension (Hypertensive control group) and 50 age and sex matched controls with no obvious disease constituted the Normal control group. hsCRP levels were measured in all the groups and compared statistically.
Conclusion: hsCRP is an acute phase reactant whose concentration rises in stroke as well as in those at risk. The rise may be identified even before the appearance of risk factors. Hence, hsCRP may be useful as a predictive and diagnostic marker in stroke.
Introduction
Apoplexy- Dated unconsciousness or incapacity resulting from a cerebral haemorrhage or stroke [1]. In modern times, the term ‘Apoplexy’ has been largely replaced by the term ‘Stroke’. For all practical purposes, Apoplexy and Stroke refer to the same condition.
Most cerebrovascular diseases are manifested by the abrupt onset of a focal neurological deficit. The WHO has defined stroke as “rapidly developing clinical signs of focal (at times global) disturbance of cerebral function, lasting more than 24 h or leading to death with no apparent cause other than that of vascular origin” [2]. Such terms defined by the duration of neurologic symptoms are being redefined with the more widespread use of sensitive brain imaging. Hence, the most recent definition of stroke for clinical trials requires either symptoms lasting more than 24 h or imaging of an acute clinically relevant brain lesion in patients with rapidly vanishing symptoms. The definition of stroke is thus clinical and laboratory and imaging studies serve to support the diagnosis.
Annually 15 million people worldwide suffer a stroke. Of these, 5 million die and another 5 million are left permanently disabled [3]. India ranks second worldwide in terms of deaths from stroke. According to the Indian Council of Medical Research, there were 930,985 cases of stroke in 2004 in India with 639,455 deaths [4].
Stroke occurs predominantly in the middle and late years of life. Age is the strongest determinant of stroke [3]. Several other factors are known to be risk factors for stroke. The most important among these are hypertension, atrial fibrillation, diabetes mellitus, cigarette smoking and hyperlipidemia. After age, the second most powerful, modifiable risk factor is hypertension.
The past decades have witnessed a major reassessment of our perception of acute stroke. A consensus has emerged that inflammation plays a decisive role in the pathophysiology of acute cerebrovascular accidents.
Ever since its discovery by Tillett and Francis in 1930 [5,6], C-Reactive Protein (CRP) has been accepted as a marker of inflammation. Recently developed high sensitivity assays for CRP (hsCRP) have made it possible to assess CRP levels in apparently healthy individuals. CRP has been observed to be related to the risk of cerebrovascular events [7-9] and is consistently elevated in circulation of patients after acute stroke, even when factors known to be associated with raised CRP concentrations such as infection and atherosclerosis are excluded [10-12]. CRP and hsCRP signify the same biochemical molecule but it is important that a physician request a “high-sensitivity” test or hsCRP if he or she is using CRP for the purpose of risk assessment. This is because older tests for CRP, which are adequate for monitoring severe inflammatory conditions, do not have the ability to measure levels accurately within the range needed for stroke risk detection and prediction. Stroke risk prediction is based on conventional markers such as measurement of blood pressure, assessment of lipid profile. A point of care test that helps in prediction of risk in those who are apparently healthy and also helps in diagnosis of acute stroke in those who have suffered one is still to be found. Such a test would go a long way in decreasing the time spent in diagnosis of stroke as well as serve as a screening tool for prediction. Such a marker is of immense importance in the field of public health, more so in India which has the world’s second largest population.
A few studies done so far have shown that serum concentration of hsCRP is significantly high in patients with acute stroke as compared to normal subjects [10-12]. But there have been no studies to evaluate the role of hsCRP as a predictive marker for acute stroke. The present study aimed to analyse the role of hsCRP as a predictive marker for stroke.
Materials and Methods
The study consisted of a total of 150 participants. The participants were divided into three Groups. The Stroke Group consisted of 50 patients of acute stroke admitted in the Departments of Medicine and Neurology of Gauhati Medical College and Hospital, Assam, India, between July 2011 and June 2012. The control population consisted of two groups – 50 age and sex matched controls with hypertension which constituted the Hypertensive control group and 50 age and sex matched controls with no obvious disease which constituted the Normal group. The Hypertensive controls were recruited from the Department of Cardiology, Gauhati Medical College and Hospital and the normal controls were randomly drawn from the general population. Individuals with traumatic intracranial haemorrhage, intracranial infections and tumours, those with history of recent clinical infections, major renal, hepatic diseases and those with Diabetes Mellitus were excluded from the study.
Diagnosis of stroke was based on history, clinical evaluation and evidence of stroke on CT scan (Brain). All cases presenting within 72 h of onset of symptoms were included in the study.
Five ml of blood sample was drawn from the participants under aseptic conditions from the median cubital vein. It was collected in properly labelled vacutainers and then centrifuged at 3000 rpm for 15 min. The serum thus obtained was subjected to biochemical analysis within 8 h of collection of blood.
Estimation of serum hsCRP was done in Vitros 5600 Integrated System Autoanalyzer employing Latex Enhanced Immunoturbidimetric Assay [13]. The reagent pack consisted of dual chambered ready to use liquid reagents. Samples are mixed with Reagent 1 containing a buffer. Addition of anti-CRP antibodies coupled to latex microparticles (Reagent 2) produced an immunochemical reaction yielding CRP Antigen-Antibody complexes. The turbidity produced was measured spectrophotometrically at 660 nm after incubating at 37ºc for 8 min.
Ethics
The study was approved by the Institutional Ethics Committee, Gauhati Medical College and Hospital and informed, written consent was obtained from all the participants in the study or from immediate family members in case of the stroke patients.
Statistical Analysis
All data were expressed as Mean ± SD. One-way ANOVA was performed to evaluate whether the difference in the mean hsCRP levels of the three respective groups was significant or not. p-value of less than 0.05 was considered to indicate statistical significance. Statistical analysis was performed using IBM SPSS Statistics Program Version 20.0.0.
Results
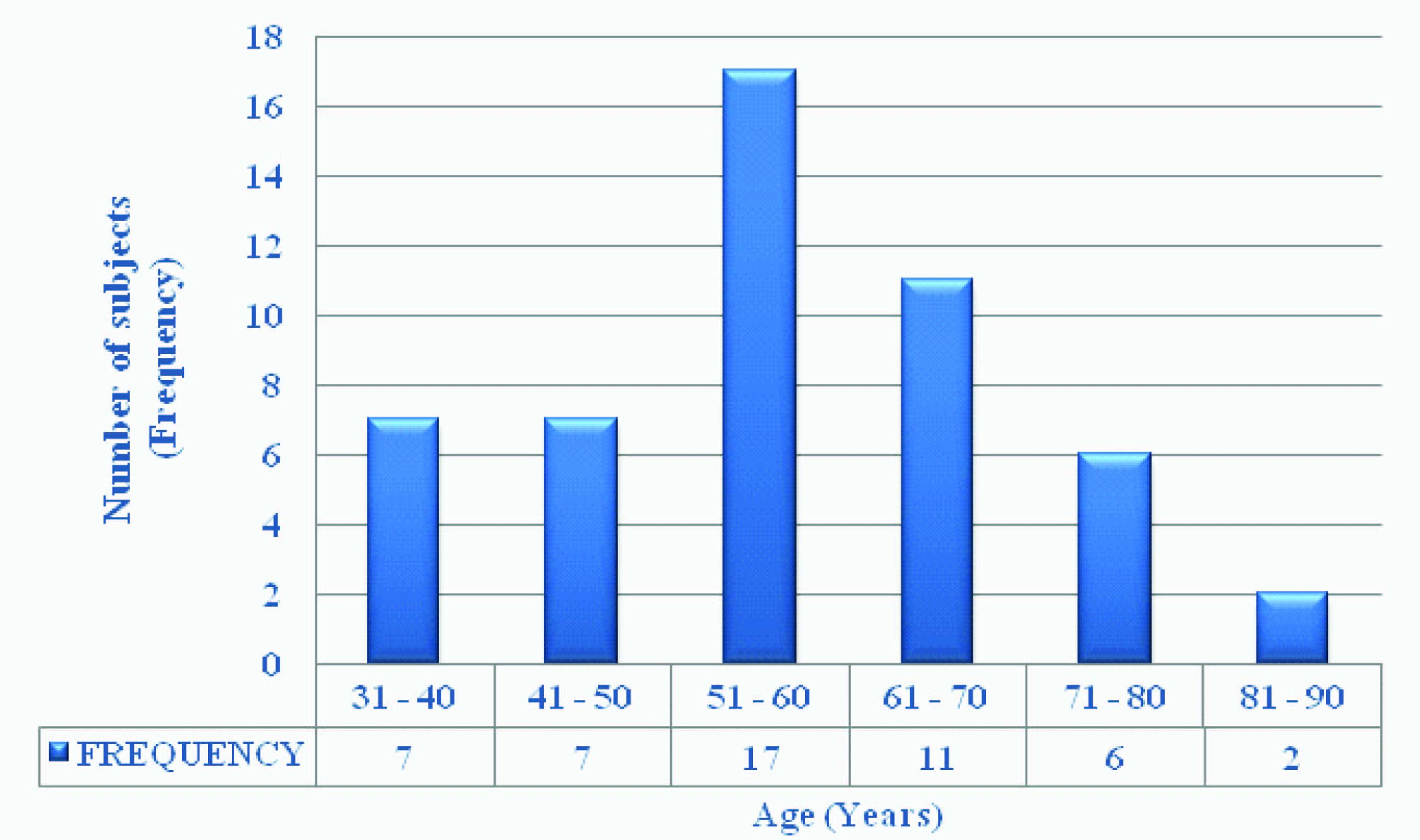
Demographic profile of stroke patients: The mean age of stroke patients was 58 y. The highest frequency of stroke incidence was found in the 51–60 y age group. The incidence in males was higher than in females (Male: Female Ratio - 34:16) [Table/Fig-1,2].
Blood Pressure levels in the three groups under study: Stroke patients showed significantly elevated Blood Pressure levels as compared to that of Hypertensive controls and of Normal controls. The variation in Blood Pressure among the three groups was statistically significant (p < 0.0001) [Table/Fig-3].
Serum hsCRP levels in the three groups under study: [Table/Fig-4] show the statistical distribution of hsCRP levels in the three groups studied. The mean hsCRP levels showed a statistically significant elevation (p<0.0001) in both hypertension and stroke when compared to that in normal controls.
Discussion
Stroke is fast emerging as a major public health problem in India as it produces an enormous burden on the economy of the country. There is increasing evidence that stroke incidence rates in developing countries have increased by more than 100% during the last four decades, while they have decreased by 42% in developed countries over the same time. In a period of four decades, stroke incidence rates increased from 52 per 100,000 person-years (1970- 1979) to 117 per 100,000 person-years (2000-2008) in developing countries. On the other hand, stroke incidence rates decreased from 163 per 100,000 person-years (1970-1979) to 94 per 100,000 person-years (2000-2008) in developed countries [14]. This reflects a shift in the earlier notion that cerebrovascular diseases were more prevalent in the relatively more affluent parts of the world than in the relatively less affluent parts. This new insight into the incidence and prevalence of cerebrovascular diseases is significant because the developing countries encompass a majority of the population of the world and are still lagging behind in the quality of health care and rehabilitation services and this very cause may play an important role in the higher incidence and prevalence seen in this situation.
Elkind et al.,[3] in Merritt’s Neurology have mentioned that the strongest determinant of stroke is age. The findings of the present study were in corroboration with a study by Talreja Mishra et al., [12] (age distribution 30 – 90 y, mean age 59 y) and another study by Wang et al., [15] (mean age 61.01 ± 0.42 for ischemic and 57.58 ± 0.75 y for haemorrhagic stroke). Similarly, risk profile studies from the Framingham Study undertaken by Wolf et al., [16] have shown that the 10 y probability of stroke was higher in men than in women (9.6% versus 6.5%). The findings of the present study are similar to those from the above studies.
The rising incidence of stroke associated with advancing age is due to the increased prevalence of atherosclerosis and hypertension in the middle-aged Indian population.
Men have a higher incidence of stroke as is evident from the present study. This may be ascribed to a number of factors. Firstly, the reason might be the positive effects of oestrogen on the cerebral circulation [17], in case of females. A second factor may be blood pressure. A study by Reckelhoff [18] has shown that blood pressure values are higher in men than women of similar ages.
In the present study, the average blood pressure of the patients was 160/90 mm Hg, which was statistically significantly high as compared to that in normal age and sex-matched controls as well as that in the hypertensive age and sex-matched controls. This signifies that increased blood pressure may be a risk factor in the aetiology of stroke. The existence of hypertension as a risk factor for development of stroke has been stressed upon by many researchers. Hadjiev et al.,[19] have found a high incidence of hypertension in stroke patients (65.8%, p = 0.0293) in a study comprising 500 volunteers followed up for two years. Similarly, Hart et al., [20] in their 20 y follow up study of men and women in Scotland have reported an extremely significant association (p<0.0001) between hypertension and stroke risk. The findings of the present study tally with those of the previous studies.
Hypertension is a central risk factor for cerebrovascular events. Basic data suggest that increasing levels of blood pressure may stimulate a proinflammatory response and that endothelial inflammation may also herald the changes in arterial wall that characterize the hypertensive state. Hypertension, at least in the case of intracerebral haemorrhage, may lead to spontaneous rupture of a small penetrating artery deep in the brain. The small arteries seem most prone to hypertension-induced vascular injury. Hypertension also accentuates the progression of atherosclerosis that has an inflammatory component which plays an integral role in the pathogenesis of stroke [21].
In the present study, it was found that the level of hsCRP in stroke patients was significantly high (p<0.0001) when compared to that in hypertensive controls and in normal controls. Elkind et al., [10] in their study of levels of acute phase reactants in stroke have found that levels of hsCRP were significantly higher in stroke patients than in stroke-free patients (p<0.05). Moreover, there was no evidence of a time trend in levels of hsCRP during 28 d of follow-up of stroke patients. It thus appears that if levels of hsCRP increase at the time of stroke, they remain elevated for at least one month. This finding is also corroborated by Soliman et al., [11] who observed in their study that there was a highly significant increase in serum hsCRP level in the first 48 h after stroke onset. Similar observations of elevated hsCRP levels have also been reported by Talreja Mishra et al.., [12] in their study, who found a highly significant increase in level of hsCRP (p<0.001) in 40 patients with stroke than in normal age and sex-matched subjects. In a prospective case-referent study Andersson et al., [9] demonstrated that hsCRP, divided into three groups, i.e. <1mg/L – Low Risk, 1 to 3 mg/L – Average Risk and >3 mg/L – High Risk, is significantly associated with the risk of firstever stroke. This finding is significant because this establishes the first ever reference range for hsCRP in relation to cerebrovascular risk assessment.
Despite a decade of intense public education and medical advancement, stroke continues to represent a leading cause of long-term disability and death. A major obstacle to the appropriate treatment of patients with suspected stroke is rapid entry into a care pathway that expedites the initial clinical examination and diagnostic testing requisite for initiating early management strategies. Although most diagnostic approaches for the evaluation of acute stroke rely on neuroimaging techniques, an alternative strategy would be the evaluation of blood-borne biochemical markers of tissue injury. This approach has precedence in the triage and early management of other urgent medical conditions [22].
A point-of-care test that measures biochemical markers of cerebral ischemia could be cost- and time-saving in comparison with neuroimaging techniques currently being investigated. There are recently developed and more sensitive methods of neuroimaging for diagnosis of stroke. But they, at the same time, consume a lot of time or are available at academic institutions or specialized stroke centers. In the community setup, a physician has to take split second decisions on whether to treat a suspected stroke patient with thrombolytics or transfer the patient to a hospital with stroke unit. A blood test to diagnose stroke will go a long way in helping the physician to take such decisions. As an added benefit, if the same blood test can foretell the chances of having a stroke in a person who is apparently healthy, then that test can be used as a screening tool for prediction of stroke in the community.
Distribution profile of stroke patients into different categories
| Categories | Stroke Patients |
|---|
| Total Cases | 50 |
| Sex | Males | 34 |
| Female | 16 |
| Mean Age (Years) | 58 |
| Range (Years) | 32 – 86 |
| Standard Deviation (Sd) | 13.21 |
| Ischemic Stroke | 36 |
| Haemorrhagic Stroke | 14 |
Frequency distribution of stroke patients according to age
Distribution of mean blood pressure (Mean ± SD) levels in normal controls, hypertensive controls and stroke cases
| Normal | Hypertensive | Stroke | p Value |
|---|
| Systolic | 112.84 ± 5.45 | 145.32 ± 12.15 | 159.72 ± 12.20 | < 0.0001 |
| Diastolic | 73.88 ± 3.73 | 85.4 ± 4.85 | 90.24 ± 6.22 | < 0.0001 |
Statistical distribution of hsCRP levels (mg/L) in normal controls, hypertensive controls and stroke patients
| Group | Number of Cases | Mean ± SD | Median | Min | Max | 95% Confidence Interval |
|---|
| from | to |
|---|
| Normal | 50 | 1.143 ± 0.725 | 1.13 | 0.1 | 3.51 | 0.9364 | 1.349 |
| Hypertensive | 50 | 8.181 ± 2.539 | 8.695 | 2.12 | 13.27 | 7.459 | 8.903 |
| Stroke | 50 | 40.8 ± 11.06 | 40.02 | 18.02 | 69.63 | 37.653 | 43.946 |
| p value | < 0.0001 | |
Limitation
A limitation of the present study was the inability to follow up those subjects with risk factors for stroke who had an elevated hsCRP. Also there was no hsCRP estimation done in patients before the occurrence of stroke. Hence, we hope that the present study will encourage further studies on the topic in a bigger way.
Conclusion
In conclusion, we would like to state that a biochemical test for the prediction and diagnosis of stroke is the need of the hour. From the study, it can be reported that there is a significant elevation of hsCRP in stroke as well as in those with risk of stroke. This rise can be traced back to the first appearance of risk factors of stroke.
[1]. New Oxford Advanced Learners’ Dictionary 2010 7th EditionApoplexyOxford: Oxford University Press:59 [Google Scholar]
[2]. J Mackay, GA Mensah, A Watts, M Addy, The Atlas of Heart Disease and Stroke. Geneva: World Health Organization in collaboration with Centers for Disease Control and Prevention USA 2004 :19-81. [Google Scholar]
[3]. MSV Elkind, RL Sacco, Pathogenesis, Classification, and Epidemiology of Cerebrovascular Disease. In: Rowland LP, Pedley TA, editors. Merritt’s NeurologyTetracyclineTeratology 2010 12th EditionPhiladelphiaLippincott Williams & Wilkins [Google Scholar]
[4]. K Prasad, D Vibha, Meenakshi JJ Hefferren, Cerebrovascular disease in South Asia - Part I: A burning problemJ R Soc Med Cardiovasc Dis 2012 1(20):1-7.doi:10.1258/cvd.2012.012025 [Google Scholar]
[5]. WS Tillet, T Francis, HO Heymann, Serological reactions in pneumonia with a nonproteinfraction from pneumococcusJ Exp Med 1930 52:561-71. [Google Scholar]
[6]. EB Oliveira, EC Gotschlich, TY Liu, Primary structure of human C-reactive proteinProc Natl Acad Sci USA 1977 74(8):3148-51. [Google Scholar]
[7]. M Di Napoli, MSV Elkind, DA Godoy, P Singh, F Papa, AP Wagner, Role of C-reactive protein in Cerebrovascular DiseaseExpert Rev Cardiovasc Ther 2011 41(12):1565-84. [Google Scholar]
[8]. Y Wakugawa, Y Kiyohara, Y Tanizaki, M Kubo, T Ninomiya, J Hata, C-Reactive Protein and Risk of First-Ever Ischaemic and Haemorrhagic Stroke in a General Japanese Population – The Hisayama StudyStroke 2006 37:27-32. [Google Scholar]
[9]. J Andersson, L Johansson, P Ladenvall, PG Wiklund, B Stegmayr, C Jer, C-Reactive Protein is a Determinant of First-Ever Stroke: Prospective Nested Cross-Referent StudyCerebrovasc Dis 2009 27:544-51. [Google Scholar]
[10]. MSV Elkind, K Coates, W Tai, MC Paik, B Boden-Albala, RL Sacco, Levels of acute phase proteins remain stable after ischemic strokeBMC Neurology 2006 6:37-43. [Google Scholar]
[11]. RH Soliman, NA Abdel-Monem, AA Helmy, SA El-Shafy, High Sensitivity C-Reactive Protein and its Gene Polymorphism in Acute Ischemic Strokethe Egyptian Journal of Neurology, Psychiatry and Neurosurgery 2010 47(1):373-79. [Google Scholar]
[12]. P Talreja Mishra, R Chandra, SK Saxena, R Jain, A Bhuyan, High Sensitivity C-Reactive Protein (hsCRP) Level in Cerebrovascular Accident (Stroke) Journal Indian Academy of Clinical Medicine 2010 11(3):204-07. [Google Scholar]
[13]. High- Sensitivity C-Reactive Protein. REF 6801739. [products insert]. Buckinghamshire UKOrtho-Clinical Diagnostics 2008 [Google Scholar]
[14]. World Heart Federation [Online].2010. [Cited 2010 Jun 19] Available from: URL http://www.worldheart.org/ [Google Scholar]
[15]. Q Wang, H Ding, J Tang, L Zhang, Y Xu, W Wang, C-Reactive protein polymorphisms and genetic susceptibility to ischemic and hemorrhagic stroke in the Chinese Han populationActa Pharmacol Sin 2009 30(3):291-98. [Google Scholar]
[16]. PA Wolf, RB D'Agostino, AJ Belanger, WB Kannel, Probability of stroke: a risk profile from the Framingham StudyStroke 1991 22:312-18. [Google Scholar]
[17]. DN Krause, SP Duckles, DA Pelligrino, AK Shetty, Influence of sex steroid hormones on cerebrovascular functionJ Appl Physiol 2006 101:1252-61. [Google Scholar]
[18]. DI Hadjiev, PP Mineva, MI Verkov, Multiple modifiable risk factors for first ischaemic stroke: A population-based epidemiological studyEuropean Journal of Neurology 2003 10:577-82. [Google Scholar]
[19]. DI Hadjiev, PP Mineva, MI Verkov, Multiple modifiable risk factors for first ischaemic stroke: A population-based epidemiological studyEuropean Journal of Neurology 2003 10:577-82. [Google Scholar]
[20]. CL Hart, DJ Hole, GD Smith, Comparison of Risk Factors for Stroke Incidence and Stroke Mortality in 20 Years of Follow-up in Men and Women in the Renfrew/ Paisley Study in ScotlandStroke 2000 30:1893-96. [Google Scholar]
[21]. AG Thrift, RG Evans, GA Donnan, Hypertension and risk of intracerebral haemorrhage: Special considerations in patients with renal diseaseNephrol Dial Transplant 2009 14:2291-92. [Google Scholar]
[22]. AK Saenger, RH Christenson, Stroke Biomarkers: Progress and Challenges for Diagnosis, Prognosis, Differentiation and TreatmentClin Chem 2010 190(1):21-33. [Google Scholar]