Filariasis, transmitted by the bite of various species of mosquito, is a global health problem of tropical belt of the world. It is a major health problem in South East Asia, including India [1]. It affects over 120 million people in 80 countries. The disease is endemic all over India except some parts of Northern India (Delhi, Rajasthan, Haryana, Punjab and Himachal Pradesh) and Northeast India (Nagaland, Manipur, Tripura, Sikkim & Arunachal Pradesh) [2]. In India, there are at least 600 million people at risk of lymphatic filarial infection and at least 735 thousand have lymphoedema and another 336 thousand have hydrocele [3]. The parasite is primarily confined to Lymphatic channel or lymph nodes where it can remain viable for more than two decades. The most common presentation of the disease is asymptomatic/ subclinical microfilaremia, Hydrocele, acute adeno-lymphangitis (ADL) and chronic lymphatic disease [1]. Demonstration of microfilaria in peripheral blood smear is used for diagnosis of filariasis. It is rare to find microfilariae in fine needle aspiration cytology (FNAC) smears even in endemic areas. The aim of present study was to assess the role of FNAC in diagnosis of filariasis in asymptomatic patients having palpable swellings.
Materials and Methods
This retrospective study was conducted in the Department of Pathology, Dr. B.S. Ambedkar Hospital, Delhi, which caters primarily to the sub-urban population of North Delhi, India. A large number of migrant populations from nearby states of Delhi reside in the area. The study was done on FNAC carried out on superficial swellings in the department over last ten years from April, 2003 to March 2013. The records of all those cases finally diagnosed as filariasis on FNAC, with or without any associated pathology, were retrieved.
During this period, a total of about 25,468 FNACs were carried out on superficial swellings/ clinically palpable swellings from various sites. There were 12,684 cases of lymph node swellings, 4,572 cases of breast lumps, 3,823 cases of thyroid swellings, 2,984 cases of soft tissue swelling and 50 cases of scrotal swelling. There were 1,355 cases of palpable swelling which fell into miscellaneous group including swellings in oral cavity.
FNAC were done using 10 ml syringe and 22 gauge needle under aseptic precautions. Aspirated material was spread on slides. In case of cystic lesions, cyto-centrifugation of fluid was carried out and repeats FNAC from the residual swelling was also carried out. Air dried smears were stained with Giemsa stain. Out of all these cases of FNAC, there were incidental findings of microfilaria in 20 cases. All these slides were reviewed again to reaffirm the diagnosis of filariasis.
Results
The incidental finding of microfilaria was found in 20 cases accounting for only 0.078% of total FNACs carried out at the center. Out of these 20 cases of superficial swellings diagnosed as filariasis on FNAC, there were 17 cases in third and fourth decades of life. There were only three cases in 5th decade of life while no case was seen below the age of 20 years. The disease was equally prevalent in males and females (M: F = 1:1). The records revealed that in none of the situation, the clinical diagnosis of filariasis was made by the clinicians. It was only after diagnosis on FNAC, treatment for the disease was started.
All the patients presented to the clinician with history of slowly growing swelling. The size of swelling ranged from 1 cm to 10 cm. While four of the 20 cases had history of fever, seven patients complained of some degree of pain. Two patients had associated complaint of infertility with testicular swelling. The duration of disease ranged from weeks to years.
Out of the 20 cases of superficial swellings diagnosed as filariasis on FNAC, the commonest site involved were swellings from testiculoscrotal region (six cases) (12% of total cases of Testiculoscrotal swelling) and lymph nodes swellings (six cases) (0.047% of the total cases of lymph node swellings). Three cases of filariasis were diagnosed on thyroid swelling (0.08% of thyroid swellings), three cases on soft tissue swelling (0.10% of soft tissue swellings) and two cases of filariasis on breast lumps (0.044 of breast lumps).
Peripheral smears showed eosinophilia in seven cases. Out of these seven cases which showed eosinophilia (ranging from 10 to 39%), three cases had lymph node enlargement, and three had soft tissue swelling while one patient had presented with breast lump. Microfilaremia was detected in three cases, one case each of lymph node swelling, testiculoscrotal swelling and soft tissue swelling [Table/Fig-1].
Clinical and haematological presentation of filariasis (n=20)
| Clinical & hematological findings | Lymph nodes | Testiculoscrotal region | Soft tissue | Thyroid | Breast | Total |
|---|
| Palpable Swelling | 6 | 6 | 3 | 3 | 2 | 20 |
| Fever | 2 | 0 | 1 | 0 | 1 | 4 |
| Pain | 2 | 2 | 2 | 0 | 1 | 7 |
| Associated complaints | 0 | Hydrocele (2) | 0 | Nodular enlargement (2) diffuse | 0 | 0 |
| | Primary infertility (2) | | Hyperthyroidism (1) | | |
| Peripheral blood smear- |
| Eosinophilia | 3 | 0 | 3 | 0 | 1 | 7 |
| Microfilaremia | 1 | 1 | 1 | 0 | 0 | 3 |
On FNAC, clear fluid was aspirated in 10 cases, blood mixed in six and purulent in two. Colloid was aspirated in two cases of thyroid swellings. Granulomas were seen in two cases- one each in a thyroid aspirate and a soft tissue swelling aspirate. Reactive lymphoid cells were seen in two cases from lymph node. Secondary maturation arrest was seen in aspirate from the atrophic testis in case of a spermatic cord nodule. Aspirate from spermatic cord nodule revealed few microfilaria. One of the aspirates from thyroid showed features of lymphocytic thyroiditis, while the other two showed features of colloid goiter with only an occasional microfilaria. Only few clusters of benign ductal epithelial cells were seen in one of the two breast aspirates along with microfilaria. Cell adherence of inflammatory cells and macrophages to microfilaria was seen in four out of 20 cases [Table/Fig-2].
Aspirate morphology and background Cytology: (n=20)
| Lymph nodes (6) | Testiculoscrotal region (6) | Soft tissue (3) | Thyroid (3) | Breast (3) | Total |
|---|
| Nature of aspirate from swelling |
| Clear Fluid | 4 | 2 | 3 | 0 | 1 | 10 |
| Hemorrhagic | 1 | 3 | 0 | 1 | 1 | 6 |
| Pus like | 0 | 2 | 0 | 0 | 0 | 2 |
| Colloid | - | - | - | 2 | - | 2 |
| Special associated features on microscopy |
| Granulomas | 0 | 0 | 1 | 1 | 0 | 2 |
| Other Features | Florid Reactive hyperplasia (2) | Secondary maturation arrest (2) | -- | Colloid Goitre(2) Lymphocytic Thyroiditis (1) | {Cluster of benign ductal epithelial cells (1)} | |
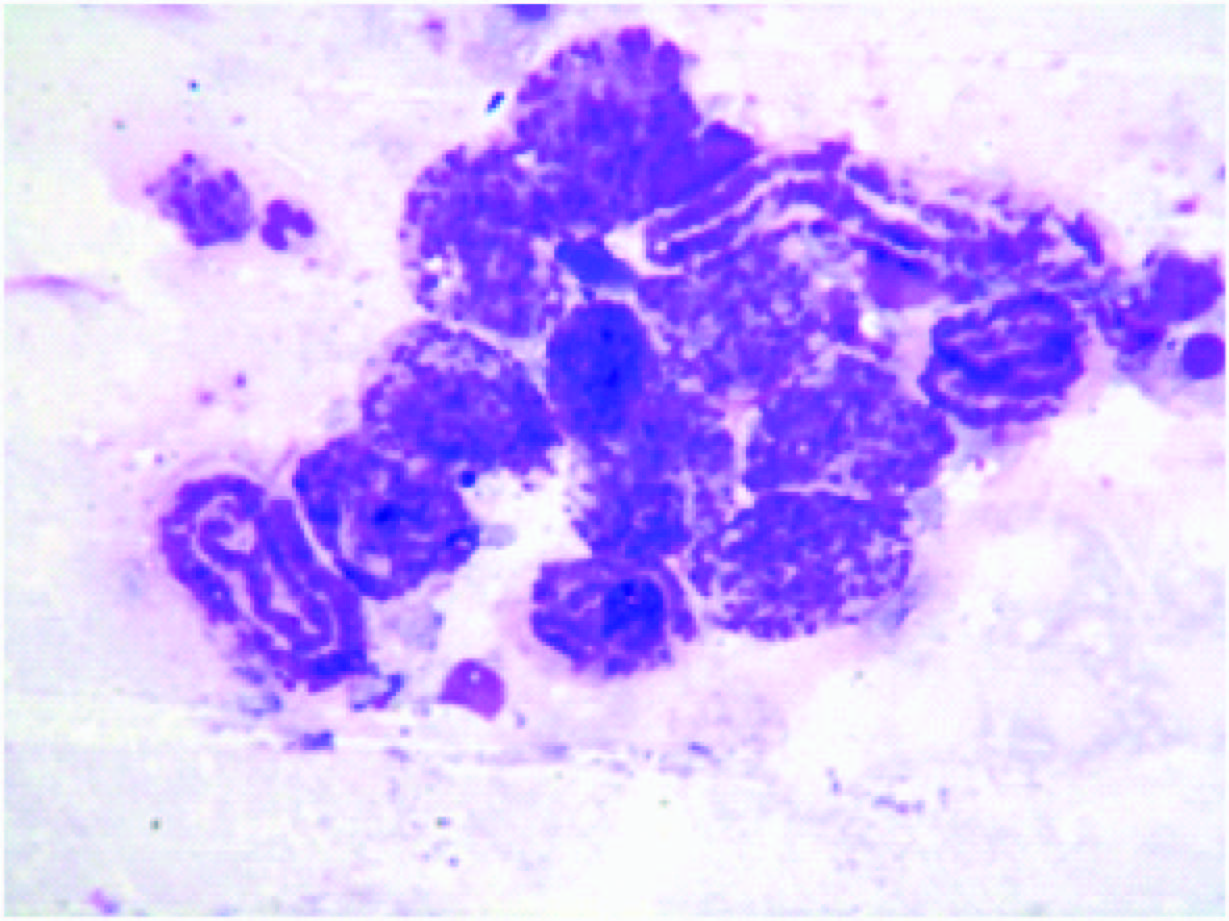
Smears prepared from aspirates revealed sheathed microfilariae with a central column of nuclei. Cephalic and tail ends were free from nuclei (somatic cells). The number of microfilariae varied from single to numerous (over 100s) per slide. Many coiled larvae were seen in four cases and embryoid bodies were seen in three cases. Adult worms were seen in two cases [Table/Fig-3]. Adult gravid female worm with embryoid bodies and discharging numerous larvae were seen in two cases. Adult male worm was seen in one case. The male worm was thinner and smaller than the female worm. The causative agent in all the cases was Wuchereria bancrofti [Table/Fig-3].
Anatomical sites and stages of filaria parasite seen on FNAC: (n=20)
| Anatomical site | Microfilaria | Eggs | Adult worm | Total cases |
|---|
| Lymph nodes (6) |
| Axilla | 4 | 1 | 0 | 4 |
| Cervical | 2 | 0 | 0 | 2 |
| Testiculo-scrotal region (6) |
| Scrotal | 2 | 0 | 0 | 2 |
| Epidydmal Nodule | 3 | 1 | 1 | 3 |
| Spermatic Cord Nodule | 1 | 0 | 0 | 1 |
| Soft tissue (3) |
| Arm | 3 | 0 | 1 | 3 |
| Breast (2) | 2 | 1 | 0 | 2 |
| Thyroid (3) | 3 | 0 | 0 | 3 |
Discussion
Filariasis is a major public health problem in tropical countries, including India. It is caused by nematodes Wuchereria bancrofti, Brugia malayi, B. timori, Loa-loa, Onchocerca volvulus, Mansonella perstans, M.ozzardi and, M.ozzardi [1]. Wuchereria bancrofti (95%) and Brugia malayi (5%) are the most common species causing filariasis in India [2]. Adult worms live in the lymphatic channels of the definitive host and microfilaria is released and circulated in the peripheral blood. Female W. bancrofti measures 80–100 × 0.25 mm and the male 40 × 0.1 mm. The disease most frequently involves lymphatics of lower limbs, retroperitoneal tissue, spermatic cord, epididymis and mammary gland [4,5].
At our institution from April, 2003 to March, 2013, a total of 25,468 were carried out from superficial sites. Microfilaria can be easily diagnosed using hematoxylin stain, Giemsa stain or methylene blue and eosin. We have been using Giemsa stain at our centre. The incidence of detection of microfilaria was only 0.078% (Total 20 cases). In none of those situations, the patient was referred for FNAC with the suspicion of Filariasis as primary diagnosis. Presence of microfilaria at these sites was more of an incidental finding. Similar observations of very low detection rate of microfilaria from superficial sites have been reported by some authors [6]. In our study, the causative agent in all cases was W. bancrofti similar to the national survey in India which puts estimates of 95% cases caused by W. bancrofti [3].
Six cases of swellings in testicular-scrotal region showed microfilariae [Table/Fig-4]. Thus, there was significant incidental detection of microfilaria on FNAC in cases of these swelling (12% of the total 50 cases of testiculoscrotal swellings). Most of Indian studies have also reported testiculoscrotalregion as a common site for complications of Filariasis in India [2]. The lymphatic vessels of spermatic cord appear to be common and perhaps the principal site of adult Wuchereria bancrofti in men with asymptomatic microfilaremia. Occurrence of living W. bancrofti in scrotal area of men was also reported [6–8]. We had two cases where adult worm was detected in testiculoscrotal swellings. Noroes et al., [9] also reported a case of adult worm W. bancrofti in scrotal swelling. Two of the cases in our series came to the hospital with primary complaint of infertility but records did not support filariasis as an etiological cause of infertility.
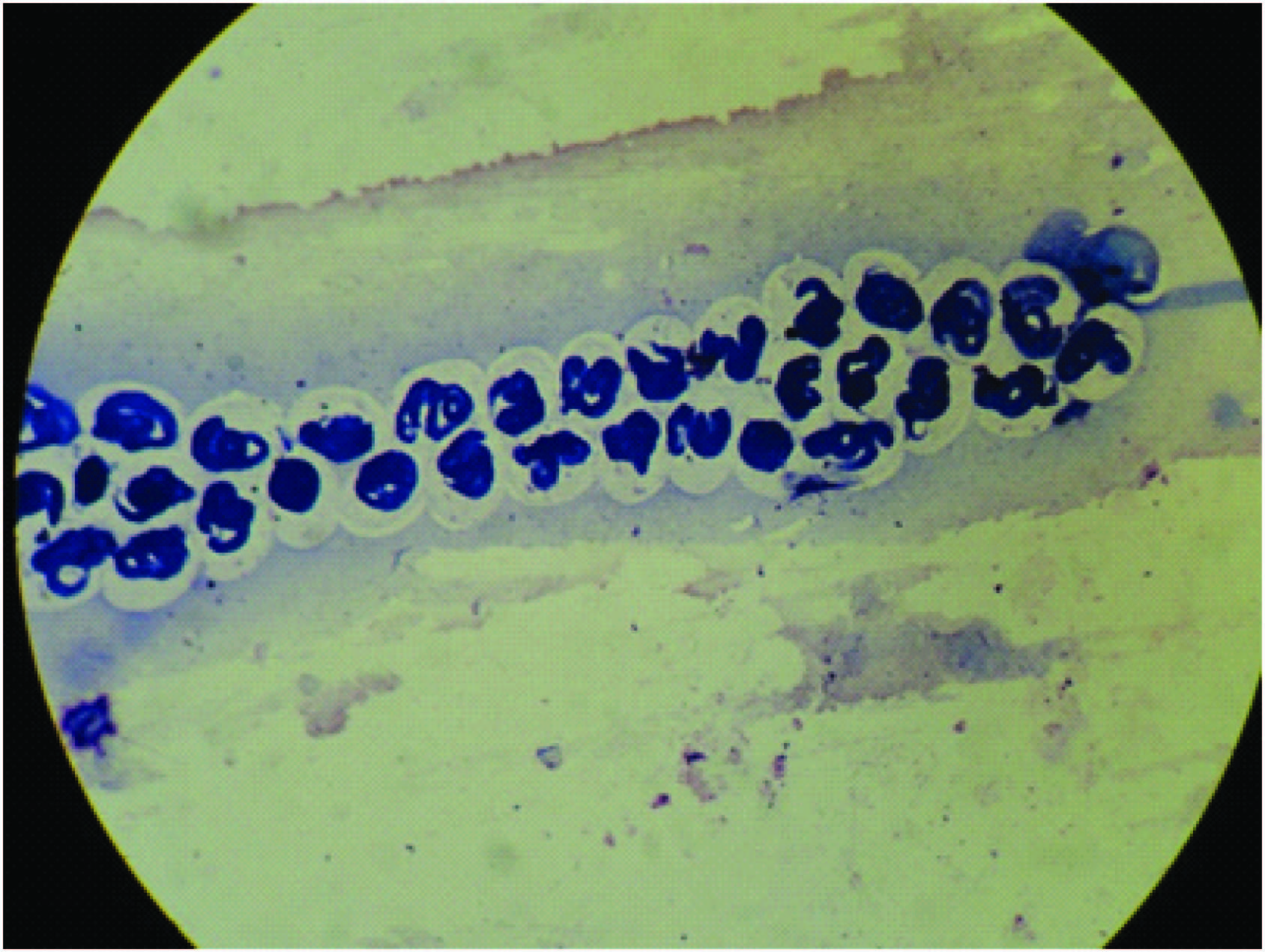
40x10X Aspirate from epididymal nodule showing coiled microfilarae and embryonated eggs
Six cases of superficial lymph nodes (4 axillary and 2 cervical) accounted for 30% of the total diagnosed cases. Aspirates from lymph nodes demonstrated microfilariae in a background of reactive lymphoid cells. Similar observations in many case reports have been noticed in literature [5,6,8,10].
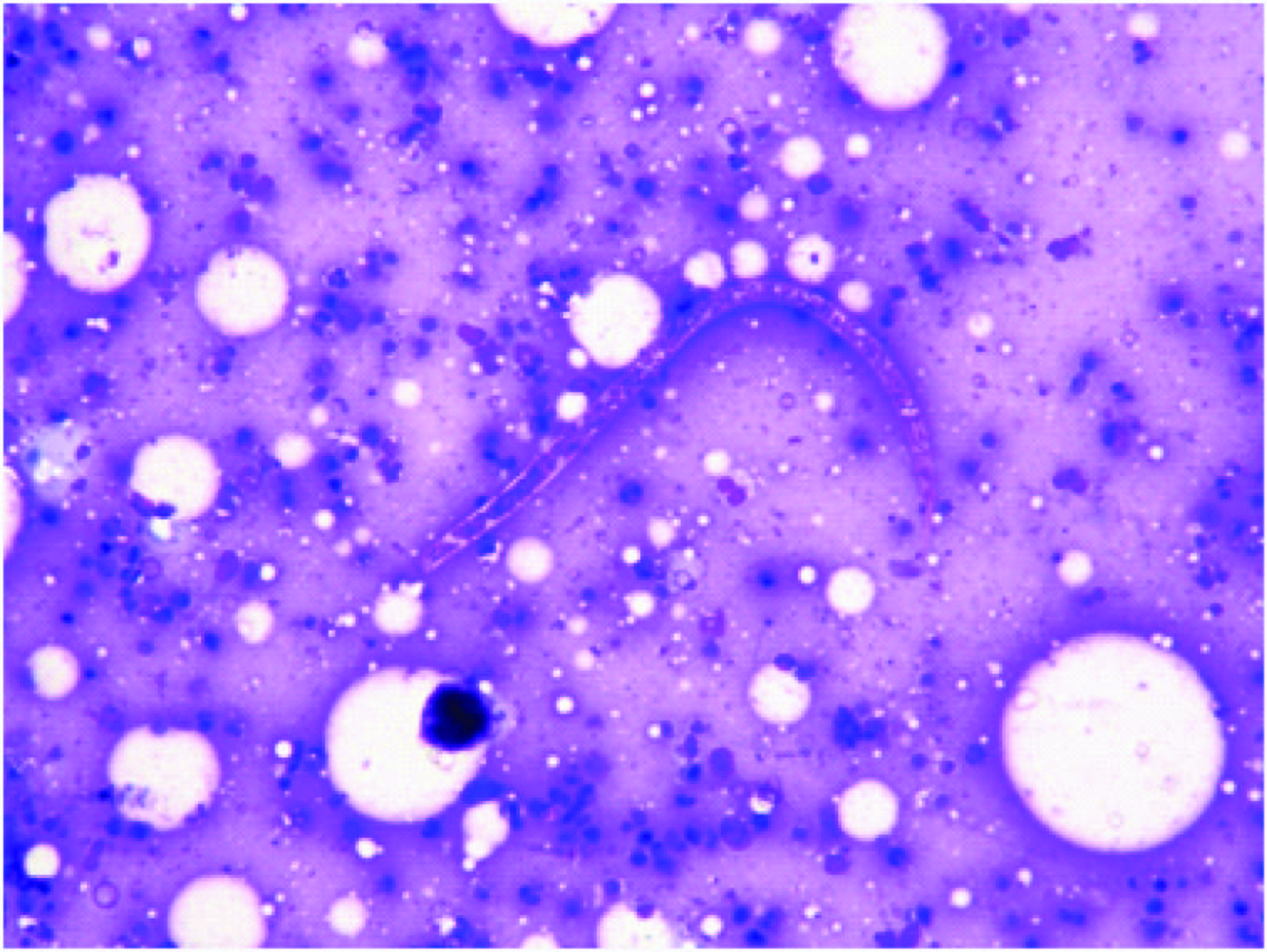
Breast lumps are a very rare site for detection of microfilaria. We had only two cases of breast aspirates [Table/Fig-5] which showed microfilaria out of 4,572 breast lumps. There are few isolated reports of incidental finding of microfilariae in breast lumps on FNAC smears [7,10,11].
20x10X Aspirate from breast lump showing ensheathed microfilaria of W. bancrofti in the background of acute inflammatory cells
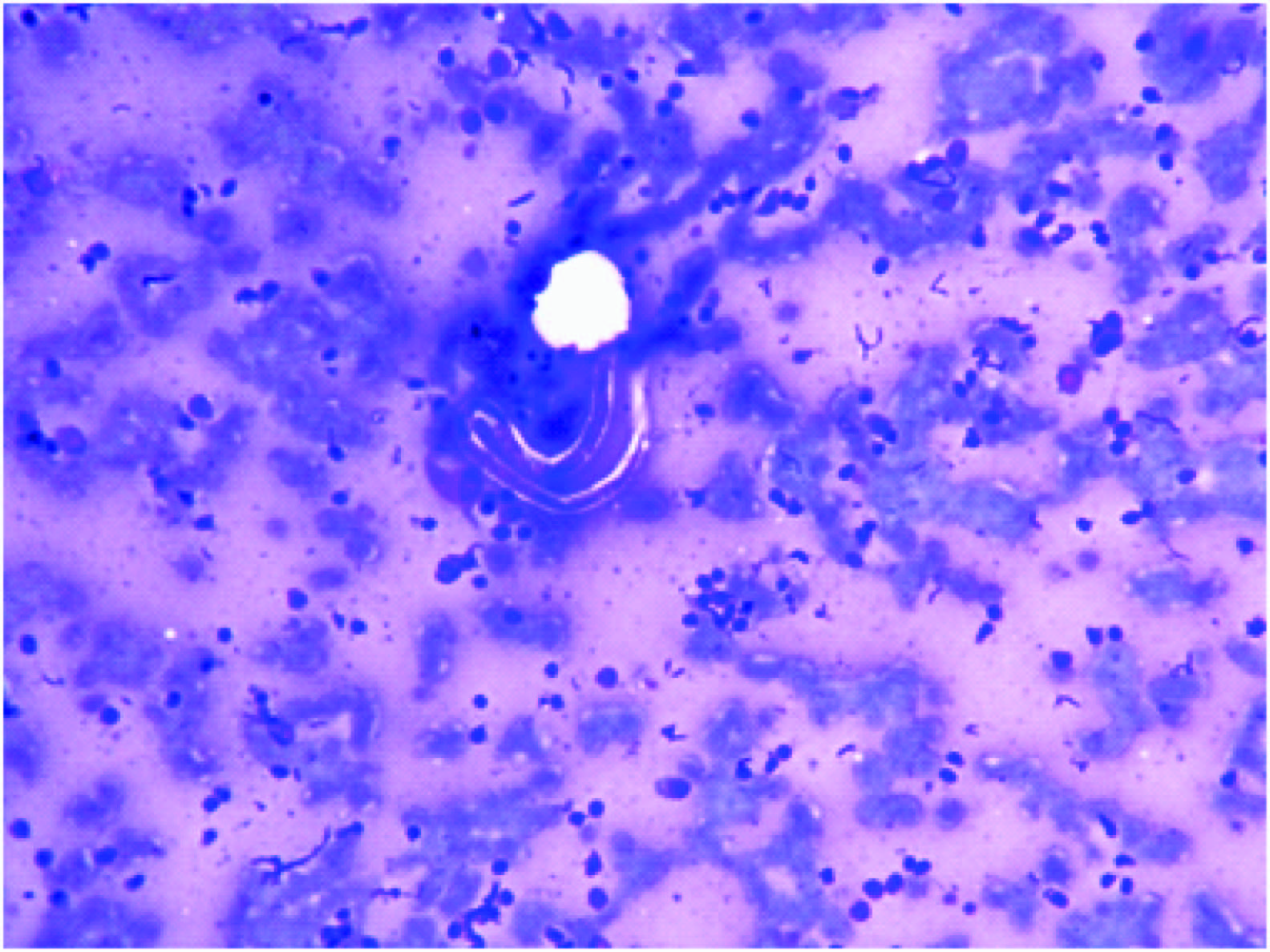
Demonstration of microfilaria in Thyroid swelling is also very unusual. Presence of microfilaria have been reported in thyroid by Yenkeshwar et al., [5], Kishore et al., [7] Varghese et al., [10] and Chowdry et al., [12]. We had three such cases amongst 3,823 of thyroid swelling subjected for FNAC. Whereas one thyroid aspirate showed microfilaria in a background of lymphocytic thyroiditis, while the two revealed microfilaria in a background of colloid goiter [Table/Fig-6].
20x10X Ensheathed microfilaria of W. bancrofti in a background of reactive lymphoid cells & colloid in a thyroid aspirate
Aspirates from soft tissue swelling in arm showed microfilaria in four cases. In one of these cases adult gravid worm and eggs were also seen [Table/Fig-7a,7b]. The incidence of finding microfilaria in soft tissue swellings is very low. Demonstrations of microfilariae from similar sites have also reported by other workers [5,8,13]. Out of 20 cases showing microfilariae in FNAC smear examination, blood eosinophilia was present in 35% cases (seven cases). Three of these seven cases showed microfilaremia in nocturnal venous blood smear examination, accounting for only 15 % of the total 20 cases diagnosed on FNAC. Findings are consistent with observation made by others [8,14]. Thus, we conclude that in a large number of cases, filariasis can occur even without microfilaraemia.
40x10X Aspirate from soft tissue swelling showing adult gravid worm with numerous eggs
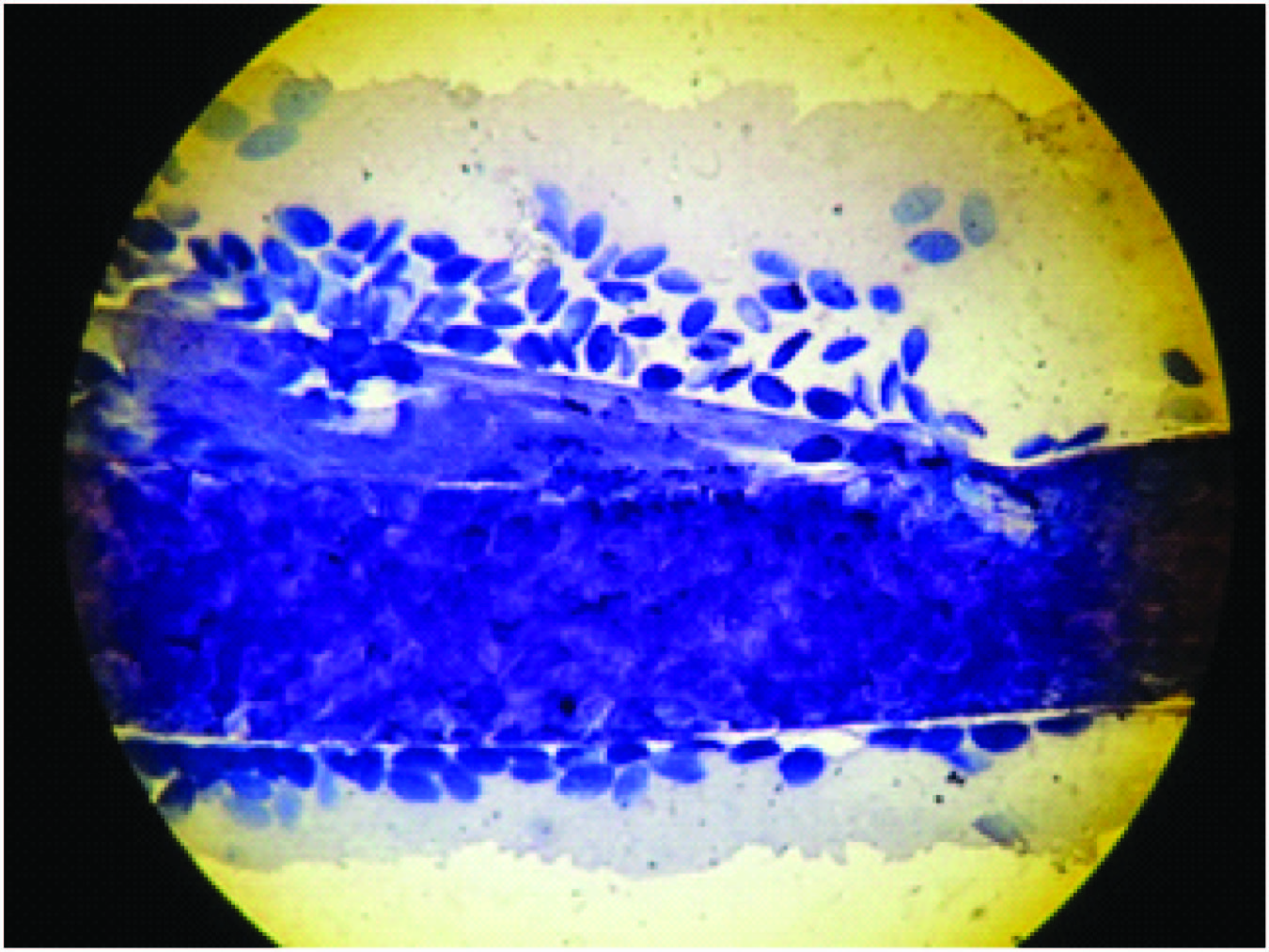
40x10X Another field of same slide Fig 4(a) showing numerous coiled microfilarae
Significant adherence of inflammatory cells and macrophages to microfilariae was present in four out of 20 cases. Cell adherence to microfilaria of W. bancrofti was reported by other workers also [8,15].
Recently, specialized test based upon principles of immune-chromatography, Polymerase chain reaction (PCR) and Enzyme linked immunosorbent assays (ELISA) with high sensitivity and specificity [16] have been introduced but still the gold standard for confirmed diagnosis is demonstration of the microfilaria in the smear.
Conclusion
To conclude, in this retrospective study we observed that there is a significant possibility of finding microfilaria in patient with testiculoscrotal swellings and clinician should always consider its possibility in these cases. However, despite high incidence of filariasis in an endemic country like India, detection of microfilaria in other superficial locations on FNAC is rare. Careful screening of FNAC smears is very important as it provides definitive diagnosis of filariasis even in situations where the clinician has not suspected the disease. The prompt recognition and administration of specific treatment can help preventing the severe manifestations of lymphatic filariasis.