Introduction
Adnexal torsion is one of the few gynaecological surgical emergencies. Ovarian torsion is defined as partial or complete rotation of the ovarian vascular pedicle causing obstruction to venous outflow and arterial inflow [1]. When fallopian tube also twists with the ovary it is known as adnexal torsion [2]. Adnexal torsion mostly occurs in the child bearing group, but is not uncommon in premenarchal girls or postmenopausal women [3]. It is usually associated with a cyst or a tumour, the most common being mature cystic teratoma [1]. As the symptoms are nonspecific it can lead to delay in diagnosing adnexal torsion. Laboratory investigations and imaging using Doppler scan, CT, MRI helps in diagnosis. However surgical intervention, preferably by laparoscopy is the gold standard for diagnosis and treatment of adnexal torsion. Conservative surgery such as detorsion with cystectomy or cyst aspiration is preferred to removal of the adnexa when possible.
Materials and Methods
This study was undertaken after clearance from the ethical committee of Amrita Institute.
A retrospective analysis of our hospital surgical registry for the year 2008-2013 identified records of 70 patients with surgically proven adnexal torsion. Clinical information obtained from the patients’ medical records included age, medical history, clinical signs and symptoms. Abdominal pain was defined as lower abdominal pain {pelvic}, diffuse pain and epigastric pain. The onset of pain till admission to the hospital was noted in days. Duration of associated symptoms was recorded in days. Fever with the body temperature exceeding 37.7oc [4] and Leukocytosis when WBC counts greater than 10,800/mm3 was considered as clinically significant values [5]. Imaging, operative findings and histopathological reports were obtained from the case records.
Statistical Analysis
Statistical analysis was performed with SPSS statistics 20. All continuous parameters are presented as means ± SD. All categorical parameters as presented in percentage .Comparing the average of parameters between two groups, those following the normal distributions independent sample t-test was used. Those not following the normal distributions, Mann Whitney U-test were used. Chi-Square Test was used to find the association between two categorical variables. p-value < 0.05 is considered as statistically significant.
Results
Clinical Presentation
The median age of the patients was 25.5 y (11-91y). Two out of the 70 patients were pre menarchal (2.9%) and 12 were postmenopausal women (17.1%). Lower abdominal pain was the main symptom seen. Apart from pain, other clinical signs and symptoms were nausea, vomiting, dysuria, urinary retention, diarrhea, constipation, vaginal spotting and menorrhagia. We had two cases (2.9%) of early weeks of pregnancy with torsion. Torsion occurred in 35 cases (50%) during post ovulatory period and 17 cases (24.3%) during pre ovulatory period. Two cases were asymptomatic in whom ovarian cyst was incidentally detected by ultrasound during health check up.
In our patients palpable mass was seen in 30 cases (42.9%) with tenderness in 18 cases (25.7%) and Leukocytosis in 31 cases (44.1%). Anaemia was reported preoperatively in three cases and required blood transfusion.
Ultrasound was performed in all cases and adnexal mass was reported in 69 (98.6%) with diagnosis of torsion in four. Doppler was done only in 21 cases and torsion was diagnosed in 14 cases. CT scan done in 13 cases (18.6%) with diagnosis of torsion made in three. MRI was done in seven cases (11.4%) in which three were diagnosed as torsion. The other ultrasound findings were ovarian cyst in 32 cases (45.3%), ovarian cyst with free fluid in 12 cases (16.8%), complexcyst, hemorrhagiccyst, dermoidcyst and multiloculated cyst.
Polycystic ovaries were diagnosed in the contra lateral ovary by imaging in14 cases pre operatively [Table/Fig-1] and four cases in the follow up period. Of the 18 cases (25.7%) diagnosed as polycystic ovaries, 10 cases had tumours also as another risk factor for torsion.
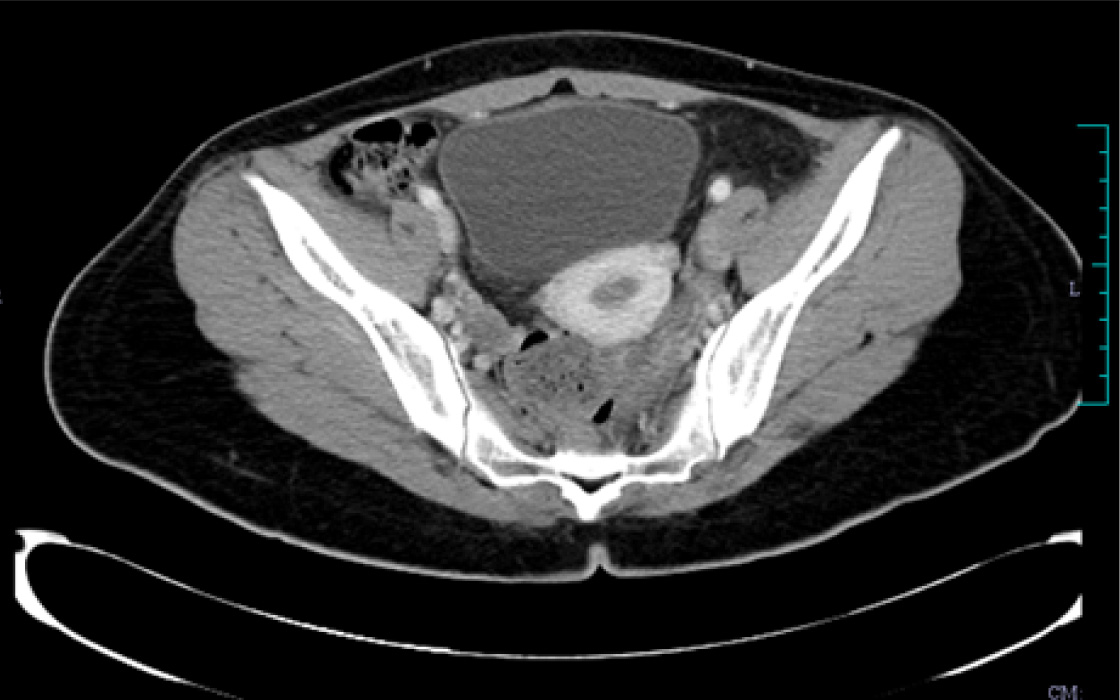
CT Scan
A 20-year-old presented with abdominal pain of two days duration. CT scan showed torsion of left ovary 7x5x5cm with polycystic right ovary.
Surgery
All the patients under went surgical procedure in which 13 cases (18.6%) had laparotomy and 57cases (81.4%) underwent laparoscopy. The surgical findings were isolated torsion ovary in 40cases (57.1%), combined ovarian and fallopian tube 15 (21.3%), isolated tubal torsion in 5 cases (7.1%) and paraovariancyst/ paratubalcyst in 10cases (14.3%). The risk factors for adnexal torsion found in our study were tumours, adhesions, hydrosalpinx and polycystic ovaries.
The size of the mass in adnexal torsion was <5cm in 12 cases (17.1%), 5-10 cm in 50 cases (71.4%) and > 10 cm in 8 cases (11.4%). Right sided torsion was seen in 39 cases (55.7%), left sided in 30 cases (42.9%) and bilateral in 1case (1.4%), who was a postmenopausal woman with adnexal mass on both ovaries.
Detorsion was done in 1case (1.4%), detorsion with cystectomy in 37(52.9%), salpingoophorectomy in 18 cases (25.7%), salpingectomy in 5 cases (7.1%), abdominal hysterectomy with BSO in 6cases (8.6%) and lap hysterectomy with BSO in 3 cases (4.3%).
In spite of bluish- black appearing ovaries conservative surgery was done in 5 cases. Follow up over a period of 6months to 2 years by Ultrasound was done in all five cases. Ovarian function was assessed by the presence of follicles.
Pathological examination of all specimens was done. Results are revealed in [Table/Fig-2].
Discussion
Awareness and high level of clinical suspicion of adnexal torsion with imaging helps in early diagnosis and appropriate management of the condition. Delay in the diagnosis is due to nonspecific symptoms and varied imaging.
Even though adnexal torsion occurs in all age groups, it is most commonly seen in reproductive age groups [6,7]. In this study also majority of the torsion was seen in younger age groups [Table/Fig-3].
Lower abdominal pain (87.1%) was the main symptom. Other associated symptoms and signs were nausea and vomiting, lower urinary symptoms, fever, leukocytosis, palpable mass, tenderness and vaginal bleeding [Table/Fig-4]. In a study of 179 patients, the clinical features of pelvic pain was found in 82%, nausea/vomiting in 49%, leukocytosis in 20.1%, fever in 7.8% and lower urinary symptoms in 14.5% [8].
Very rarely torsion may result in anaemia due to haemorrhage and may require blood transfusion [9]. We had three cases of anaemia (4 gm%, 7gm%, 8gm%) which required blood transfusion. One of our patients with hemorrhagic necrosis had an Hb of 4gm% [Table/Fig-5].
CT scan- 25 year old presented with abdominal pain and distension of 5 days, vomiting and urinary retension of 1day duration and her Hb was 4gm%. CT scan suggestive of hemorrhagic cyst 26x10 cm. Intra operative diagnoses was left sided ovarian torsion with hemorrhagic necrosis.
Yet another complication of torsion is adnexal necrosis. This may result in infection with associated leukocytosis.
Maternal ovarian torsion during pregnancy is a rare event and occurs mainly in the first trimester. We had two cases of early pregnancy (5-6 wk) with ovarian torsion and they underwent elective abortion. The incidence of torsion with pregnancy was low (<6%) as seen in the other study [10] [Table/Fig-3].
Torsion occurred in the postovulatory period in most of the cases. It may be due to pelvic venous congestion at the time of ovulation or pre-menstrual phase that causes torsion [11].
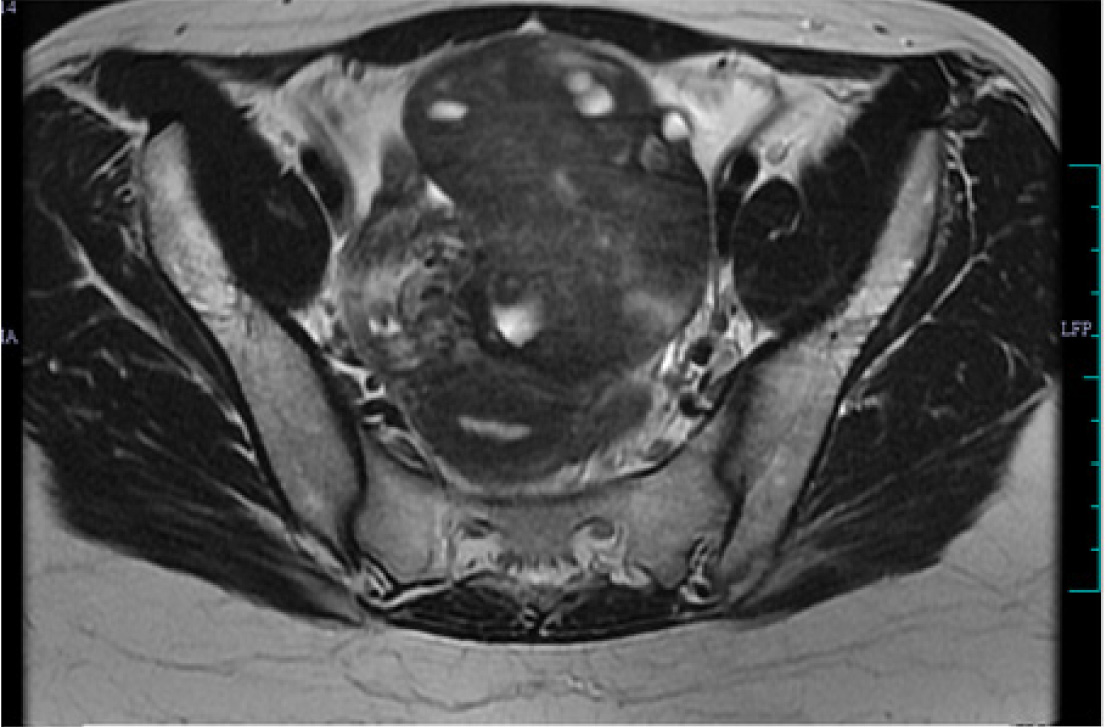
The sensitivity of ultrasound in diagnosing torsion ranges from 40-75% [12]. Twisted adnexal masses are often mid line, located anterior to the uterus and the other findings are cystic, solid or complex mass with or without pelvic free fluid, thickening of the wall and cystic haemorrhage. Multiple peripheral cysts in the setting of pain with a unilateral enlarged ovary are helpful in diagnosing torsion [13]. Two small series of 20 patients with suspected torsion found whirlpool sign (twisted vascular pedicle) to have a sensitivity of more than 90% for diagnosing torsion [9,16]. We could diagnose adnexal torsion in 75% of cases intra operatively by direct visualization of rotated adnexa. Torsion was diagnosed by ultrasound with doppler in 25.7%, CT scan in 4.3% and MRI [Table/Fig-6] in 4.3% of cases performed under the respective imaging in our study. In a study of 35 patients of adnexal torsion, correct diagnosis by clinical and sonography was only in 26% and with CT scan in 34% of cases [17].
Twenty three year old with right sided lower abdominal pain and vomiting of two days duration. MRI reported-torsion right ovary 8x7x6cm.
Ovarian mass is the primary risk factor for torsion. Few case series have reported that there is more likelihood of torsion [18] when the size of the ovarian mass is 5cm or larger. Adnexal mass were seen in 98.6 % in this study. There were 50 cases (71.4%) between the sizes of 5-10 cm which had undergone torsion [Table/Fig-3].In about 34 [48.6%] cases tumours was found to be a risk factor for torsion. 11 cases (15.7%) there was no risk factor for torsion. Others had a combination of adhesions, hydrosalpinx and polycystic ovaries as a risk for torsion.
Torsion of the right ovary was more common than the left, probably due to presence of sigmoid on left and longer right ligament of ovary [19]. In our study the adnexal torsion of the right side was about 55.7% when compared to the left side [Table/Fig-3].
Unexplained ovarian torsion in adolescents and young adults with PCOD has been reported [20]. Our data also showed few cases of polycystic ovaries which have undergone torsion.
Isolated torsion of the fallopian tube is less common, but may also occur and adversely impact the tubal function [21]. Isolated tubal torsion associated with hydrosalpinx were seen in 69% of cases and salpingectomy was performed in 11/13 cases in a study [22].We had 5 isolated tubal torsions and the risk factors seen were paraovarian cyst and hydrosalpinx. All five underwent lap salpingectomy as the tubes were non-viable [Table/Fig-7].
Torsion of paratubal or paraovarian cyst may also occur and they increase the risk of tubal torsion [23]. Torsion of Para ovarian/tubal cysts was present in 10 cases in our study.
Laparoscopy is the recommended procedure for adnexal torsion as it gives better visualization, shorter hospital stay, fewer postoperative complications, small scar, less blood loss and analgesia requirement [6,24]. Laparoscopy was done in 81.7% of the torsion cases in our study and was found to be a reliable method [Table/Fig-8].
Over the past years, salpingoophorectomy was the standard treatment for adnexal torsion due to fear of thromboembolism. But recent studies suggest a conservative approach of detorsion with ovarian cystectomy for benign tumours [24]. Salpingoophorectomy is preferred in post menopausal women, suspected malignancy and non-viable ovary [3]. We did radical surgery in 11 (15.7%) postmenopausal women who had torsion. We could do conservative procedure in 35 patients (71.45%) who were below 40 y.
Hemorrhagic necrosis was seen in 21 cases (30.4%) of which 5 cases (23.8%) underwent ovarian cystectomy and 16 cases (76.2%) underwent radical surgery [Table/Fig-9]. Various studies have shown that even though the adnexa appear blue or black, it does not imply that it is nonviable and hence detorsion is done to retain the ovarian function [3,24,25].
The reported pathology in our study was benign in 66cases (94.3%) and malignant in 4 cases (5.7%). Due to fixity and adhesion, malignant as well as endometriotic cyst rarely undergoes torsion [3]. Case series have reported about malignancy in 2% or fewer of the cases of torsion [6][18]. Torsion are more likely to occur in an underlying ovarian lesion such as a tumour or cyst [1]. As consistent with various studies, in our study also teratoma (22.8%) was the commonest benign neoplasm for the ovarian torsion [17] [Table/Fig-3,Table/Fig-8].
The complications of torsion we had were anaemia (3 cases), hemorrhagic necrosis (21 cases) and 1case each of paraovarian and ovarian abcess. During the postoperative period there were three superficial wound infections, all of them responded with antibiotics. A 16-year-old girl who was a known case of Kartageners syndrome died on second postoperative day after salpingo ophorectomy done for teratoma with extensive hemorrhagic necrosis.
As the time interval between symptoms to surgery is prolonged, the rate of ovarian conservation is reduced [26]. The time interval from admission to the surgery in our patients was 24h (median) and 38 cases (54.3%) had conservative surgery. In a study of ovarian torsion in children, the time interval was 20.75 h (median) and 80.4 % of cases were treated conservatively [24][Table/Fig-8].
Even though an ovary has undergone hemorrhagic necrosis, it regains ovarian function as demonstrated by presence of follicles in sonography [27]. Out of the 5 cases we had on follow up of 6 months to 2 years, 4 had follicles and 1 ovary with no blood flow [Table/Fig-10].Traditionally, necrotic appearance has been synonymous of oophorectomy; however current trend depends ovary preservation [27].
CT scan showed torsion of left ovary
Pathological examination of specimens
| Benign RETE cyst | 1 | 1.4% |
| Borderline serous cyst adenoma incystadenofibroma | 1 | 1.4% |
| Cystic follicle | 2 | 2.9% |
| Teratoma,hemorrhagic necrosis | 3 | 4.3% |
| Teratoma | 13 | 18.6% |
| Immature teratoma grade 3 ,hemorrhagic necrosis 1 | 1 | 1.4% |
| Serous cyst adenoma | 11 | 15.7% |
| Mucinous cyst adenoma | 5 | 7.1% |
| Endometriotic cyst | 2 | 2.9% |
| Hemorrhagic necrosis | 12 | 17.1% |
| Fimbrial cyst | 1 | 1.4% |
| Follicular cyst | 2 | 2.9% |
| Paraovarian cyst | 4 | 5.7% |
| Paraovarian cystadenofibroma | 1 | 1.4% |
| Paraovarian abscess with paraovarian cyst | 1 | 1.4% |
| Paratubal cyst, hydrosalpinx | 1 | 1.4% |
| Paratubalcyst,hemorrhagic necrosis | 1 | 1.4% |
| Paramesonephric cyst, hemorrhagic necrosis, torsion tube | 1 | 1.4% |
| Hemorrhagic necrosis ,torsion tube, hydrosalpinx | 1 | 1.4% |
| Hemorrhagic necrosis, torsion tube | 1 | 1.4% |
| Dysgerminoma ,hemorrhagic necrosis | 1 | 1.4% |
| Poorly differentiated sex cord tumour | 1 | 1.4% |
| Sclerosing stromal tumour, hemorrhagic necrosis | 1 | 1.4% |
| R –Papillary serous cystadenofibroma L-Serous cyst adenoma | 1 | 1.4% |
Our study compared with other studies
| Our study | Kandasami Vijayalakshmi et al., [7] | C Spinelli et al., [14] | Vijayaraghavan [15] |
|---|
| No: of patients | 70 | 18 | 30 | 21 |
| Age | 11-91y | 25-72y | 2months -18y | 7-69y |
| Reproductive Age <45yrs | 82.6% | 66.7% | | |
| Parity | 50% | 88.9% |
| Pregnancy | 2.9% | | | 4.7% |
| Menopause | 17% | 11% | | |
| Pain abdomen | 95.7% | 77.8% | 100% | 100% |
| Nausea/Vomiting | 65.7% | 27.8% | 56.7% | |
| Fever | 12.9% | 5.6% | 20% | |
| leukocytosis | 44% | 63.3% |
| Dysuria | 8.6% | 5.6% | | |
| Palpable mass | 42.9% | 22.2% | | 47.6% |
| Tenderness | 25.7% | 38.9% | | 23.8% |
| USG with Doppler)Diagnosed Torsion | 25.7% | | 63% | 95.2% |
| Freefliud in POD | 23.8% | | 26.7% |
| Right sided | 55.7% | 50% | 70% | |
| Left | 42.9% | 38.9% | 30% |
| Bilateral | 1.4% | 11.1% | |
| Size [5-10cm ] | 71.4% | 33.3% | | |
| >10cm | 11.4% | 44.4% |
| Mature cystic teratoma | 22.8% | 16.7% | 16.7% | 28.5% |
| Mucinous cyst adenoma | 7.1% | 33.3% | 3.3% | 9.52% |
| Serous cyst adenoma | 15.7% | 16.7% | | 47.6% |
| Hemorrhagic necrosis | 30.4% | | | 9.52% |
| % Laproscopy | 81.4% | | 40% | |
| Open method | 18.6 % | 60% |
| Conservative surgery | 64.3% | 46.7% |
| Radical surgery | 45.7% | 53.3% |
| Time Interval Median | 24hrs | | 12hrs | |
| Pelvic pain | 61 | 87% |
| Epigastric pain | 4 | 5.7% |
| Diffuse abdominal pain | 2 | 2.9% |
| Asymptomatic | 2 | 2.9% |
| Nausea/ vomiting | 46 | 65.7% |
| Fever | 9 | 12.9% |
| Dysuria | 5 | 8.6% |
| Urinary retention | 1 | 1.4% |
| Constipation | 5 | 7.1 |
| Diarrhoea | 1 | 1.4% |
| Vaginal spotting | 1 | 1.4% |
| Menorrhagia | 1 | 1.4% |
CT scan of left adnexal torsion reported as haemorrhagic cyst 26x10 cm

MRI scan reported as torsion right ovary 8x 7x 6cm
Comparative Study of fallopian tube torsion
| Boukaidist et al., [22] | Our study |
|---|
| No of cases of isolated tubal torsion | 13 | 5 |
| Site of fallopian tube | Left-9 (69%) | Right-3 (66%) |
| Salpingectomy | 11 | 5 |
| Risk factors Hydrosalpinx Paraovarian cyst | 9 - | 1 4 |
| HPE-ischemic infarction | 3(50%) | 5(100%) |
Comparison of our study with other studies
| Nurith et al., [17] | Ziv Tsafrir et al., [24] | Our Study |
|---|
| Age in Years (Median) | 5-85 (38.5) | 3-16 (12) | 11-91 (25.5) |
| Premenarchal | 3(9%) | 20(90%) | 2(2.9%) |
| Postmenopausal | 10(29%) | - | 12(17%) |
| Pregnancy | - | - | 2(2.9%) |
| Asymptomatic | - | - | 2(2.9%) |
| Pain Abdomen | 35(100%) | 22(100%) | 67(95.7%) |
| Nausea/Vomiting | 16(46%) | 13(59%) | 46(65.7%) |
| Fever | 7(20%) | 2(9%) | 9(12.9%) |
| Peritoneal Signs | 12(34%) | 6(27.3%) | 18(25.7%) |
| Leukocytosis | 15(43%) | 8(36%) | 31(44%) |
| Usg–Done -Torsion Diagnosed -Mass/Enlarged Ovary | 33(94%) 9(26%) 31(91%) | 22(100%) - 8(36.3%) | 70(100%) 4(5.6%) 69(98.6%) |
| Doppler (Torsion Diagnosed/Done) | 6/11(55%) | 6/22(27%) | 14/21(66%) |
| Ctscan (Torsion Diagnosed/Done) | 12/35(35%) | 0/1 | 3/13(23%) |
| MRI (Torsion Diagnosed/Done) | - | - | 3/7(42.8%) |
| Laparoscopy Done | 10(29%) | 17(77.2%) | 57(81.4%) |
| Hemorragic Necrosis | 20(57%) | - | 21(30.4%) |
| Right Adnexa | 18(51.4%) | 15(68.2%) | 39(55.7%) |
| Size (5-10cm) | - | 5(22.7%) | 50(71.4%) |
| Ovary | 13(37%) | 18(81.8%) | 40(57.1%) |
| Ovary and Fallopian Tube | 21(60%) | - | 15(21.3%) |
| Fallopian Tube | 1(3%) | - | 5(7.1%) |
| Paraovarian/Paratubal Cyst | - | 4 | 10(14.3%) |
| Hpr (Mature Cystic Teratoma) | 8(32%) | 1(4.5%) | 16(22.8%) |
| Conservative Surgery | 11(31.5%) | 19(86.4%) | 38(54.3%) |
| Time Interval (Median) in Hours | - | 20.75 | 24 |
| Total Number of Cases | 35 | 22 | 70 |
Hemorrhagic necrosis,leukocytosis vs type of surgery
* Chi square test
| p-value* | | | Hemorrhagic necrosis [21cases] | Without hemorrhagic necrosis [48cases] |
|---|
| 0.003 | Type of surgery | CS | 5(23.8%) | 32(66.7%) |
| | RS | 16(76.2%) | 16(33.3%) |
| 0.075 | WBC<11,000 | CS | 8(20.5%) | 31(79.5%) |
| >11,000 | RS | 13(43.3%) | 17(56.7%) |
Follow of necrosed ovaries which were preserved
| | Lasobetaneorce et al., [27] | Our Study |
|---|
| 1 | Total number | 6 | 5 |
| 2 | Mean age | 8.5y(3-12) | 21.4y(11-38) |
| 3 | Average size | 5-8cm | 6.6-9.2cm |
| 4 | Site(Right) | 4 | 3 |
| 5 | Time interval between onset of symptoms to surgery | 6.5(1-15days) | 5.4(2-14d) |
Conclusion
Diagnosis of ovarian torsion is a difficult task which requires good clinical awareness. High index of clinical suspicion is the most important factor in diagnosing adnexal torsion. Ultrasound with Doppler helps in diagnosing adnexal mass with torsion. Laparoscopy is not only useful for diagnosis but also for treating torsion with less morbidity. Conservative surgery is preferred for patients in the reproductive age group.
[1]. C Hannah, Chang Shweta Vikram Pearls and Pitfalls in Diagnosis of Ovarian TorsionRadiographics 2008 28:1355-68. [Google Scholar]
[2]. Growdon Whitfield B, Laufer Marc R, Ovarian and fallopian tube torsionUptodate 2013 4:1-18. [Google Scholar]
[3]. G Oelsnar, D Shashar, Adnexal torsionClin Obst Gynecol 2006 49(3):459-63. [Google Scholar]
[4]. Longo Fauci Kasper Hauser Jameson loscalzo Fever and hyperthermiaHarrisons118th EditionTextbook of Internal Medicine:143-58. [Google Scholar]
[5]. Longo Fauci Kasper Hauser Jameson loscalzo Disorders of granulocytes and monocytesHarrisons118th EditionTextbook of Internal Medicine:472-82. [Google Scholar]
[6]. Z Tsafrir, J Hasson, L Levin, Adnexal torsion: cystectomy and ovarian fixation are equally important in preventing recurrenceEur J Obstet GynecolReprod Biol 2012 162:203 [Google Scholar]
[7]. vijayalekshmi Kandaswamy, Clinico Pathological profile of adnexal torsion cases. A retrospective analysis from a tertiary care hospitalJournal of clinical and diagnostic Research 2014 8(6):oc04-07. [Google Scholar]
[8]. LM Lo, SD Chang, SG Horng, TY Yang, CL Lee, CC Liang, Laparoscopy versus laparotomy surgical intervention of ovarian torsionJ Obstet Gynaecol Res 2008 34(6):1020-25. [Google Scholar]
[9]. K Shukunami, K Nishijima, M Orisaka, Acute abdomen in a Jehovah’s witness with chronic anaemiaAm J Emerg Med 2004 22:242 [Google Scholar]
[10]. J Hasson, Z Tsafrir, F Azem, S Baron, B Almog, R Mashiach, Comparison of adnexal torsion between pregnant and non pregnant womenAm J Obstet Gynecol 2010 202:536 [Google Scholar]
[11]. Bharathi A, Gowri Mangala, SQ Cohlan, SQ Cohlan, Torsion of the fallopian tube and the haematosalpinx in perimenopausal women –A case reportJ Clin Diagn Res 2013 7(4):731-33. [Google Scholar]
[12]. R Mashiach, N Melamed, N Gilad, Sonographic diagnosis of ovarian torsion:accuracy and predictive factorsJ Ultrasound Med. 2011 30:1205 [Google Scholar]
[13]. C Wikinson, A Sanderson, Adnexal torsion –a multi modality imaging reviewClin Radiol 2012 67:476 [Google Scholar]
[14]. Spinelli Claudio, Adnexal torsion in children and adolescents: new trends to conservative surgical approach – our experience and review of literature Gynecol Endocrinol 2013 29(1):54-58. [Google Scholar]
[15]. Vijayaraghavan SB, Sonographic whirlpool signs in ovarian torsionJournal of ultrasound in medicine 2004 23(12):1643-49. [Google Scholar]
[16]. DV Valsky, E Esh-Broder, SM Cohen, Added value of grey –scale whirlpool sign in the diagnosis of adnexal torsionUltrasound Obstet Gynecol 2010 36:630 [Google Scholar]
[17]. Hiller Nurith, Appelbaum Liat, Simonovsky Natalia, Sagi Lev, Aharoni Dvora, Sella Tamar, CT Features of Adnexal torsionAmerican Journal of Roentgenology 2007 189:124-29. [Google Scholar]
[18]. SC Oltmann, A Fischer, R Barber, R Huang, B Hicks, N Garcia, Cannot exclude torsion –a 15year reviewJ Pediatr Surg 2009 44:1212-16. [Google Scholar]
[19]. C Huchon, A Fauconnier, Adnexal torsion a literature reviewEur J Obstet Gynecol Reprod Biol 2010 150:8 [Google Scholar]
[20]. AA Shah, CE Likes, TM Price, Early polycystic ovary syndrome as a possible etiology of unexplained premenarcheal ovarian torsionJ Pediatr Adolesc Gynecol 2009 22:265 [Google Scholar]
[21]. J Schrager, G Robles, T Platz, Isolated fallopian tube torsion: a rare entity in a pre menarcheal femaleAm Surg 2012 78:118 [Google Scholar]
[22]. SA Boukaidi, J Delotte, H Steyart, JS Valla, C Saltonet, J Bouaziz, Thirteen cases of isolated tubal torsions associated with hydrosalpinx in children and adolescents, proposal for conservative management: retrospective review and literature surveyJ Pediatr Surg 2001 46(7):1425-31. [Google Scholar]
[23]. MR Said, V Bamigboye, Twisted paraovarian cyst in a young girlJ Obstet Gynaecol 2008 28:549 [Google Scholar]
[24]. Tsafrir Ziv, Azem Foad, Risk factors, symptoms, and treatment of ovarian torsion in children.The twelve year experience of one centerJournal of minimally invasive gynaecology 2012 19:29-33. [Google Scholar]
[25]. P Galinier, L Carfargna, M Delsol, Ovarian torsion. Management and ovarian prognosis: a report of 45 casesJ Pediatr Surg 2009 44:1759-65. [Google Scholar]
[26]. V Rousseau, R Massicot, AA Dwarish, Emergency management and conservative surgery of ovarian torsion in children: a report of 40 casesJ Pediatr Adolesc Gynecol 2008 21:201-06. [Google Scholar]
[27]. CE Lasso Betancor, JI Garrido Perez, Oarian torsion long term follows up of the black-bluish ovary after laparoscopic detorsion Cir Pediatr 2014 27(1):26-30. [Google Scholar]