Psychological Evaluation of Patients in Critical Care/Intensive Care Unit and Patients Admitted in Wards
Gaurav Sharma B1, Maben EVS2, Kotian MS3, Ganaraja B4
1 Student, AJ Institute of Medical Sciences and Research, Kuntikana, Mangalore, India.
2 Professor & HOD, Department of Medicine, AJ Institute of Medical Sciences and Research, Kuntikana, Mangalore, India.
3 Associate Professor, Department of Community Medicine, Kasturba Medical College, Manipal University, Mangalore, India.
4 Additional Professor, Department of Physiology, Kasturba Medical College, Manipal University, Mangalore, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ganaraja B, Additional Professor, Department of Physiology, Kasturba Medical College, Centre For Basic Sciences, Manipal University, Mangalore, India. Phone : 00919449642150, E-mai : ganaraj.b@gmail.com
Background: Psychological assessment for depression, anxiety and stress among ICU patients and the patients admitted to ward in a hospital in India. This aspect did not get much attention in India so far. Such studies were common in developed countries. Therefore we decided in this study, to analyse the psychological status responses from the hospitalised patients in Mangalore using a validated questionnaire.
Aim: To assess and compare the depression, anxiety and stress Scores from the patients admitted in Intensive Care Unit (ICU) and those admitted to ward.
Materials and Methods: Eighty patients admitted to hospital, 40 from ICU and 40 admitted to ward were recruited. They were explained the procedure and after taking an informed consent, they were administered Depression, Anxiety, Stress Scale (DASS) Questionnaire, which contains 42-item questionnaire which includes three self-report scales designed to measure the negative emotional states of depression, anxiety and stress. The responses were computed and tabulated. We analysed the responses with Student’s t-test and Chi-square test, p<0.05 accepted as statistically significant.
Results: The results revealed significantly elevated stress, depression and anxiety among the ICU patients when compared to those in the ward (p<0.001). Above normal anxiety and stress levels were also seen in the ward patients, compared to the scores in normal range. 50% and 25% respectively showed mild and normal depression scores in ward patients, compared to 12% and 5% in those admitted to ICU. This trend was also true for Anxiety and stress scores.
Conclusion: From the results we found that there were elevated depression, anxiety and stress levels among the patients and this was significantly higher in ICU patients. Various factors could influence the psychological wellbeing of the patients, including the hospital environment, care givers, presence of family members nearby apart from the seriousness of illness, apprehensions about possibility of death. Such studies were rare among Indian patients. The findings of this study could be useful in incorporating suitable psychological help to the patients in hospitals to improve their recovery and wellbeing.
Anxiety, Depression, Intensive care unit, Indian hospital, Stress
Introduction
Psychological states such as depression, stress and anxiety among the patients in Intensive care unit (ICU) were well known factors which often affected the outcome of treatment. Long term studies reported that prolonged stay in ICU could have an adverse psychological sequel on patients [1,2], which can last long after the recovery. A study showed high Post-traumatic Stress disorder (PTSD) in patients who stayed for more than four days in ICU [3].Svenningsen H [4] had reported fluctuations in the level of sedation of patients in the ICU increased the incidence of delirium, but the delirium did not affect the risk of PTSD, anxiety, or depression. However, these parameters were affected by the type of memories the patients had. Therefore anxiety, depression could affect the quality of life among patients following recovery.
Delirium is another complication among the patients admitted to ICU [5], which was reportedly positively influenced by shifting to step down ICU, showing beneficial findings [6]. The disabilities and depression among ICU patients continuing even after the discharge and recovery form critical illness was a function of severity of illness and the duration of stay in ICU [7]. It has been established that the family members of the ICU patients too were subjected to adverse stress related issues [8,9]. Pillai et al., have reported PTSD symptoms among the relatives caring the ICU patients from India [10].
Several studies have reported the effects of altered sleep patterns and sleep quality in the ICU patients, which are bound to have a repercussion on the other psychological parameters [11–13].
Therefore, a systematic analysis of the psychological impact of diseases which involve admission to ICU and long term treatment, on the patients could be very useful for the care givers. Studies on depression, anxiety, Post traumatic stress disorders and other such studies on patients as well as the patient family members were carried out in advanced countries [14–16].
In Indian conditions this type of study on ICU patients has not been reported so far. Following a detailed survey of literature, we decided to take up this study on a small group of patients admitted into ICU. In the present study we used the Depression Anxiety and Stress Scale (DASS) self reporting questionnaire [17], which has been well validated and found to reliable in assessing the Depression, anxiety and stress among patients admitted in ICU [18]. Since studies on depression, stress and anxiety from ICU patients have been rare in India, this study reports, for the first time, and compares the DASS scores of patients admitted to ICU and ward in a hospital of South India. The results of this study reveal significantly elevatedpsychological distress among the ICU patients.
Materials and Methods
Total number of 80 subjects, 40 of them from the patients admitted to ICU and other 40 from the patients admitted to the ward (at AJ Institute of Medical Sciences and research centre, Mangalore), were randomized and the DASS questionnaire was administered after explaining the study protocol to the subjects. A signed informed consent was obtained from each subject before they were enrolled into the study. They were assured that all the information was confidential and they are free to withdraw from the study if they wished so.
DASS Questionnaire
The DASS is a 42-item questionnaire which includes three self-report scales designed to measure the negative emotional states of depression, anxiety and stress. Each of the three scales contains 14 items, divided into subscales of 2-5 items with similar content. (www.psy.unsw.edu.au/groups, Australian Centre for Post traumatic mental health) [17]. The questionnaire contained a statement for which the patient was required to state (0) Did not apply to me at all; (1) Applied to me to some degree, or some of the time; (2) Applied to me to a considerable degree, or a good part of time (3) Applied to me very much, or most of the time. Then the scores were tabulated as per whichever category it belonged to, (which only the investigator knew) namely, (1) Depression Score (D Score), (2) Anxiety score (A Score); Stress score (S Score), were computed and tabulated into following grades.
Depression Anxiety Stress
Normal (N) 0 – 9 0 - 7 0 – 14
Mild (Mi) 10 – 13 8 – 9 15 – 18
Moderate (Mo) 14 – 20 10 – 14 19 – 25
Severe (Se) 21 – 27 15 – 19 26 – 33
Extremely Severe (ES) 28+ 20+ 34 +
Questionnaire administration: All the study related work was carried out between 11 AM to 12 noon, so that the patients will be in as much relaxed state after the morning routines. The study was carried out by an undergraduate medical student who was well versed with the local language and able to freely communicate with the patients. The patients’ responses were marked by the investigator, to reduce discomfort to the patient.
Inclusion criteria
ICU for more than 3 days
Able to understand and respond to questionnaire
Aged above 18 years
Exclusion criteria
Shorter than 3 days in ICU
Patients on ventilator
Patients unable to respond to questionnaire
Results
The results obtained were statistically analysed using SPSS 17.0, Unpaired ‘t’ test to compare the scores among the groups, Pearson Chi-Square used for qualitative data, p<0.05 was considered significant.
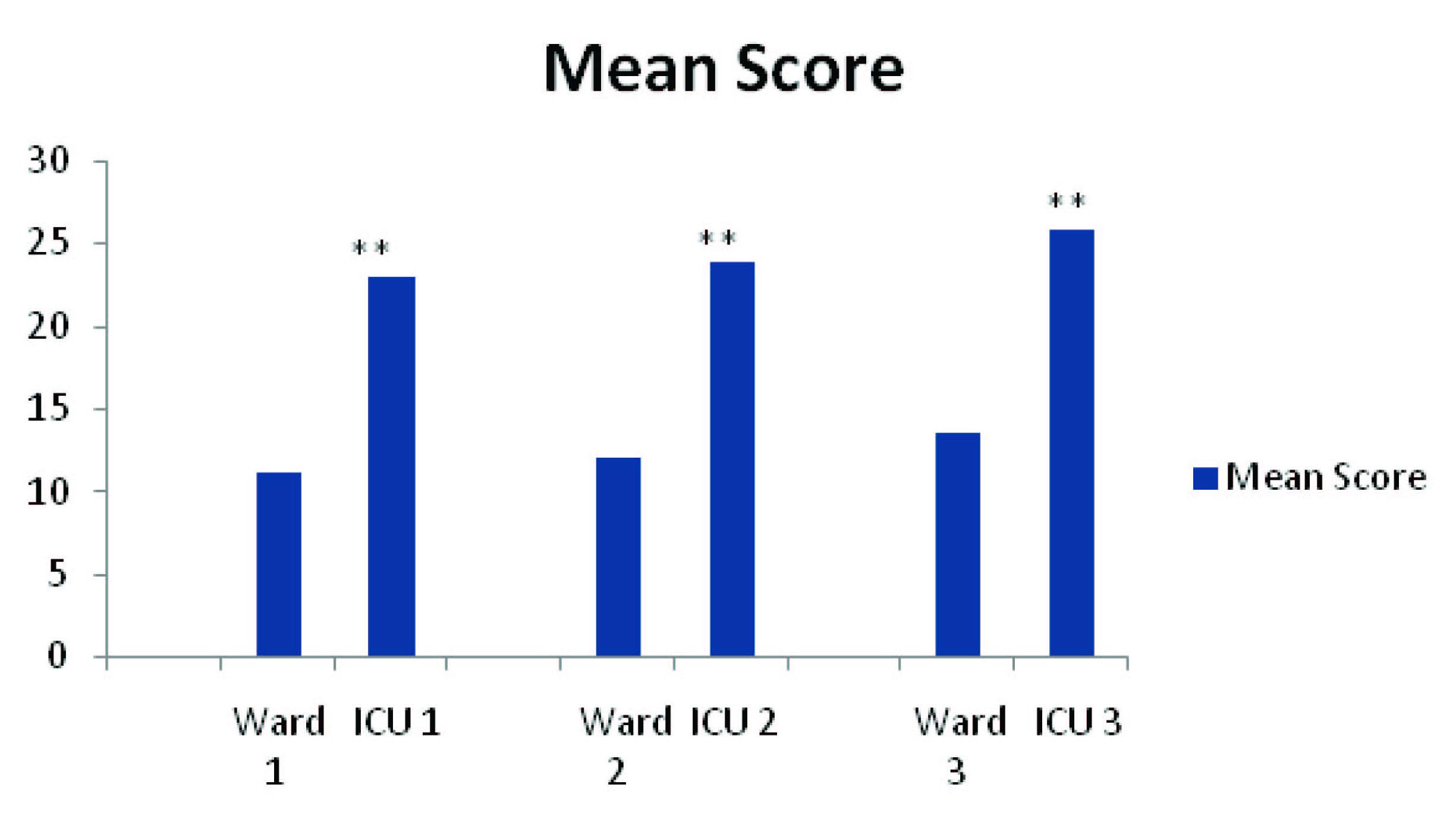
The mean of depression score, anxiety score and stress scores were found to be significantly higher among the ICU patients compared to the ward patients.
Depression grades among the ICU patients were compared to those in ward. We found 32.5% had scores of Extremely severe (ES) among ICU patients, while it was nil in ward. Moderate stress (Mo - 20%) and Mild stress (Mi 50%) was significantly higher among the ward patients.
Anxiety grade showed Extremely severe (Es 60%) and Severe levels (Se 25%) in ICU patients and corresponding figures were 10% and 30 % respectively in ward patients. While moderate, mild and normal figures were comparable in ward admitted patients, ICU patients revealed a high degree of severity of anxiety.
Analysis of stress grades revealed that 50% of the patients in ICU were severely stressed, but the Extremely high (Es) grades were shown only by 10%. In contrast to this the stress levels among ward admitted patients, only 15% of them showed mild stress where as 70% of them were normal. We also analysed the grades among the patients in two age groups, viz. Above 40y (n=17) and below 40y (n=23). We found 43%, 78% and 17% of Extremely sever (Es) depression, anxiety and stress score levels for the group above 40 y, compared to 17%, 35% and 0% respectively for the below 40 y group. But below 40 y age group showed severe (Se) range of scores for parameters.
On analysis of data from male (22) and female (18) patients, Females showed ES Depression (38%), Anxiety score (78%) and Stress score (11%), which were higher than males who showed ES levels among 27% (D score), 45% (A Score) and 9% (S-score). Among Male patients, the distribution of levels of severity was almost equal levels as far as D – score and A scores were concerned (D-Score = ES = 27%; Se = 32%; Mi = 27%; MI = 9%; N = 5%; A score = ES n=45%; Se = 32%; Mo=23%, Mi=Nil; N=NIL); this type of distribution was not observed in females.
Discussion
Psychological impact of the stay in ICU appears to affect the patients in a deleterious way [18]. From the results obtained in the present study in Indian hospital set up, we found significantly elevated levels of depression reporting using the DASS response. It was also true for the anxiety and stress scores. Even though the patients ward admitted to ward, (group 1) showed increased levels of depression,anxiety and stress scores, which were well above normal mean scores [Table/Fig-1] these scores among the ICU patients were significantly higher (p<001). Higher stress levels found in these patients was in accordance with the previous findings reported elsewhere [19]. We found highly significant increase in all parameters in ICU patients. Further, we compared the self reported results with those admitted in the ward, predictably, these patients reported lesser levels of depression, stress and anxiety in ward patients.
Overall Comparison of scores among ICU and ward patients showing mean scores for the whole group. Mean Group scores: Students t-test.**p<0.001.1=D Score (depression score); 2=A Score (Anxiety score); 3=S Score (Stress score)
Depression scores and anxiety scores were extremely severe (ES) in about 32% and 60% of patients respectively among ICU patients [Table/Fig-2], but in those in the wards 50% showed mild depression (Mi) reporting, which is much lower levels. This evidence suggested that the ICU situation increases the depression, anxiety and stress levels, and predictably in the wards, the stress levels will be lower. The reasons for this may be several, which may include the severity of illness, end of life feeling in ICU, proximity to the family members in the wards not with standing the financial worries. Economic conditions of patients and family too have an influence on these parameters. We have also found from the patient’s data that 95% of the patients we included in this study did not have medical insurance unlike more than 75% of the patients covered in the developed countries, particularly in the US [20,21]. This study gives an insight into the psychological status of patients admitted to hospital.
Comparison of number of subjects reporting depression score, anxiety score & stress score of Patients in ICU & ward.
| | Depression score | Anxiety score | Stress score |
|---|
| Ward | ICU | Total | Ward | ICU | Total | Ward | ICU | Total |
|---|
| ES | Count | 0 | 13** | 13 | 4 | 24** | 28 | 0 | 4 | 4 |
| % | 0% | 32.5% | 16.3% | 10.0% | 60.0% | 35.0% | .0% | 10.0% | 5.0% |
| Se | Count | 2 | 10** | 12 | 12 | 11 | 23 | 4 | 21** | 25 |
| % | 5% | 7.5% | 15.1% | 30% | 25% | 27.5% | 10.0% | 52.5% | 31.3% |
| Mo | Count | 8 | 10 | 18 | 10** | 5 | 15 | 2 | 9 | 11 |
| % | 20% | 25% | 22.5% | 25.0% | 12.5% | 18.8% | 5.0% | 22.5% | 13.8% |
| Mi | Count | 20** | 5 | 25 | 6** | 0 | 6 | 6** | 1 | 7 |
| % | 50.0% | 12.5% | 31.3% | 15.0% | .0% | 7.5% | 15.0% | 2.5% | 8.8% |
| N | Count | 10** | 2 | 12 | 8** | 0 | 8 | 28** | 5 | 33 |
| % | 25.0% | 5.0% | 15.0% | 20.0% | .0% | 10.0% | 70.0% | 12.5% | 41.3% |
Pearson Chi square test (df=5; ** p<0.001); ES = extremely severe; Se = Severe; Mo = Moderate; Mi = mild; N = normal
Conclusion
This study throws light on the status of patients in hospital environment in Indian conditions, which revealed elevated depression, anxiety and stress. It is necessary to give attention to measures to attenuate this from cascading and causing detrimental effects on the patients. Suitable psychiatric help, counseling and better communication with the patients regarding their disease status and recovery could be more helpful. However our study involved only a small number of patients and those admitted to one centre only. More number of patients and in multiple centres may throw better light on the problem encountered in the Intensive care units.
Pearson Chi square test (df=5; ** p<0.001); ES = extremely severe; Se = Severe; Mo = Moderate; Mi = mild; N = normal
[1]. Jones C, Skirrow P, Griffiths RD, Humphris GH, Ingleby S, Eddleston J, Rehabilitation after critical illness: a randomized, controlled trialCrit Care Med 2003 31(10):2456-61. [Google Scholar]
[2]. Sukantarat KT, Brett SJ, The neuropsychological consequences of intensive care. In: Angus DC, Carlet J, edsSurviving Intensive Care (Update in Intensive Care and Emergency Medicine) 2002 BerlinSpringer-Verlag:51-61. [Google Scholar]
[3]. Koshy G, Wilkinson A, Harmsworth A, Waldmann C, Intensive care unit followup program at a district general hospitalIntensive Care Medicine 1997 23(S1):S160 [Google Scholar]
[4]. Svenningsen H, Associations between sedation, delirium and post-traumatic stress disorder and their impact on quality of life and memories following discharge from an intensive care unitDan Med J 2013 60(4):4630 [Google Scholar]
[5]. Roberts B, Rickard CM, Rajbhandari D, Turner G, Clarke J, Hill D, Multicentre study of delirium in ICU patients using a simple screening toolAust Crit Care 2005 18(1):6:8-9.:11-14. [Google Scholar]
[6]. Ceriana P, Fanfulla F, Mazzacane F, Santoro C, Nava S, Delirium in patients admitted to a step-down unit: analysis of incidence and risk factorsJ Crit Care 2010 25(1):136-43. [Google Scholar]
[7]. Brummel NE, Jackson JC, Pandharipande PP, Thompson JL, Shintani AK, Dittus RS, Delirium in the ICU and subsequent long-term disability among survivors of mechanical ventilationCrit Care Med 2014 42(2):369-77. [Google Scholar]
[8]. Jezierska N, Psychological reactions in family members of patients hospitalised in intensive care unitsAnaesthesiol Intensive Ther 2014 46(1):42-45. [Google Scholar]
[9]. Day Alex, Haj-Bakri Samer, Lubchansky Stephanie, Mehta Sangeeta, Sleep, anxiety and fatigue in familymembers of patients admitted to the intensive care unit:a questionnaire studyCritical Care 2013 17:R91 [Google Scholar]
[10]. Pillai LV, Ambike D, Husainy S, Vaidya N, Kulkarni SD, Aigolikar S, The prevalence of post-traumatic stress disorder symptoms in relatives of severe trauma patients admitted to the intensive care unitIndian J Crit Care Med 2006 10:181-86. [Google Scholar]
[11]. Little A, Ethier C, Ayas N, Thanachayanont T, Jiang D, Mehta S, A patient survey of sleep quality in the intensive care unitMinerva Anestesiol 2012 78:406-14. [Google Scholar]
[12]. Parthasarathy S, Tobin MJ, Sleep in the intensive care unitIntensive Care Med 2004 30:197-206. [Google Scholar]
[13]. Drouot X, Cabello B, d’Ortho MP, Brochard L, Sleep in the intensive care unitSleep Med Rev 2008 12:391-403. [Google Scholar]
[14]. Pochard F, Darmon M, Fassier T, Bollaert PE, Cheval C, Coloigner M, Symptoms of anxiety and depression in family members of intensive care unit patients before discharge or death. A prospective multicentric studyJ Crit Care 2005 20:90-96. [Google Scholar]
[15]. Azoulay E, Pochard F, Kentish-Barnes N, Chevret S, Aboab J, Adrie C, Risk of post-traumatic stress symptoms in family members of intensive care unit patientsAm J RespirCrit Care Med 2005 171:987-94. [Google Scholar]
[16]. Guntupalli KK, Rebbapragada VR, Lodhi MH, Bradford S, Burruss J, McCabe D, Anxiety, depression and post-traumatic stress reactions in relatives of intensive care unit patientsChest 2007 132(4 Suppl):549-50. [Google Scholar]
[17]. Lovibond SH, Lovibond PF, Manual for the Depression Anxiety Stress Scales 1995 2nd. EdSydneyPsychology FoundationISBN 7334-1423-0 [Google Scholar]
[18]. Sukantarat KT, Williamson RC, Brett SJ, Psychological assessment of ICU survivors: a comparison between the Hospital Anxiety and Depression scale and the Depression, Anxiety and Stress scaleAnaesthesia 2007 62(3):239-43. [Google Scholar]
[19]. Tramm R, Hodgson C, Ilic D, Sheldrake J, Pellegrino V, Identification and prevalence of PTSD risk factors in ECMO patients: A single centre studyAust Crit Care 2014 May 17 :piiS1036-7314(14)00034-4 [Google Scholar]
[20]. Kulkarni Hrishikesh S, Kulkarni Karishma R, Mallampalli Antara, Parkar Shubhangi R, Karnad Dilip R, Guntupalli Kalpalatha K, Comparison of anxiety, depression, and post-traumatic stress symptoms in relatives of ICU patients in an American and an Indian public hospitalIndian J Crit Care Med 2011 15(3):147-56. [Google Scholar]
[21]. Danis M, Linde-Zwirble WT, Astor A, Lidicker JR, Angus DC, How does lack of insurance affect use of intensive care? A population-based studyCrit Care Med 2006 34:2043-48. [Google Scholar]