Thoracic Part of Sympathetic Chain and its Branching Pattern Variations in South Indian Cadavers
Hemanth Kommuru1, Swayam Jothi2, P Bapuji3, Lekha Sree D4, Jacintha Antony5
1 Tutor, Department of Anatomy, SSSMC & RI, Ammapettai, Tiruporur, Gudvancherry Main Road, Nellikuppam, Kancheepurm, Tamil Nadu, India.
2 Professor & Head, Department of Anatomy, SSSMC & RI, Ammapettai, Tiruporur, Gudvancherry Main Road, Nellikuppam, Kancheepurm, Tamil Nadu, India.
3 Professor & Head, Department of Anatomy, ASRAM, Eluru Andhra Pradesh, India.
4 PG Student, Department of Anatomy, Guntur Medical College, Guntur, India.
5 Professor & Head, Department of Anatomy, Sri Balaji Medical College, Chennai, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Hemanth Kommuru, Tutor, Department of Anatomy SSSMC & RI, Ammapettai, Department of Anatomy, Tiruporur, Gudvancherry Main Road, Nellikuppam-603108 Kancheepurm, Tamil Nadu, India. Phone : 9884583539, E-mail : hemanth.kommuri@gmail.com
Introduction: The sympathetic trunks are two ganglionated nerve trunks that extend the whole length of the vertebral column.The two trunks end by joining together to form a single ganglion, the ganglion impar. The thoracic part of the sympathetic chain runs downward and leaves the thorax behind the medial arcuate ligament. The preganglionic fibers which are grouped together to forms planchnic nerves and supply the abdominal viscera. Anatomical variations of the thoracic sympathetic trunk in relation to intercostal nerves may be one of the reasons that cause surgical failures. Therefore, our present study aimed to investigate the sympathetic variations in the cadavers.
Materials and Methods: In the present study we have investigated 31 embalmed cadavers thoracic cavities were eviscerated, the posterior thoracic walls were dissected carefully to expose the sympathetic chain and its branches.
Results: Stellate ganglion was observed bilaterally in 4 cadavers and unilaterally in 15 cadavers. Greater splanchnic nerve highest origin was 4th ganglion and the lowest origin was 11th ganglion. Common origin for the lesser splanchnic nerve was from the 11th ganglion. Common origin for the least splanchnic nerves was from the 12th ganglion.
Conclusion: Information on the variability of the anatomy of the thoracic sympathetic chain and splanchnic nerves may be important for the success of subdiaphragmatic neuroablative surgical approaches to pain control and splanchnic neurectomy for the management of chronic abdominal pain.
Ganglia, Rami communicantes, Splanchnic nerves, Sympathetic chain
Introduction
The sympathetic trunks are two ganglionated nerve trunks that extend the whole length of the vertebral column. In the neck, each trunk has 3 ganglia; in the thorax, 11 or 12; in the lumbar region, 4 or 5; and in the pelvis, 4 or 5. In the neck, the trunks lie anterior to the transverse processes of the cervical vertebrae; in the thorax, they are anterior to the heads of the ribs or lie on the sides of the vertebral bodies; in the abdomen, they are anterolateral to the sides of the bodies of the lumbar vertebrae; and in the pelvis, they are anterior to the sacrum [1]. Below, the two trunks end by joining together to form a single ganglion, the ganglion impar. The ganglia are joined to spinal nerves by short connecting nerves called white and grey rami communicantes. Preganglioic axons are coming from the lateral grey column (horn) of the spinal cord. The myelinated axons of these cells leave the cord and join the paravertebral ganglia of the sympathetic trunk through the white rami communicantes while postganglionic axons leave the trunk through the grey rami communicantes. The axons of postganglionic neurons are non- myelinated and distributed to target organs in various ways. The principal neurotransmitter released by postganglionic sympathetic neurons is noradrenaline. Sympathetic fibers cause constriction of the blood vessels supplied to the skin and GIT and dilatation of the blood vessels supplied to the skeletal muscle, brain and to the heart. Postganglionic sympathetic fibers are secretomotor to the sweat glands. In the viscera, they cause general vasoconstriction, bronchial and bronchiolar dilatation. They also enhance glandular secretions and inhibit the alimentary muscle contraction. The term stellate ganglion refers to fusion of the inferior cervical sympathetic ganglion with the first thoracic ganglion and the stellate ganglion is present in 80% of the population [2]. The stellate ganglion is located at the level of seventh cervical vertebrae (C7) anterior to the transverse process of C7, superior to the neck of the first rib, and just below the subclavian artery. The thoracic part of the sympathetic chain runs downward on head of ribs and leaves the thorax on the side of the body of the 12th thoracic vertebra behind the medial arcuate ligament. The thoracic part of the sympathetic chain has rami communicantes, postganglionic fibers to the heart, aorta, lungs and oesophagus. The preganglionic fibers which are grouped together to form splanchnic nerves (greater, lesser and least) and supply the abdominal viscera [3]. Anatomical variations of the thoracic sympathetic trunk in relation to intercostals nerves may be one of the reasons that cause surgical failures. Therefore our present study is attempted to investigate the incidence of variations in the thoracic part of the sympathetic chain in the cadavers in our anatomy department [Table/Fig-1].
Objectives
To find out variations in the number of ganglia in the thoracic part of the sympathetic chain.
To observe the variations in the formation of splanchnic nerves in the thoracic part of the sympathetic chain.
To find out variations in rami communicantes in the thoracic part of the sympathetic chain.
To observe variations in the visceral branches of thoracic part of the sympathetic chain.
Materials and Methods
In the present study we have investigated 31 embalmed cadavers which were dissected bilaterally. Out of 31, 19 cadavers were male and the remaining 12 were female. The thoracic cavity was eviscerated via an anterior approach and the posterior thoracic wall was exposed. Care was taken while stripping the parietal pleura to expose the sympathetic chain and its branches.
Observations
Ganglia of the chain
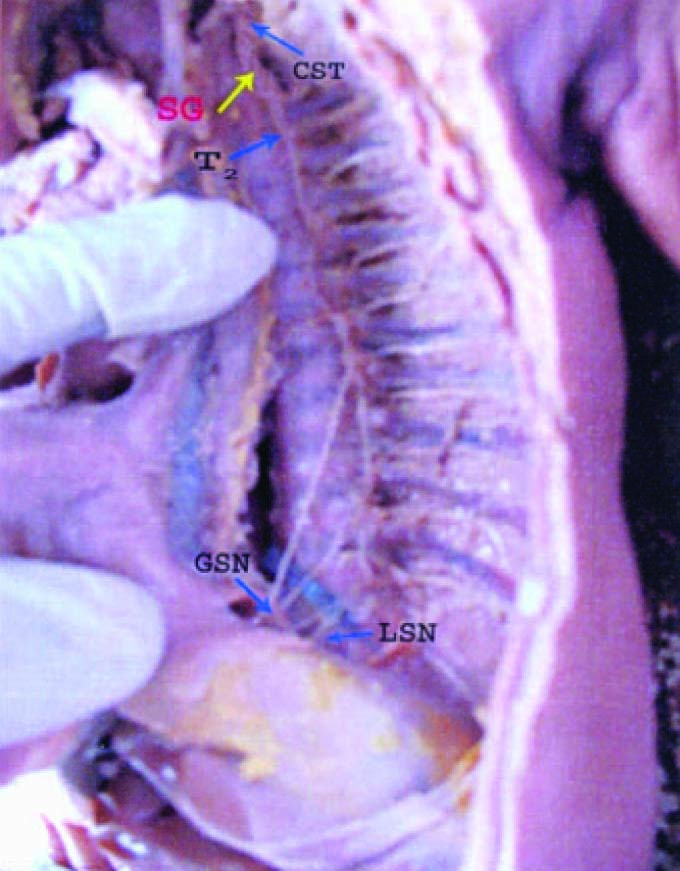
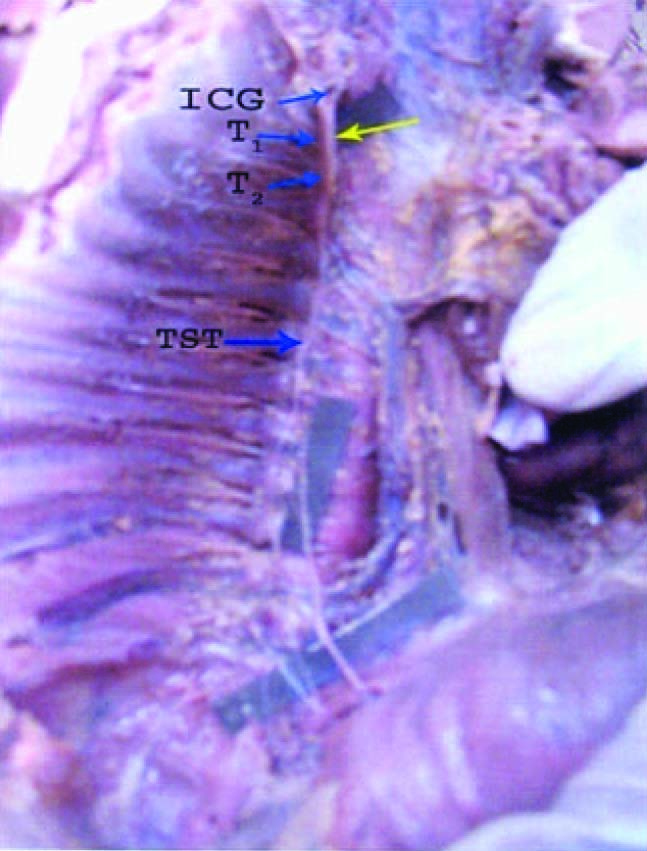
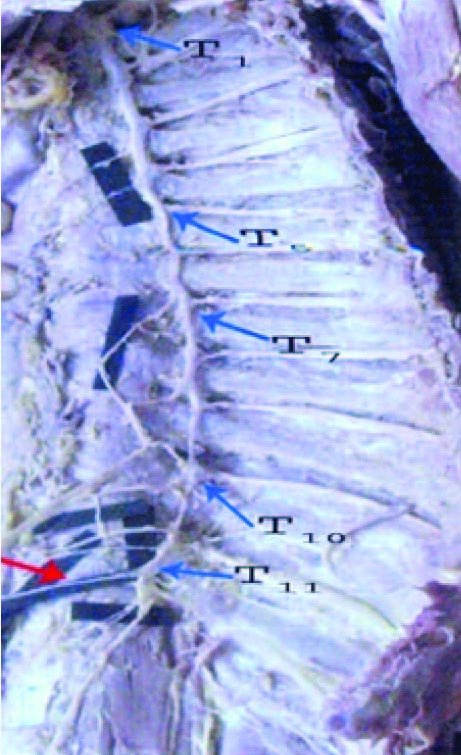
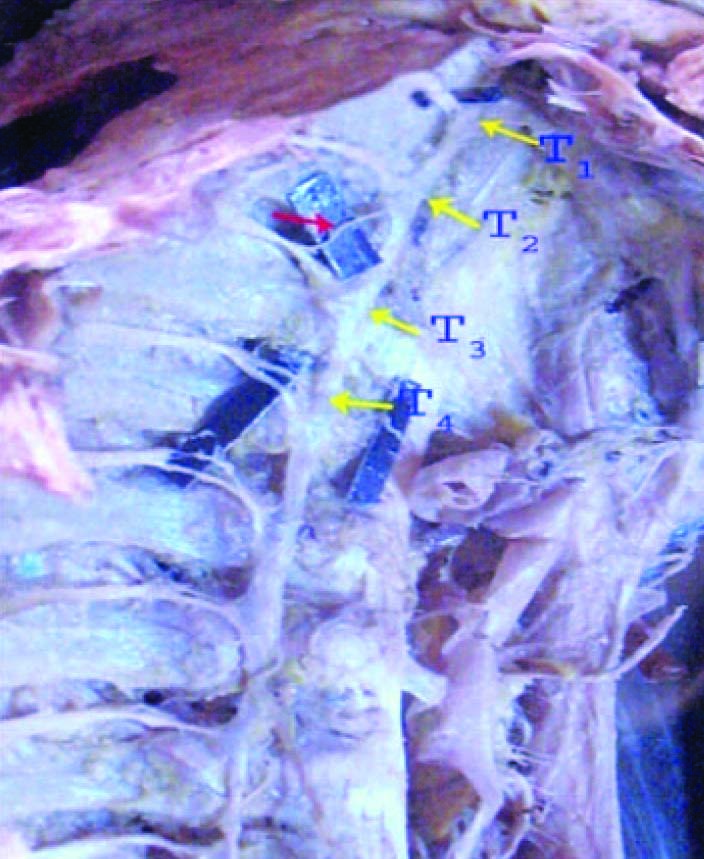
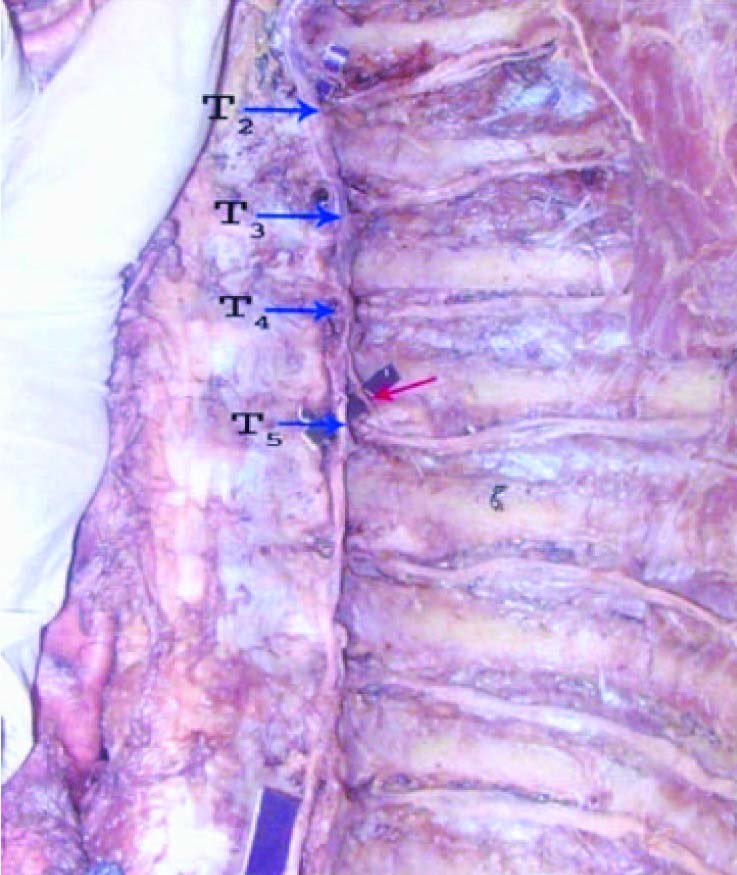
Stellate ganglion was present bilaterally in 4 cadavers and unilaterally in 15 cadavers [Table/Fig-2] One cadaver showed the fusion of inferior cervical ganglion with first and second thoracic ganglion on the right side [Table/Fig-3] in eleven cadavers 11 ganglia were present bilaterally [Table/Fig-4].
Various percentages of splanchnic nerve formations were tabulated
| Splanchnic nerves | Origin from ganglia | Percentage |
|---|
| Greater splanchnic nerve | 7,8,9th ganglia | 37% |
| 8,9,10th ganglia | 31% |
| 6,7,8,9th ganglia | 21% |
| 4,5,6,7,8,9th ganglia | 1.6% |
| 8,9,10,11th ganglia | 1.6% |
| Lesser splanchnic nerve | 10, 11th ganglia | 63% |
| 9,10,11th ganglia | 21% |
| 10th ganglion | 6% |
| 8,9,10,11th ganglia | 5% |
| 11th ganglion | 5% |
| Least splanchnic nerve | 11th ganglion | 70.83% |
| 12th ganglion | 29.17% |
Stellate ganglia on the left side SG- Stellate ganglion ,CST- cervical sympathetic trunk,T2- second thoracic ganglion on the left side, GSN –Greater splanchnic nerve ,LSN-Lesser splanchnic.,
Fusion of inferior cervical with 1st & 2nd thoracic sympathetic ganglia on the right side ICG- Inferior cervical ganglion T1,T2 –thoracic sympathetic ganglion.,
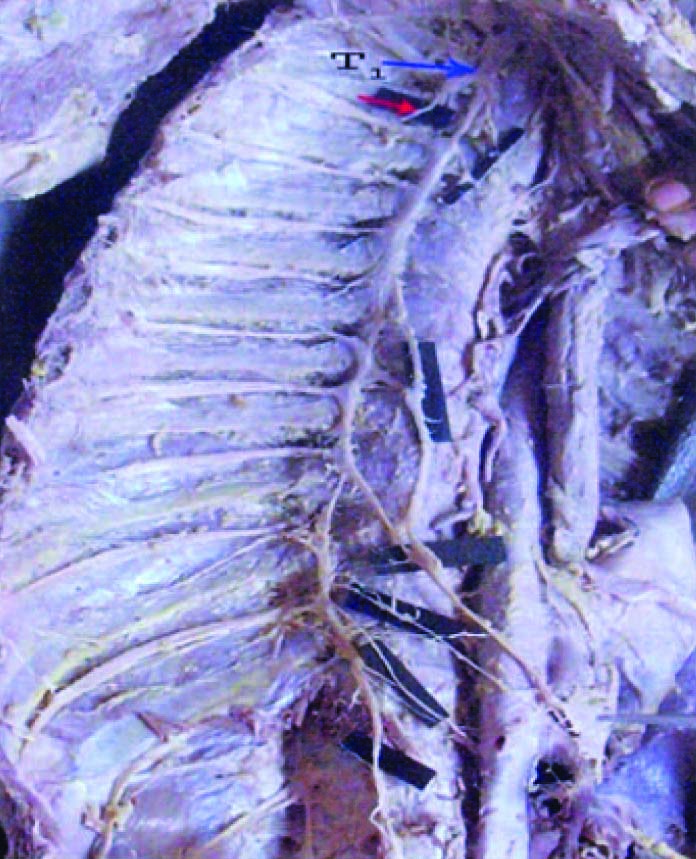
Normal pattern of the thoracic sympathetic chain with eleven thoracic sympathetic ganglia on the left side of the cadaver T1,T5,T7,T10,T11–Thoracic sympathetic ganglia
Splanchnic nerves
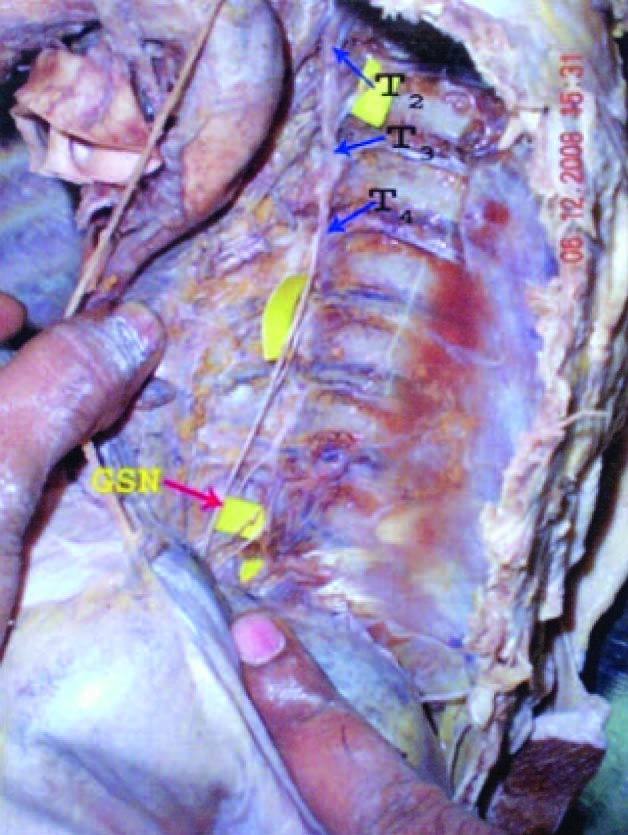
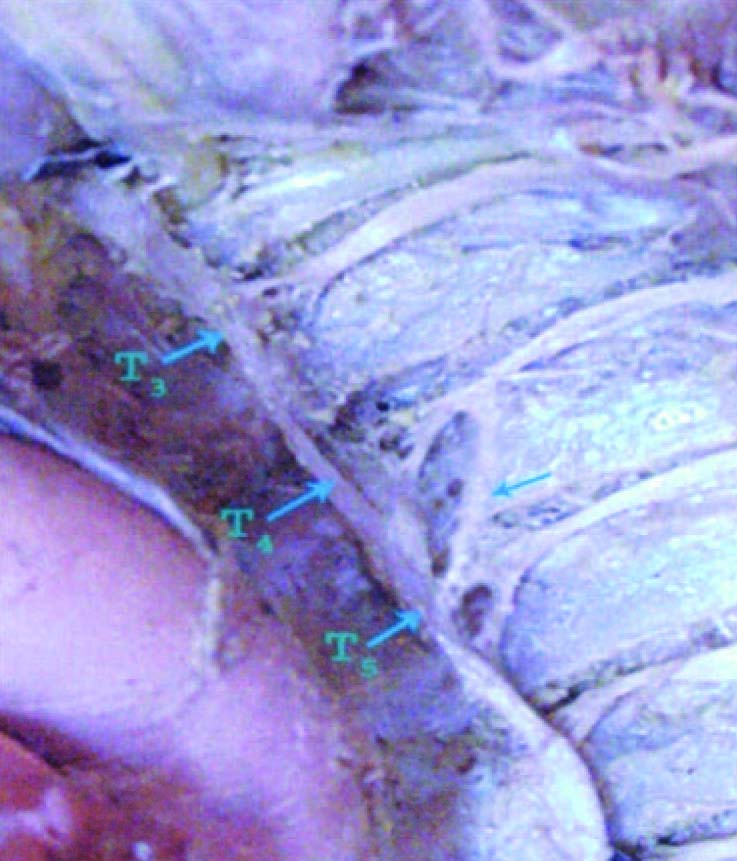
The highest origin of the greater splanchnic nerve from the fourth thoracic ganglion was observed in one cadaver on the right side [Table/Fig-5], the lowest origin of greater splanchnic nerve from the eleventh ganglion was seen in one cadaver on the left side [Table/Fig-6] and the origin of the greater splanchnic nerve was bilaterally symmetrical in 3 cadavers only. The number of ganglia involved varied from 2-6. The GSN was arising from 7, 8, & 9 ganglia in 37% of cases [Table/Fig-7]. In the present study intermediate splanchnic ganglion was found in 13 of 62 sides (21%) and observed only on the GSN [Table/Fig-8]. Lesser splanchnic nerve was bilaterally symmetrical in 12 cadavers and it was originating from 10th to 11th ganglia in 63.7% of specimens [Table/Fig-9]. Least splanchnic nerve was absent bilaterally in 12 cadavers and unilaterally in 14 cadavers. It was originating from 11th Ganglion in 27% 0f cases [Table/Fig-10] and from the 12th ganglion in 11% of cases.
Highest Origin of greater splanchnicnerve from 4th ganglion on the leftside, GSN- Greater splanchnic nerve
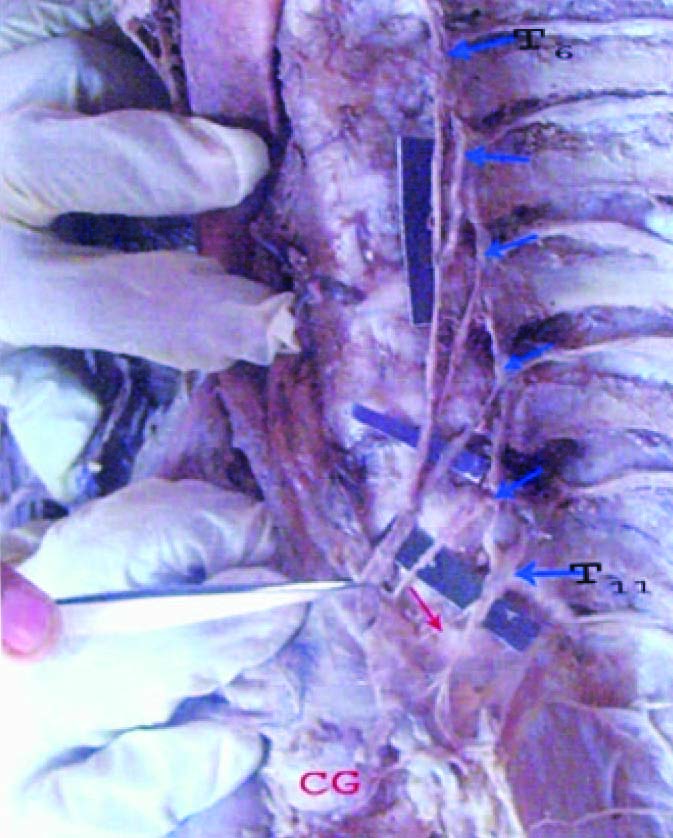
Lowest Origin of greater splanchnic nerve from 11th ganglion GSN- Greater splanchnic nerve, T11-11th thoracic ganglia on the left side of the cadaver. CG- Coeliac ganglion
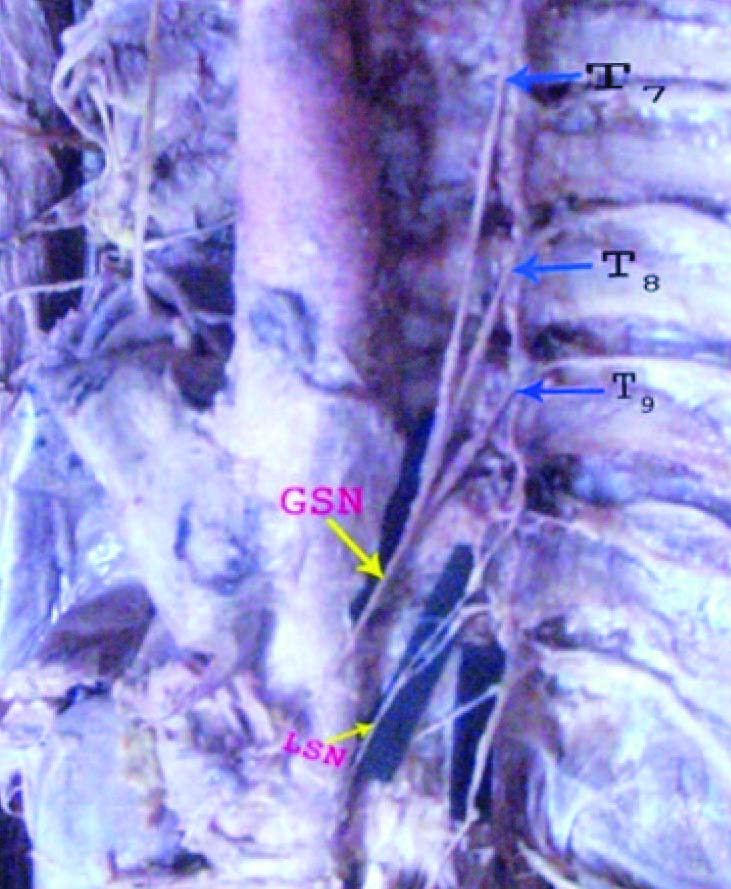
Common origin of greater splanchnic nerve from 7th ,8th & 9th ganglion GSN- Greater splanchnic nerve,T7,8,9 - thoracic ganglia on the left side of the cadaver. LSN- Lesser splanchnic nerve
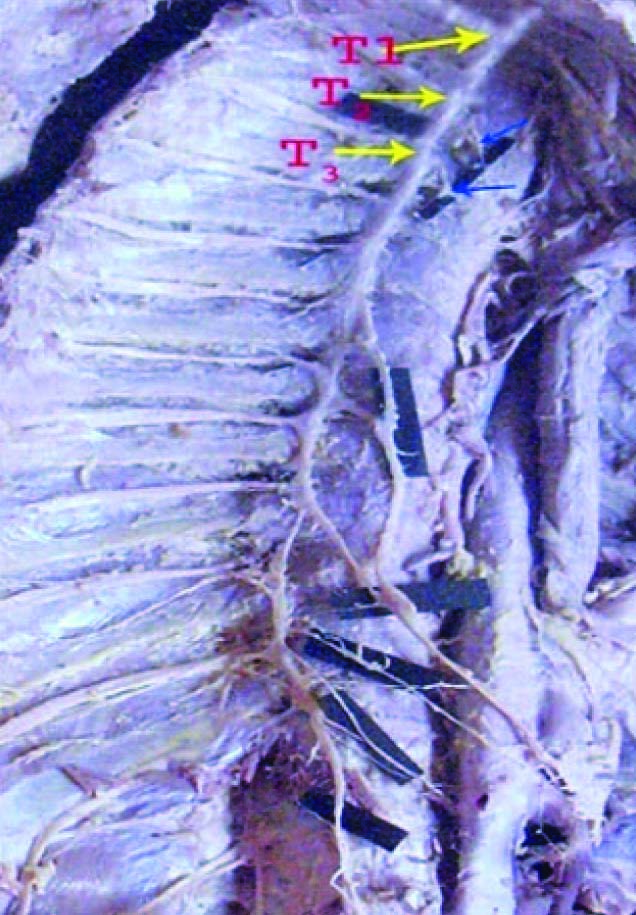
Presence of intermediate splanchnic ganglion (block arrows) on the greater splanchnic nerve on the right side of the cadaver: T1,T2,T3 are thoracic sympathetic ganglia

Common origin of Lesser splanchnic nerve from 10th & 11th Ganglia on the left side of the cadaver GSN- Greater splanchnic nerve, LSN- Lesser splanchnic nerve, CG- Celiac ganglion, ARP- Aortico renal plexus
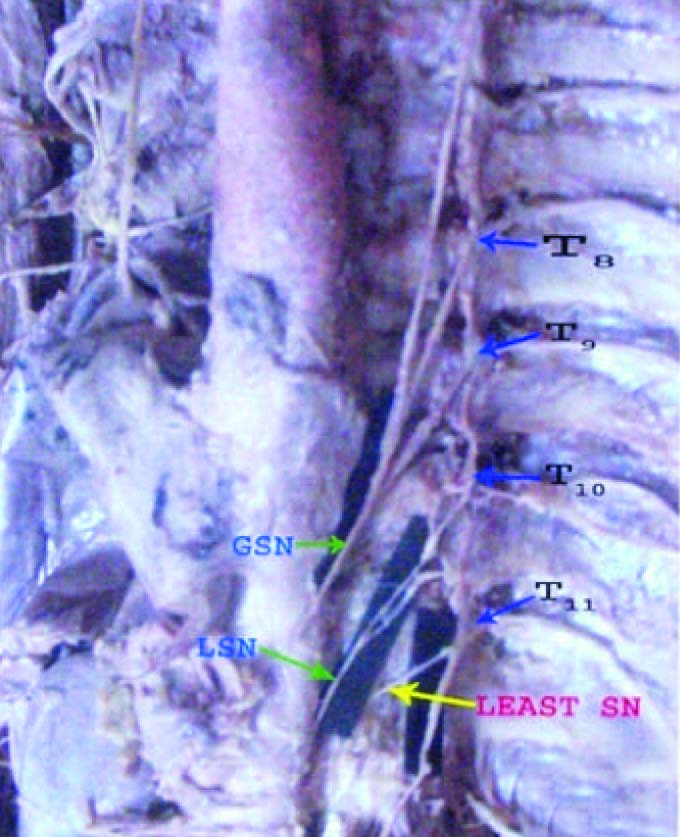
Common Origin of Least splanchnic nerve (SN) from 11th Ganglia on the left side. GSN-Greater splanchnic nerve, LSN- Lesser splanchnic nerve
Rami communicantes
Each sympathetic ganglion was found to be connected by a white rami communicantes and grey rami communicantes with the corresponding spinal nerve.
In addition, the following were observed.
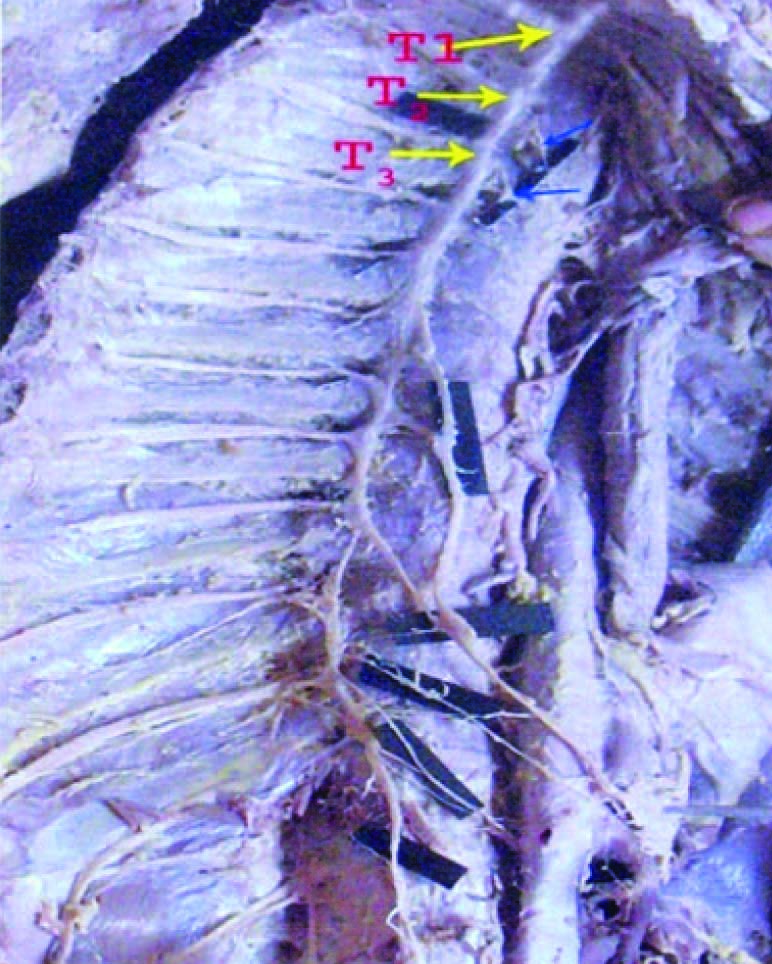
In one cadaver first thoracic ganglion was connected to second intercostals nerve on the right side [Table/Fig-11].
Another cadaver showed the second thoracic ganglion connected to the third intercostals nerve on the right side [Table/Fig-12].
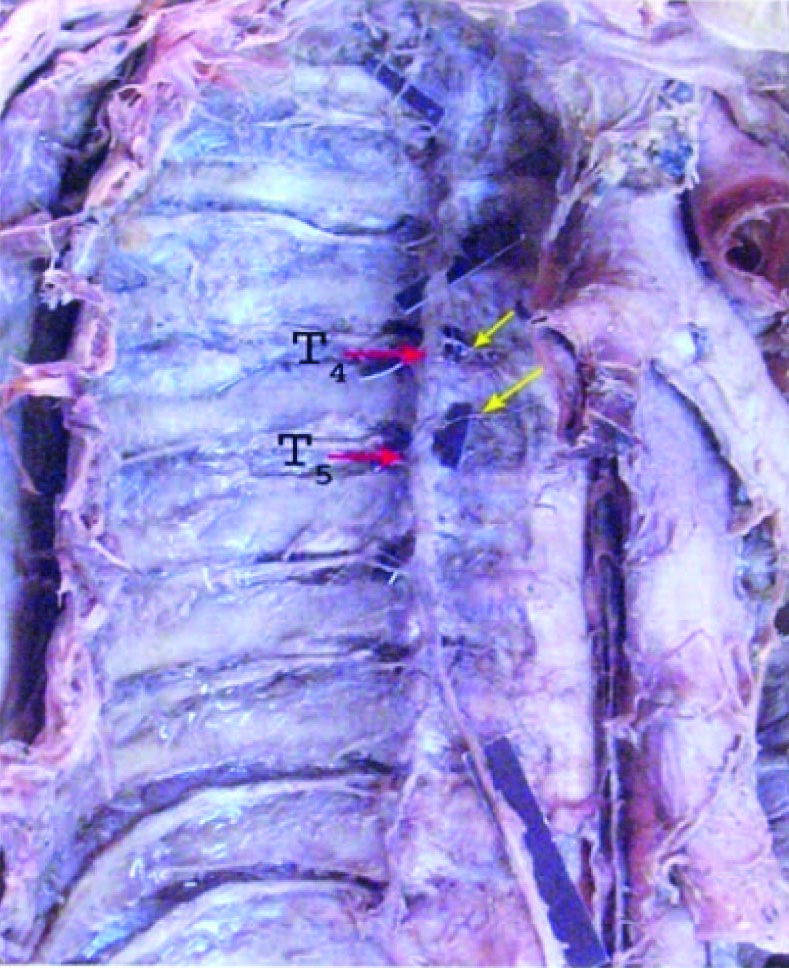
In another cadaver the fourth thoracic ganglion was connected to the third intercostal nerve on the left side [Table/Fig-13].
In another cadaver on the left side an ascending ramus was seen connecting the fifth thoracic ganglion to the fourth intercostals nerve [Table/Fig-14].
Ramus communicantes (red arrow) connecting 1st thoracic ganglion & 2nd Intercostal nerve (Right side). T1 –First thoracic ganglia.,
Ramus communicantes (red arrow) connecting 2nd thoracic ganglion & 3rd Intercostal nerve (Right side).T2 –Second thoracic ganglia,
Ramus communicantes (red arrow) connecting 4ththoracic ganglion & 5th Intercostal nerve.T4 –Fourth thoracic ganglia, T5- Fifth thoracic ganglion on the left side.
Ramus communicantes (arrow) connecting 5th thoracic ganglion & 4th Intercostal nerve on the left side. (T5 –Fifth thoracic ganglion
Medial visceral branches
Other medial visceral branches were coming from the upper five thoracic ganglia and supplyingthe thoracic viscera like heart, aorta, lungs and esophagus etc. [Table/Fig-15,16].
Medial branches (blue arrows) from 2nd & 3rd thoracic ganglia (Right side).T1,2,3- Thoracic sympathetic ganglia
Medial branches from 4th & 5th thoracic ganglia (Right side).T4,5- Thoracic sympathetic ganglia
Discussion
The inferior cervical ganglion fused with the first thoracic ganglion the Stellate ganglion will be formed and extended downwards to the level of disc between the first and second thoracic vertebra and when second was also fused the mass extended to the lower border of second thoracic vertebra [4]. Out of 25 dissections he observed the inferior cervical sympathetic ganglion independent in five incidences, fused with first thoracic ganglion in 17 cases, fused with first and second thoracic in three cases. In the present study out of 31 dissections, stellate ganglion was found in 19 cases and fused with first and second thoracic ganglion in one case and independent in 11 cases. Irregularity in the number of ganglia along the sympathetic chain is a familiar observation. Anatomical texts refer to ‘ten or eleven’ thoracic ganglia, there were 11th ganglia in seven cases out of 25 cases and in other four cases there was small accessory ganglion connected only with the twelfth or subcostal nerve [4]. In the present study in 11 cases 11 ganglia were present bilaterally; an accessory ganglion connecting with the subcostal nerve was present in three cadavers bilaterally and in one cadaver unilaterally. The origin of splanchnic nerves differs considerably with respect to their number, the level at which the thoracic ganglia gives off their fibers to the individual thoracic splanchnic nerves, the presence of the lesser and least nerves and accessory nerve fibers [5–8]. There were three splanchnic nerves of the thoracic sympathetic trunk; arising from the lower eight ganglia. The greater splanchnic nerve (GSN) is formed by branches of the 5th to 9th thoracic sympathetic ganglia, the lesser splanchnic nerve (LSN) from 10th to 11th thoracic sympathetic ganglia and the least splanchnic nerve from the 12th thoracic ganglion. Splanchnic nerves contain predominantly visceral efferent fibers and pain conducting visceral afferent fibers [9]. The highest contribution of the sympathetic chain to the GSN is coming from the T4 and T5 ganglia [10–12]. The lowest sympathetic ganglion contribution for the GSN is coming from the T12 ganglion [13]. In the present study the highest origin of the greater splanchnic nerve was T4 ganglion and the lowest origin from T11 ganglion. The greater splanchnic nerve conforming to the so- called normal pattern in only 23% and rarely bilaterally symmetrical [5]. In the present study the common origin was found in 37% of specimens and bilaterally symmetrical in three cadavers. The range of origin of the lesser splanchnic nerve to be from 9th to 12th ganglions and most common type was coming from the 10th and 11th ganglia [11]. The least splanchnic nerve was originating from 10th and 11th ganglions 27.5% cases [5] but in the present study common origin of the nerve was 10th and 11th ganglions and formed 63.7% of specimens. According to some authors the highest origin of LSN was 7th ganglion [5]. But in the present study highest origin for the lesser splanchnic nerve was coming from the 9th ganglion. Least splanchnic nerve was arising from the 12th ganglion in 57% of cases [11]. In the present study the common origin was from the 11th ganglion in 17 specimens (27%) and from the 12th ganglion in 7 specimens (11%). Some authors observed in his findings the intermediate splanchnic ganglia (ISG) was observed only on the GSN main trunk with an incidence of 6 out of 10 sides (60%) in the adult cadavers and 11 of 28 sides (39%) in the fetuses [7]. In the present study intermediate splanchnic ganglion was observed in 13 of 62 (21%) sides in adult cadavers on the GSN. The grey rami of the upper thoracic ganglia split into two bundles, the larger bundle joining the corresponding nerve while the smaller ascends behind the neck of the rib above and join the next higher nerve [14]. In the present study sympathetic ganglion was found to be connected by a white ramus and a grey ramus with the corresponding spinal nerve. In one cadaver first thoracic ganglion was connected to second intercostal nerve on the right side, another cadaver showed the second thoracic ganglion connected to the third intercostal nerve on the right side, in another cadaver the fourth thoracic ganglion was connected to the third intercostal costal nerve on the right side and in another cadaver on the left side an ascending ramus was seen connecting the fifth thoracic ganglion to the fourth intercostals nerve.
A variable number of thoracic splanchnic branches leave the chain, especially in the upper part of the thorax to join the cardiac and pulmonary plexus; others join the aortic plexus and are distributed through them. The thoracic cardiac branches contain about twice as many fibres as that reach the cardiac plexus by the larger cervical sympathetic cardiac branches [15]. In the present study medial visceral branches coming from the upper thoracic ganglia were involvedin the formation of cardiac plexus, pulmonary plexus and supplying the heart, esophagus, lungs.
Information on the variability of the anatomy of the thoracic sympathetic chain and splanchnic nerves may be important for the success of subdiaphragmatic neuroablative surgical approaches to pain control and splanchnic neurectomy for the management of chronic abdominal pain [16].
Conclusion
In the present study the variations in the thoracic sympathetic chain and the formation of splanchnic neural pattern were identified. Inconsistent results of splanchnectomies may be due to anatomical variations in the formation of splanchnic nerves, So it is essential to know the details, pattern, and variations of the sympathetic chain and origin of splanchnic nerves for sympathectomy and splanchnectomy.
[1]. Cunningham DJ, Notes on the great splanchnic ganglionJournal of Anatomy 1875 9:303-05. [Google Scholar]
[2]. Elias M, Cervical sympathetic and stellate ganglion blocksPain Physician 2000 3(3):294-304. [Google Scholar]
[3]. Gest TR, Hildebrandt S, The pattern of the thoracic splanchnic nerves as they pass through the diaphragmClin Anat 2009 22(7):809-14. [Google Scholar]
[4]. Pick J, Sheehan D, Sympathetic rami in manJ. Anat 1946 80(Pt1):12-20.3. [Google Scholar]
[5]. Edwards L, Fand Baker RC, Variations in the formation of the splanchnic nerves in manA Nat.Rec 1940 77:335-42. [Google Scholar]
[6]. Jit I, Mukerjee RN, Observations on the anatomy of the human thoracic sympathetic chain and its branches; with an anatomical assessment of operations for hypertensionJ AnatSoc India 1960 9:55-82. [Google Scholar]
[7]. Naidoo N, Partab P, Pather N, Moodley J, Singh B, Satyapal KS, Thoracic splanchnic nerves: Implications for splanchnic denervationJ Anat 2001 199:585-90. [Google Scholar]
[8]. Yang HJ, Gil YC, Lee WJ, Kim TJ, Lee HY, Anatomy of thoracic splanchnic nerves for surgical resectionClin Anat 2008 21:171-77. [Google Scholar]
[9]. Last R.J, McMinn R.M.H, Last’s anatomy, regional and applied 1994 6th ednEdinburghChurchill Livingstone [Google Scholar]
[10]. Kuntz A, The Autonomic Nervous System 1934 2nd ednLondonBaillie’ re, Tindall and Cox:28-57. [Google Scholar]
[11]. Reed A.F, The origin of the splanchnic nervesAnat.Rec 1951 109:341 [Google Scholar]
[12]. Mitchell GAG, Anatomy of the Autonomic Nervous System 1953 EdinburghE & S Livingstone [Google Scholar]
[13]. Holinshed WH, Anatomy for Surgeons 1956 volume 2New YorkCassell:197-214. [Google Scholar]
[14]. Pearson A.A, The connections of the sympathetic trunk in the cervical and upper thoracic levels in the human fetusAnat. Rec 1950 106:231 [Google Scholar]
[15]. Saccomanno G, The components of the upper thoracic sympathetic nervesJ.Comp. Neurol 1943 79(issue 3):355-378. [Google Scholar]
[16]. Bradley EL III, Bem, Nerve blocks and neuroablative surgery for chronic pancreatitisWorld J Surg 2003 27:1241-48. [Google Scholar]