To compare ECG changes in patients of acute mania being treated with lithium carbonate or verapamil.
Materials and Methods
Randomized double blind parallel group controlled study of 4 wk duration done at the Rajindra medical college and hospital, Patiala Punjab, India after ethical clearance from institutional Ethic committee. Fifty patients of bipolar affective disorders admitted in the ward of psychiatry department, Rajindra Hospital, Patiala, were taken. A written informed consent was taken prior to the enrollment. The detailed history of all the patients fulfilling the inclusion and exclusion criteria was recorded on the performa.
Inclusion Criteria
Patients fulfilling ICD 10 criteria for manic episode.
Adult males and non-pregnant females not planning conception.
Patients with a score of >10 on bech-Raefelson Mania Rating scale(BRMRS).
Exclusion Criteria
Patients with history of epilepsy, mental retardation, substance abuse, or having taken any treatment of ECT for current episode during previous month.
Patients with any other medical illness contraindicating the use of trial medication.
Pregnant females, lactating mothers, and females planning conception.
Refusal to give informed consent.
Design: Randomized double blind parallel group controlled study of 4 weeks duration done at the Rajindra medical college and hospital, Patiala Punjab.
Twelve lead electrocardiogram in lying down position with emphasis on heart rate, rhythm, P-wave, P-R interval, QRS axis, QRS complex, QT interval, ST segment, T wave, U wave was recorded at the base line level, 7 d and 28 d after start of treatment.
Dose of drug
Verapamil: 80mg two times a day on Ist day
80mg three times a day on 2nd day
80mg four times a day thereafter.
Lithium carbonate: 300mg three times a day for five days
Then adjusted thereafter according to plasma level between 0.6-1.2 meq/L.
Fifty patients were randomly allocated to one of the two groups. Group A(n-25) were put on Lithium carbonate 300 mg three times a day for five days and then adjusted dose to maintain plasma level between 0.6-1.2 meq/L. In Group B (25) patients were given tablet verapamil 80mg two times a day on Ist day, 80mg three times a day for the next two days and then 80mg four times a day thereafter. After giving first dose of verapamil, patients were observed for any cardiovascular side effects and subsequent doses were given only if the patient was able to tolerate the verapamil. In both groups rescue haloperidol treatment was given by i.m or oral route in case of any worsening of symptoms [8].
The study parameters were recorded at the baseline, after 7 d and 28 d of trial medication.
The patients were observed for any cardiovascular side effect. Serum lithium was estimated by flame photometric method [9].
Statistical Analysis
The data was put in tables as mean ± standard error. Nominal and ordinal data was analysed by non parametric tests, and true interval data was analyzed by parametric tests. Chi-square-test was used for ordinal data in two groups. Unpaired t test was used for comparing baseline data in two groups and paired t-test was used for the interval data. A level of less than 5% value of p was considered statistically significant.
Results and Observations
The two population groups were similar in all characteristics like age, sex, marital status, literacy and socioeconomic status. There was no significant difference in age and sex and other parameters distribution of patients between two groups as shown in [Table/Fig-1].
Age and sex distribution of patients in Group A & B
| Patient characteristic | Group A (n-25) | Group B (n-25) | Significance |
|---|
| Age(years) | Median 30 Range 18-50 | Median 30 Range 19-50 | p>0.05 NS |
| Sex | Males 18 Females- 7 | Males 20 Females- 5 | p>0.05 NS |
| Marital status | Married 19 Unmarried 6 | Married 17 Unmarried 8 | p>0.05 NS |
| Rural/ urban | Rural 10 Urban 15 | Rural 11 Urban 14 | p>0.05 N |
| literacy | Illiterate 13 Literate 12 | Illiterate 15 Literate 10 | p>0.05 N |
There was no significant difference in the heart rate of patients bet-ween two groups at the baseline (p>0.05) as shown in [Table/Fig-2].
Baseline heart rate in Group A and B
| Heart rate | Group A(n-25) | Group B(n-25) |
|---|
| Range | 71-93 | 60-107 |
| Mean ± S.E. | 78.8 ± 3.15 | 82.8 ±3.2 |
In group A the heart rate on the seventh day was not significantly different from baseline (p>0.05), but on the 28th day the HR was significant less than the baseline (p< 0.05). There was a decrease of 7.2% on the 7th day and 10.4% on the 28th day of the trial the decrease was statistically significant on the 28th day as shown in [Table/Fig-3].
Heart rate in Group A during the trial
| Heart rate | Day 1 | Day 7 | Day 28 |
|---|
| Mean ± S.E. | 78.8 ± 3.15 | 73.1 ± 2.5 | 70.6 ± 2.7 |
| Range | 71-93 | 60-88 | 60-88 |
In group B the heart rate on the seventh day was not significantly different from baseline (p>0.05), but on the 28th day the HR was significant less than the baseline (p< 0.01). There was a decrease of 7.97% on the 7th day and 19.6% on the 28th day of the trial the decrease was statistically significant on the 28th day as shown in [Table/Fig-4].
Heart rate in Group B during the trial
| Heart rate | Day 1 | Day 7 | Day 28 |
|---|
| Mean ± S.E. | 82.8 ± 3.2 | 76.2 ± 2.9 | 66.6 ± 2.1 |
| Range | 60-107 | 48-100 | 42-83 |
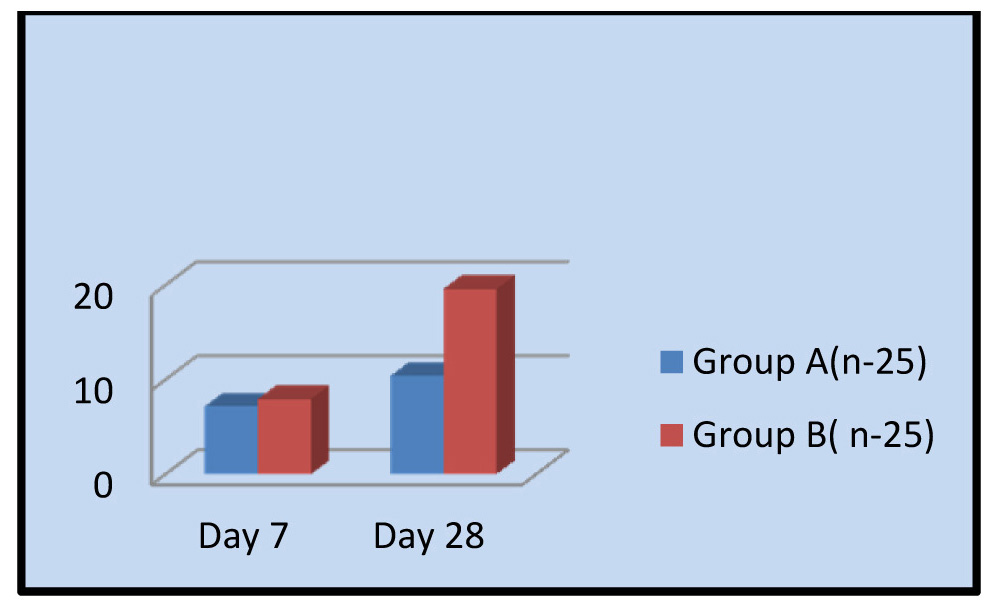
The mean percentage decrease in heart rate on day 7 was 7.2±0.80 for the Group A where it was 7.97±0.78 in Group B. on 28th day there was a decrease of 10.4%± 0.84 for group A and 19.6% ±0.46 in group B. there was a greater decrease in Group B in the heart rate on 28th day (p< 0.05) as shown in [Table/Fig-5].
Percentage decrease in heart rate during the trial
There was no significance difference (p>0.05) between two groups in the PR interval at the base line as shown in [Table/Fig-6].
PR interval at baseline in Group A and B
| PR interval in seconds | Group A(n-25) | Group B(n-25) |
|---|
| Range | 0.12-0.20 | 0.12-0.20 |
| Mean ± S.E. | 0.154 ± 0.0078 | 0.165 ±0.20 |
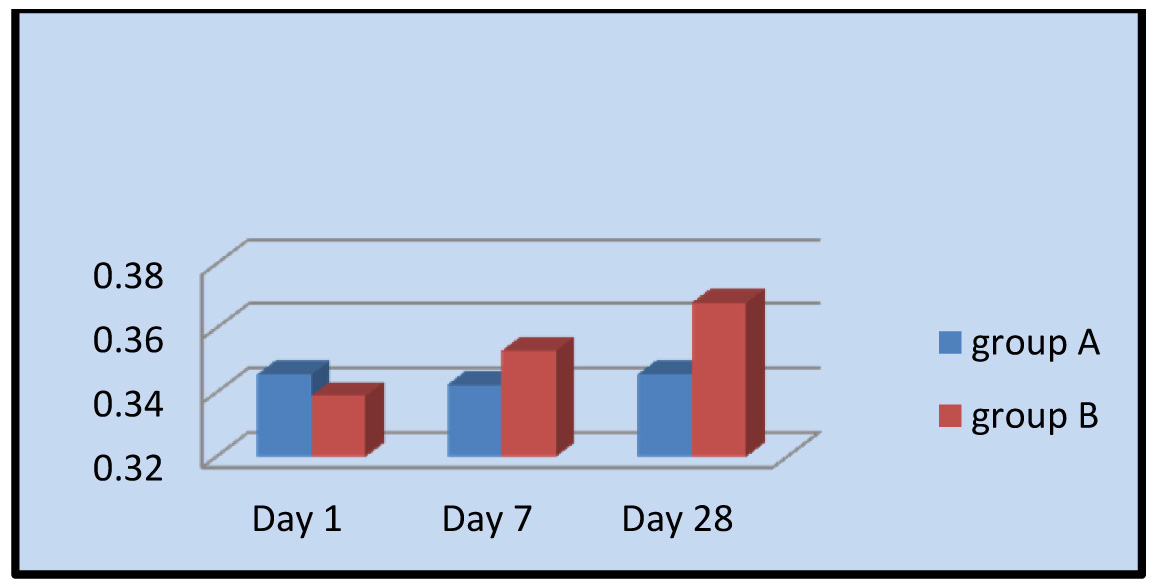
In group A the PR interval on the 7th and 28th day was not significantly different from baseline. As compared to baseline thee was increase of 5.97% on the 7th day and 1.30% on the 28th day of the trial. But this was not significant (p>0.05) as shown in [Table/Fig-7].
PR interval in Group A during the trial
| PR interval | Day 1 | Day 7 | Day 28 |
|---|
| Mean ± S.E. | 0.154 ± 0.0078 | 0.1632 ± 0.0065 | 0.154 ± 0.0078 |
| Range | 0.06-0.20 | 0.12-0.20 | 0.12-0.20 |
| Percentage increase | | 5.97 | 1.30 |
In group B the PR interval on the 7th and 28th day was not significantly different from baseline. As compared to baseline thee was increase of 1.8% on the 7th day and 5.7 on the 28th day of the trial. But this was not significant (p>0.05) as shown in [Table/Fig-8].
PR interval in group B during the trial
| PR interval | Day 1 | Day 7 | Day 28 |
|---|
| Mean ± S.E. | 0.165 ± 0.0123 | 0.168 ± 0.0065 | 0.1744 ± 0.0056 |
| Range | 0.08-0.20 | 0.08-0.20 | 0.12-0.20 |
| Percentage increase | | 1.8 | 5.7 |
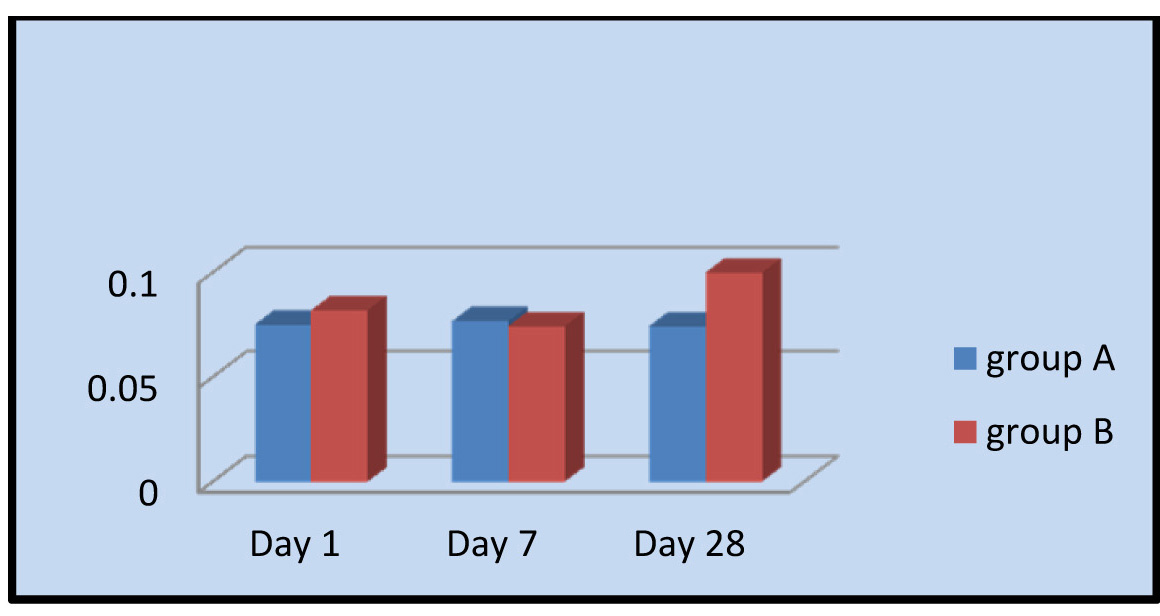
While compairing the QTc for both groups at the baseline, it was found that there was no significance difference (p>0.05) between two groups as shown in [Table/Fig-9]. The QTc on the 7th and 28th day was not significantly different from baseline as shown in [Table/Fig-10] for both the groups.
QTc at baseline in group A and B
| QTc | Group A (n-25) | Group B (n-25) |
|---|
| Range | 0.28-0.40 | 0.28-0.40 |
| Mean ± S.E. | 0.346 ± 0.00796 | 0.339 ±0.10098 |
QTc interval in Group A and B during the trial
There was no significance difference (p>0.05) between two groups in the QRS duration at the base line as shown in [Table/Fig-11]. The QRS duration on the 7th and 28th day was not significantly different (p>0.05) from the base line in both the groups as shown in [Table/Fig-12].
QRS duration at baseline in group A and B
| QRS duration | Group A(n-25) | Group B(n-25) |
|---|
| Range | 0.04-0.08 | 0.04-0.08 |
| Mean ± S.E. | 0.752 ± 0.0105 | 0.082 ±0.0154 |
QRS duration in group A and B during the trial
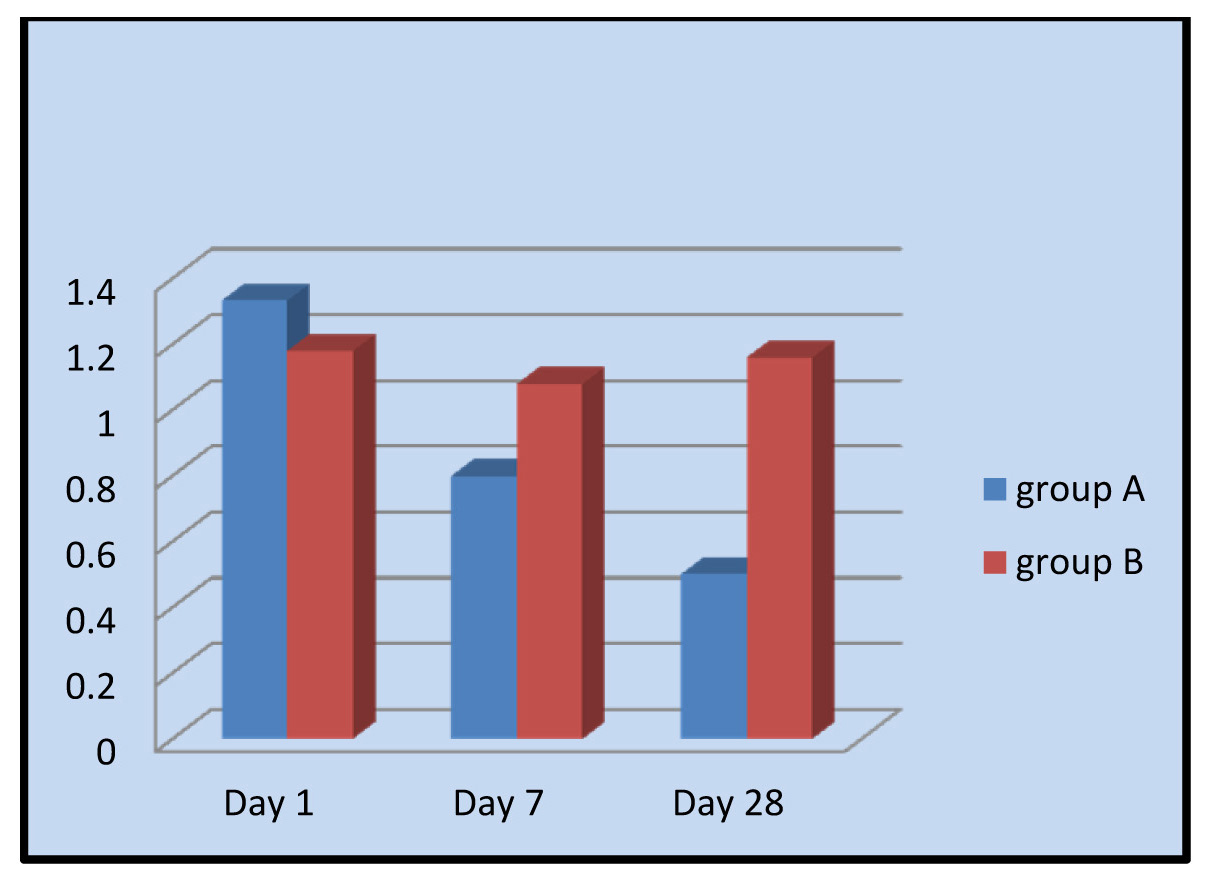
There was no significance difference (p>0.05) between two groups in the T wave amplitude at the base line as shown in [Table/Fig-13]. In group A the T wave amplitude on the 7th and 28th day was significantly less than (p<0.05) the base line i.e. the 1st day of trial as shown in [Table/Fig-14].
T wave amplitude at baseline in group A and B
| T wave amplitude | Group A(n-25) | Group B(n-25) |
|---|
| Range | 0.5-2 | 0.5-3.5 |
| Mean ± S.E. | 1.333 ± 0.60193 | 1.98 ±0.714 |
T wave amplitude in group A during the trial
| T wave amplitude(mm) | Day 1 | Day 7 | Day 28 |
|---|
| Mean ± S.E. | 1.333 ± 0.60193 | 0.8 ± 0.60193 | 0.501 ± 0.7379 |
| Range | 0.5-2 | 0 -1.5 | 1-1.0 |
In group B the T wave amplitude on the 7th and 28th day was not significantly different (p>0.05) from the base line as shown in [Table/Fig-15]. There was no significance difference (p>0.05) between two groups in the P wave amplitude at the base line. The P wave amplitude on the 7th and 28th day was not significantly different (p>0.05) from the base line in both the groups as shown in [Table/Fig-16].
T wave amplitude in group B during the trial
| T wave amplitude(mm) | Day 1 | Day 7 | Day 28 |
|---|
| Mean ± S.E. | 1.98 ± 0.714 | 1.78 ± 0.867 | 2.20 ± 0.736 |
| Range | 0.5-3.5 | 0.5 -1.5 | 1-5 |
P wave amplitude in group A and B during the trial
Discussion
Verapamil well-tolerated drug when used for its primary cardio-vascular indications has been reported in small case series and a few small controlled trials to be helpful in patients with bipolar disorder. Recently few studies classified verapamil as sometimes useful as an alternative choice for treatment-resistant mania, to be considered for patients who cannot tolerate other mood stabilizers, or as an add-on to other medications [10].
Verapamil, although primarily known as a calcium channel blocker, also has PKC inhibitory activity, produces clinical improvement in acutely manic patients. Mallinger et al., concluded that augmentation of lithium treatment with verapamil can improve therapeutic outcome in manic patients who do not respond to an initial trial of lithium [11]. Combined treatment with verapamil and lithium has been associated with a variety of adverse events, including exacerbation of lithium side effects, choreoathetosis, bradycardia with possible myocardial infarction, and neurotoxicity with ataxia. Thus, caution and appropriate monitoring are essential when using this drug combination [11].
The present study was conducted to compare the electrocardiographic changes in patients of acute mania being treated with lithium carbonate or with verapamil.
The median age in both groups was 30 y with a range of 18-50 y in group A and 19-50 y in Group B as shown from [Table/Fig-1] the median age is in agreement with Giannini et al., [6], and Garza Trevino et al., [12]. In both groups male-female ratio, marital status, rural urban distribution, literacy status, occupation and ethnic distribution was comparable (p>0.05). Thus the two groups were homogenous in patient characteristics (as shown from [Table/Fig-1]).
[Table/Fig-3] shows comparison of heart rate (beats/min.) at baseline in two groups. The mean ± SE heart rate in Group A was 78.8+3.15 with range 71-93, where as in group B it was 82.8±3.2 with a range 60-107. There was no significant between two groups at the baseline. Thus two groups were comparable.
[Table/Fig-4] show that in group B patients there was a trend showing decrease in heart rate on 7th day by 7.97% but was not significant whereas on the 28th day of trial there was a significant decrease (p<0.05), of 19.6% as compared to baseline. It is clear from the [Table/Fig-5] that there was a significant decrease in heart rate in both the groups. In Group A it was 10.4% whereas in Group B it was19.6% these findings are explained by the fact that both lithium and verapamil decrease the rate of spontaneous depolarisation of the sinous node and slow the conduction through the arterioventricular node.(dubovsky SL and Franks RD 1983). However, there was a greater decrease in heart rate with verapamil [8,13].
[Table/Fig-6,9,11] shows the comparison of PR interval, QT interval, and QRS duration at the beginning of treatment in two groups. There was no significant difference between the two groups thus at the baseline both the groups were comparable. During the trial there were no significant changes in all above parameters.
There was no significant difference in T wave amplitude between the two groups thus at the baseline both the groups were comparable. During the trial the decrease in T wave amplitude with lithium is in agreement with current literature. Similar findings have also been reported by Schou et al., [14], demers et al., [15], dermers et al., [16], Tilkian et al., [17], Dumovic et al., [18], in their respective studies. These T wave changes can be ascribed to intracellular potassium displacement by lithium carbonate- an explanation well documented by Mary et al., [19].
[Table/Fig-16] show the comparison of P wave amplitude during the trial in two groups on 1st, 7th day and 28th day. There was no significant difference between two groups.
The findings of this study should be seen in the light of the fact that these patients were permitted concurrent administration of haloperidol for controlling the symptoms of acute mania. Thus ECG changes in Group A and Group B were not because of lithium or verapamil given alone. For ethical reasons the study design permitted freedom to clinician to treat the patients in the best possible way and use haloperidol was common to both groups, thus the difference in outcome in the study parameters is ascribed to the trial drugs. The freedom from cardiovascular side effects with verapamil as seen in the electrocardiographic parameters in this study is in agreement with available literature. Gianni et al., in single blind placebo control crossover study of 30 d did not report any cardiovascular side effects with verapamil [7].
Gianni et al., [6] in another double blind crossover study in a selective population did not report any cariodvascular event with verapamil. Hoschi and kozeny also reported safe use of verapamil in treatment of bipolar affective disorder [20].
Garza Trevino conducted a randomized double blind study to evaluate the efficacy of verapamil 320 mg/day. The author reported no cardiovascular event with verapamil treatment. This is also in agreement with present study [12].
Conclusion
Verapamil, which has been used as an alternative to lithium in acute mania produced a greater decrease in heart rate as compared to lithium. The risk of bradycarida occurring in such patients being treated with verapamil should be kept in mind. The baseline electrocardiogram should be done and heart rate should be monitored during the treatment. It is further suggested that other cardiovascular depressant drugs should be ruled out while using verapamil as an antimanic drug.