Regaining Vision from No Perception of Light after Radiotherapy for a Case of Suprasellar Meningioma
Bhargavi Ilangovan1, Janos Stumpf2, Major Raghavan3, Rathna Devi R4, Subathira B5
1 Senior Resident, Department of Radiation Oncology, Apollo Speciality Hospitals, Chennai, India.
2 Senior Consultant, Department of Radiation Oncology, Apollo Speciality Hospitals, Chennai, India.
3 Senior Consultant, Department of Ophthalmology, Apollo Speciality Hospitals, Chennai, India.
4 Senior Consultant, Department of Radiation Oncology, Apollo Speciality Hospitals, Chennai, India.
5 Senior Consultant, Department of Radiation Oncology, Apollo Speciality Hospitals, Chennai, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Bhargavi Ilangovan, 64 G, SR Dream Bungalow, Gowri Nagar, Mugalivakkam, Chennai-125, India. Phone : 9840770910, E-mail : bhargavi.ilangovan@gmail.com
Meningiomas are tumours of the arachnoid cap cells. Usually they are referred to according to their location. They are primarily treated with surgery. They tend to recur following surgery. Suprasellar meningiomas frequently present with visual disturbances. Our patient is a case of recurrent suprasellar meningioma. The visual acuity in one eye was No Perception of Light(NPL). From NPL, the visual acuity improved to 6/12 in six months after High Precision Irradiation (HPI). This case emphasizes the importance and the need for aggressive management. It also shows the use of radiotherapy techniques used in synergy to produce the necessary results.
Radiotherapy, Suprasellar meningioma, Visual acuity
Case Report
A 55-year-old patient presented to the Department of Radiation Oncology, Apollo Speciality Hospitals, Chennai, India, with the complaints of diminution of vision of about two months duration. It was gradually worsening over time. On evaluation, she was found to have No Perception of Light (NPL) in the left eye, the right eye being normal. Her visual acuity and field of vision were evaluated by our neuroophthalmologist. Her left eye had no perception of light (NPL). Perimetry showed marginal scotoma in the upper temporal quadrant of the right eye.MRI brain showed a tumor in the sellar and suprasellar region with compression of the optic chiasm [Table/Fig-1].
Showing the recurrent lesion before IMRT. Volume of tumor

She had similar complaints of gradual deterioration of vision for over 18 months. She was evaluated at Bangladesh (her native place ) for the complaints. An MRI of the brain was done which showed a mass in the sellar, supra and para sellar regions compressing upon the optic chiasm suggestive of meningioma. She had gross total removal of the tumor. Histopathology reported a transitional meningioma.The patient had improvement of vision, though for a short period of time only. After about six months, she developed deterioration of vision on the left eye for which she came to our hospital.
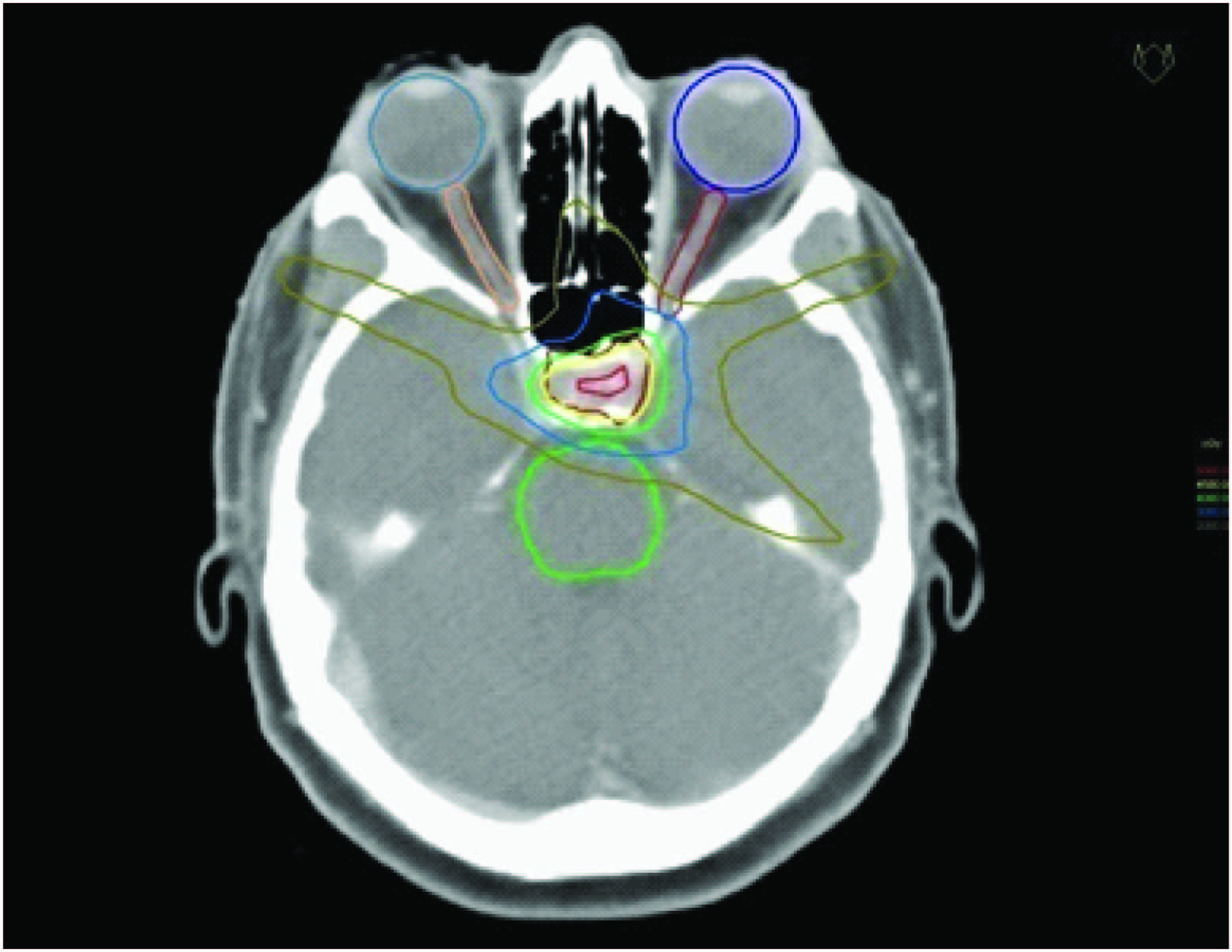
We decided to irradiate the lesion as the patient was reluctant for another surgery. She was irradiated with a combination of IMRT and Radio Surgery boost. The recurrent tumor was irradiated with a small margin, by IMRT (Intensity Modulated radiotherapy) technique [Table/Fig-2&3]. Care was taken to minimize the dose to the optic apparatus. This was achieved by detailed contouring of the optic nerves and optic chiasm. Very strict constraints were prescribed for these normal structures. Plan was evaluated and it was made sure that these constraints were adequately met with. There was response by the end of the five week treatment using conventional fractionation. The remaining volume was given a boost dose using fractionated radio surgery technique. She received a total dose of 45 Gy in 25 fractions by IMRT technique over a period of five weeks, followed by a boost dose of 10.5 Gy in 3 fractions, one fraction per day, prescribed to the 85% isodose line covering the lesion by fractionated radio surgery technique [Table/Fig-4]. The nominal total dose was 55 Gy, the radiobiological equivalent being around to 60 Gy.
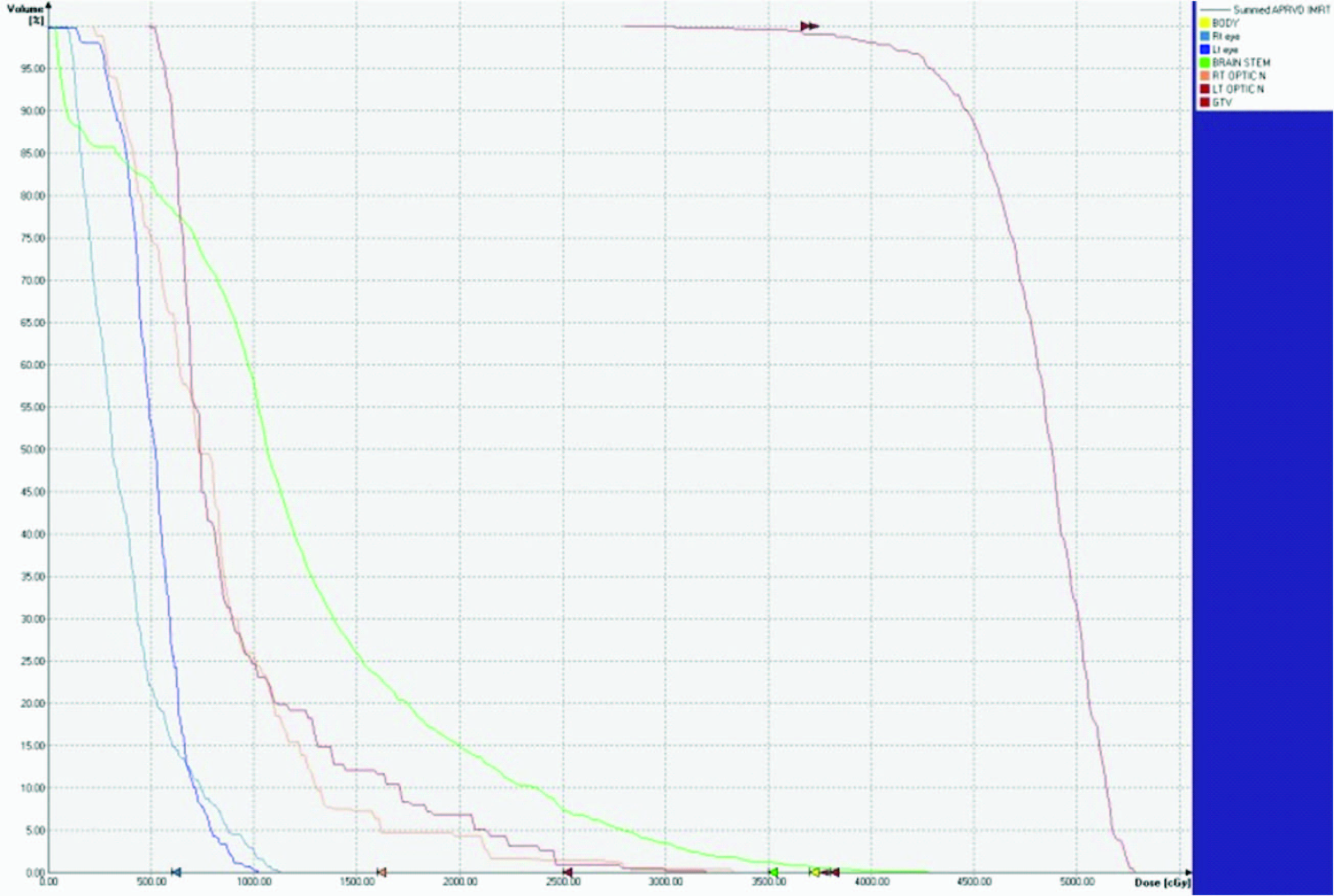

She was evaluated in one month and again in six months. There was a considerable reduction in tumor volume (about 50 percent) with return of vision [Table/Fig-5].
The follow up volume analysis

The vision in the left eye improved from no perception of light to 6/12. She was also able to identify colors and the near vision was N6. Perimetry could be recorded. [Table/Fig-6] shows its dynamism.
Showing the visual evaluation before and after radiotherapy
| Right eye | Left eye |
|---|
| 16/4/12 | 25/5/12 | 6/11/12 | 16/4/12 | 25/5/12 | 6/11/12 |
|---|
| Visual acuity | 6/6 | 6/6 | 6/6 | NPL | 6/36 | 6/12 |
| Near vision | N6 | N6 | N6 | NPL | N24 | N6 |
| Colour vision | Normal | Normal | Normal | NPL | Could not recognise primary colours | 6/20 by ishihara |
| perimetry | Marginal scotoma in the upper temporal quadrant | Marginal scotoma has improved. Enlarged blind spot normal. | | Could not be recorded | Could not be recorded | Recorded. Loss of nasal field by confrontation method. |
Discussion
Meningiomas account for approximately 30% of primary intracranial tumours and are the most common benign intracranial tumours in adults [1]. They are classified by their sites of origin [2]. The WHO classification system subdivides meningioma into 11 histological subtypes , the predominant ones being meningothelial, fibrous and transitional.
Suprasellar meningioma usually arises from the tuberculum sellae or the sulcus chiasmatis. Due to the close proximity to the optic apparatus, the same may be involved even when the lesions are small. In case of pressure on the chiasm, bitemporal filed defects may occur, while in prechiasmal involvement, vision in one eye may be more seriously involved than the other [3].
The definitive treatment of meningioma is surgery. Incompletely resected, recurrent or malignant meningiomas require radiotherapy [4]. Postoperative external beam radiotherapy was seen to increase the median time to progression [5]. A dose of 50 to 54 Gy in 180 cGy per fraction is advised for the lesion [6]. Radio surgery is gaining importance due to its precision and normal tissue preservation [7]. Impressive progress in radiotherapy has resulted in comparable geometrical and geographical precision in the delivery of radiation. It is the size and location of a benign CNS lesion, that drives the dose prescription.
In our case it was decided to irradiate owing to the patient’s reluctance for another surgery. The speed with which this tumor has recurred was pointed out. Irradiation is believed to have a long control or arrest of growth as per the general understanding and our experience. When the question of optimum dose arose, it was meaningful to offer a relatively high dose as the disease was recurrent. But the damage to the optic apparatus and the fact that the patient had only one good eye was a hindrance. She was treated with the high precision techniques. We used a combination of IMRT and cyber knife radio surgery. With IMRT we delivered the dose of 45 Gy in conventional fractionation to the large recurrent lesion, thereby the tolerance of the nearby structures was respected. The volume that was remnant after this dose was irradiated with Radio surgery. A dose of 10.5 Gy was delivered in 3 fractions. A biological equivalent of about 60 Gy was thus delivered. The neighboring structures could thus be spared more effectively due to the addition of radiosurgery as a boost. Any dose more than the tolerance dose could have been detrimental to the right eye.
The response to the treatment in terms of the volume reduction was dramatic and so was the visual improvement. From NPL, there was good vision detected during follow up. Vision lost due to chronic causes seldom improves [8]. There have been reports of visual improvement from NPL, but all in acute causes. There have been analyses of visual improvement post radiotherapy, but they did not start with a NPL [9]. The literature shows assessment of vision in cases of sellar and suprasellar meningiomas, before and after radiotherapy. The above cited study too evaluates the visual outcome after stereotactic radiotherapy. The eyes with no visual acuity were not reported to have an improvement. It is common to have an improvement in the visual acuity in the eye with residual vision, but not from NPL. The combination of conventionally fractionated radiotherapy with a boost with hypofractionated radiosurgery has perhaps worked in our favour. Likewise, the combination of high precision techniques is also not much documented in the literature. It is understood that the response of meningiomas to irradiation may be slow. Therefore surgical decompression may represent a better choice for the recovery of vision.
Our patient has shown unexpected recovery from NPL, probably due to multifactorial circumstances. Tumor has shown a quick response to radiation. Even a marginal shrink might have given a chance for the recovery of the optic apparatus. High precision irradiation has exposed the pathology, saving the sensitive optic apparatus. Combination of conventional Radiotherapy with Radiosurgery might have sped up tumor response without oedema in the region.
Conclusion
Suprasellar meningioma can be detected early because of the visual disturbances due to its proximity to the visual apparatus. Hence aggressive management in the form of surgery and/or radiotherapy, can preserve the remaining vision and can occasionally cause a significant improvement. In our case, the patient had a dramatic improvement after irradiation. This article reinstates the fact that radiotherapy with high precision is warranted in these settings. The restriction to the delivery of the required dose due to normal tissue constraints is overcome by the use of combination of high precision techniques which has been beneficial.
[1]. Cushing H, The meningiomas (dural endotheliomas): their source, and favoured seats of origin. (Cavendish Lecture)Brain 1922 (45):282-316. [Google Scholar]
[2]. Edward C, Halperin MD, Carlos A, Perez MD, Luther W, Brady MD, Perez and Brady’s principle and practice of radiation oncologychapter 32 [Google Scholar]
[3]. Sen-Li Jen, Liang-Shong Lee, Suprasellar meningiomas: analysis of 32 casesChin Med J (Taipei) 1997 159:7-14. [Google Scholar]
[4]. Forbes AR, Goldberg ID, Radiation therapy in the treatment of meningioma: the joint center for radiation therapy experience 1970 to 1982J Clin Oncol 1984 2(10):1139 [Google Scholar]
[5]. Goldsmith BJ, Wara WM, Wilson CB, Larson DA, Postoperative irradiation for subtotally resected meningiomas: a retrospective analysis of 140 patients treated from 1967 to 1990J Neurosurg 1994 80(2):195 [Google Scholar]
[6]. Milker-Zabel S, Zabel-du Bois A, Huber P, Schlegel W, Debus J, Intensity-modulated radiotherapy for complex-shaped meningioma of the skull base: long-term experience of a single institutionInt J Radiat Oncol Biol Phys 2007 68(3):858 [Google Scholar]
[7]. Hakim R, Alexander E 3rd, Loeffler JS, Shrieve DC, Wen P, Fallon MP, Results of linear accelerator-based radiosurgery for intracranial meningiomasNeurosurgery 1998 42(3):446 [Google Scholar]
[8]. Seol HJ, Park HY, Nam DH, Kong DS, Lee JI, Kim JH, Park Clinical outcomes of tuberculum sellar meningioma focusing on reversibility of post operative visual functionActa Neurochie (Kien) 2013 155(1):25-31. [Google Scholar]
[9]. Liu JK, Iormans Hershewe GL, Moorthy CR, Benzil DD, Loptic nerve sheath meningioma: visual improvement after stereotactic radiotherapyNeurosurgery 2002 50(5):950-55.Discussions 955-957 [Google Scholar]