Concurrent infection with two agents can result in an illness having overlapping symptoms creating a diagnostic dilemma for the treating physician. Acute febrile illness (AFI) is a common clinical syndrome among patients seeking hospital care in India. Dengue is one such disease which usually presents with symptoms of flu-like illness with high-grade fever, generalized body ache, nausea, and vomiting as well as maculopapular rashes. The symptoms of dengue may mimic other diseases such as leptospirosis, influenza A, Salmonella Typhi, Japanese encephalitis, chikungunya and malaria which are also prevalent in areas where dengue is endemic [1,2]. The similarity in symptoms and differential diagnoses of these diseases often mimick those of dengue and thereby makes accurate clinical diagnosis and treatment difficult without laboratory confirmation [3]. In India, potential dengue fever is generally ascribed to all febrile illnesses during the monsoon period (September to November) unless confirmed through laboratory testing. It is a common practice for patients with fever to visit a health-care facility only if fever persists after two to three days of non- specific self-medication. Dengue and typhoid fever, if not approached timely, may lead to life threatening consequences [1,3–5].
Emerging and re-emerging diseases are a concern in Asia during a dynamic time of population growth, urbanization, and global migration. This, in turn, enhances the need for continued international surveillance and improvement of public health infrastructures to meet existing and future emerging disease threats. Dengue co- infection with malaria and other arboviral illnesses has been studied in many parts of the world. Epidemiology, disease course and complications have been studied and reported for both the diseases separately, both in India and abroad. However, there is scarcity of data regarding dengue and typhoid co- infection in both, the developed and the developing world. This study attempts to find the current co- infection rates in North Delhi.
Materials and Methods
A retrospective analysis was done between August and November 2013 of a total of 659 patients. Kasturba Hospital is a 500 bedded government hospital situated in North Delhi. Individual patient hospital records showed that the common clinical manifestations in these cases at the time of sample collection were fever, headache, nausea, vomiting, malaise and arthralgia. Abdominal discomfort, chest pain, dizziness and diarrhoea were less common. Demographic data including age and sex of the patients, the date of onset of symptoms were obtained through medical records from the medical records department. Dengue specific IgM antibodies are detected by Dengue IgM antibody capture ELISA test issued by National Institute of Virology (NIV), Pune in this hospital. Serodiagnosis of Salmonella Typhi infection is conducted by the Widal test, which detects agglutinating antibodies against the O and H antigens of S. Typhi and “H” antigens of S. Paratyphi A and S. Paratyphi B [6]. Titers of antibodies against the antigens are deemed significant where single acute phase samples resulted in O > 1: 160 and H > 1 : 160.
Results
Of the 659 febrile sera samples tested here, 141 (21.39%) tested positive for dengue. Of these 91 were females and 50 males. Of the dengue cases, eleven were co- infected with typhoid fever (11/141= 7.8%). Maximum no. of dengue positive cases was seen in age group 0- 10 y. [Table/Fig-1]. Case Fatality Rate (CFR) was zero. Suspected complications like gall bladder edema and fatty liver was seen in one patient each. Other co- infections with dengue are mentioned in [Table/Fig-2]. Age groups of patients co-infected with dengue and typhoid were as follows; 0-10 y: 5, 11-20 y: 3, 21-30 y: 2, >60 y: 1.
Age-wise distribution of dengue cases and co-infected cases
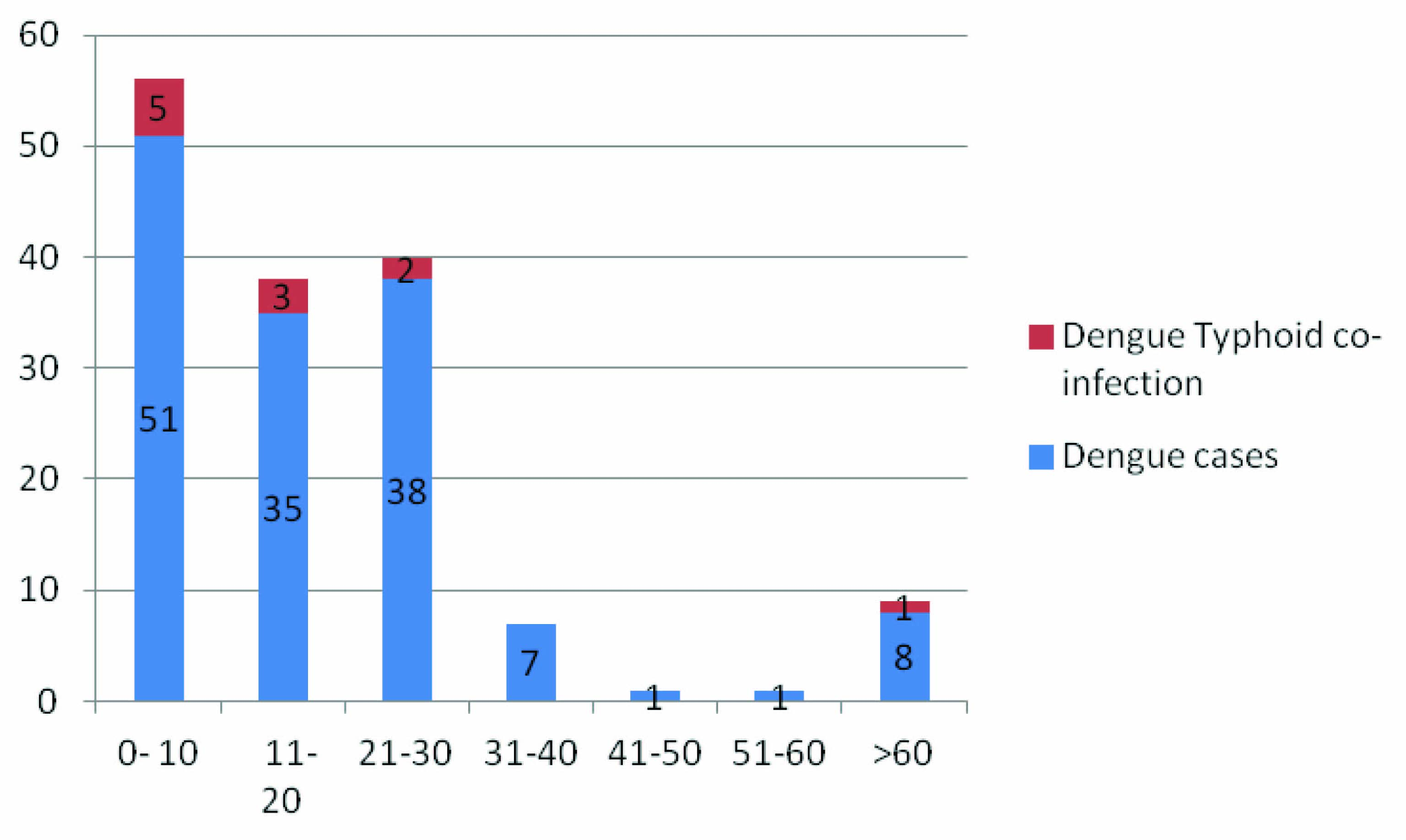
Age-wise distribution of dengue cases and co-infected cases
| Reference | Co- infection dengue + typhoid | Total no. of isolates | Percentage co-infection | Other co-infections seen in study |
|---|
| Kasper et al., [7] | 3 | 883 | 0.30% | Leptospira, influenza, other bacteria |
| Baba et al., [8] | 13 | 310 | 4.1 | Malaria |
| Parwati (case series) | 5 | 5 | - | None |
| South India | 6 | 858 | 0.60% | Leptospira, malaria |
| Ahmed et al., (case series) [9] | 1 | 1 | - | Hepatitis A,E |
| Sadjana et al., [10] (case series) | 1 | 1 | - | None |
| Present study | 11 | 141 | 7.8 | PID*, URTI** |
* Pelvic Inflammatory Disease, ** Upper Respiratory Tract Infection
Discussion
The top three causes of acute fever in Delhi during the rainy season (July- October) are dengue fever, Salmonella spp. and other viral illnesses (hepatitis A, influenza A, chikungunya etc).
Arboviral diseases are important emerging infectious diseases in India. The changing Indian scenario in terms of mass migration to urban states, deforestation, global climate changes etc has possibly made a marked difference in terms of infectious diseases.
Children frequently have concurrent infection with other viruses and bacteria causing upper respiratory symptoms [11]. Earlier there have been reports of concurrent infection of dengue virus with a flavivirus, Chikungunya and with different bacteria including Salmonella Typhi [12]. A study from South India reported co-infection with enteric fever in 6 cases (6/858: 0.7%) apart from co-infection with leptospirosis, malaria and bacterial meningitis [4]. This is much less compared to the present study (7.8%) [Table/Fig-2]. shows dengue and typhoid co- infection reported both from India and abroad.
Enteric fever/Typhoid fever is usually caused by S. typhi and less by S. paratyphi and S. choleraesuis. The onset of symptoms is insidious with an incubation of 10-14d. The fever is unremittent; there are spikes in temperature without any return to normal (saddle back fever) [13]. In contrast, dengue fever manifests as spectrum of illness ranging from inapparent or mild febrile illness to severe and fatal hemorrhagic disease. In a typical case of dengue fever, the patient experiences high fever lasting for 5 to 7d. Concomitantly, a severe frontal and retro orbital headache, myalgias, especially lower back, arm, and leg pains, malaise, arthralgia and anorexia may accompany [14]. In typhoid fever, a dull, continuous frontal headache begins during the first two days of fever; mild arthralgia involving multiple joints and vague, poorly localized back pain may occur [13]. Constipation is more common than diarrhea; it occurs in about 50%, while diarrhea occurs in about 30% of typhoid patients [13]. In dengue fever, constipation is occasionally reported; diarrhea and respiratory symptoms are frequently reported and may be due to concurrent infections [11]. A well known but not unique feature of typhoid is prominent temperature and/or pulse dissociation but it may also occur in dengue fever [11,14].
In a previous hospital-based surveillance study at Kenya, it was observed that Widal test method showed 7% false negative and 18.7% false positive typhoid cases [1]. In other studies performed in endemic regions of India, the overall sensitivity of the Widal test was 64.49% for the O antibody and 78.26% for the H antibody and is a commonly used test in resource poor settings [15]. In the present study if both O and H antibody titres were high (>1:160) irrespective of culture results, a presumptive diagnosis of typhoid was made, and the diagnosis was supported by clinical manifestations of the patient. Antibiotic usage prior to drawing sample for blood culture could not be ascertained therefore, blood culture results were not considered.
None of the patients in the present study experienced hemorrhagic manifestation. Fatty liver and gall bladder edema was seen in two cases, which could have been related to either typhoid fever [11,13] or dengue infection [16,17]. Case fatality rate (CFR) for all hospitalized children with dengue fever may be as low as 0.2-5 % with higher rates up to 12.6% in patients with Dengue Shock Syndrome [4]. In another study it was reported as 1.05% [4]. CFR in the present study was 0. This can be attributed to the fact that there is growing awareness among people regarding ill effects of dengue if not treated timely. This led to early diagnosis and thereby early treatment. All patients who showed significant titers for Widal test were clinically correlated and with immediate effect started on antibiotics. Maximum duration of hospital stay was nine days seen in one patient.
A study from Tanzania supported the long-held hypothesis that malaria in children in that region, preceeds and predisposes invasive Non Typhoidal Salmonella (NTS) infection [18,19]. Although the mechanism underlying the association between malaria and NTS is incompletely understood, the possibility of metabolic, haemodynamic or inflammatory processes occurring during severe malaria predisposing to invasive bacterial disease has not be ruled out [18]. Dengue-typhoid co-infection rate of 7.8% is a high value in itself. Similarly questions like whether or not dengue fever predisposes to typhoid fever, or do they separately infect a person, need to be answered. There is a dearth of literature regarding dengue-typhoid co- infection, the possible effect that one disease can have on progression/ regression of the other, the gravity of complications if both co- exist or whether one disease precedes the other. Both dengue and typhoid occur seasonally in India especially during the monsoons where on one hand mosquito breeding and on other hand faeco- oral transmission occurs actively. Co-infection may open an entirely new dimension of complications thus spelling an impending doom for the people as well as the concerned civic authorities and health policies. Further studies regarding this issue need to be done. In the present study, the dengue infection could have occurred concurrently while the patients were also suffering from enteric fever, or even 2-3 months before they developed the symptoms. Early recognition along with meticulous monitoring and targeted supportive care is the cornerstone of a successful outcome both in dengue and enteric fever.
Maximum dengue patients were from age group 0- 10y due to the fact that this hospital is frequented by patients who are mostly women and children. This finding may be of help to the epidemiologists, pediatricians and dengue prevention and control measure authorities for early diagnosis and to plan out and implement various measures. This study emphasizes the importance of early diagnosis and prevention of complications using accurate tests and prompt treatment.
The limitations of the present study relate to the inherent weakness of a retrospective analysis. Secondly, Widal test has its own limitations in detecting typhoid. Thirdly, serotyping of dengue isolates was beyond the scope of the study but would have added interesting information.
Conclusion
The present study reports the incidence of dengue and co- infection which are important when planning large scale vaccine trials as well as making health policies. If not treated early, dengue and typhoid together, may lead to multi-organ involvement and further undesired consequences. Dengue-typhoid co-infection is a preventable cause of death. Although further studies are required, to the best of our knowledge, this is the first study from North- India, to report the co- infection of dengue and typhoid fever.
* Pelvic Inflammatory Disease, ** Upper Respiratory Tract Infection