Evaluation of post partum headache and seizures is diagnostic challenge. There are various causes for maternal seizures & headache occurring during pregnancy or post partum period. Post partum headache is defined as history of headache, neck & shoulder pain in the first week of delivery [1]. Both the complaints of headache and seizures overlap in most postpartum patients and with causes like cerebral cortical venous thrombosis, ischemic stroke, eclamptic encephalopathy, post partum cerebral angiopathy, neoplastic or infectious causes [2]. Recognition of characteristic imaging findings in these patients helps for the proper management of the cases. There is more often delay in the diagnosis of uncommon but serious conditions in peripartum period because of owing all clinical features to eclampsia and hence reluctance to perform imaging studies. The pathologic conditions resulting in postpartum headache & seizures can be broadly divided into cerebrovascular causes, neoplastic causes & infectious causes.
Materials and Methods
Forty patients with a history of post partum headache and/or post partum seizures are referred for cross-sectional imaging to the Department of Radio-diagnosis in Shri BM Patil Medical College & Hospital, Bijapur, India. The study was conducted for a period of one y from June 2011 to May 2012. Out of 40 patients, 15 had a history of eclampsia. Remaining 25 patients were normotensive and developed post partum headache or seizures within six weeks of delivery. All patients with postpartum headache and seizures were included in the study. Subjects with complaints of more than six weeks were excluded from the study. In this prospective study youngest subject was around 18 y & elder one 38 y old.
Out of 40 patients, 16 presented with single or multiple episodes of seizures, 14 with headache & single or multiple episodes of seizures, five patients presented with headache, unconsciousness & seizures & other five with seizures & unconsciousness.
All 40 patients underwent cross sectional imaging in the form of spiral computed tomography (CT) of brain and magnetic resonance imaging (MRI) of brain. CT brain was performed with 16 slice CT Philips Brilliance and MR brain in Philips Achieva 1.5 Tesla. Initially all patients underwent spiral CT brain, if in doubt further imaging with MRI brain was performed. Intra venous contrast was administered in few cases for the confirmation of diagnosis. Spiral CT brain was viewed in axial & reformatted images. MR brain was performed with T1, T2 & FLAIR sequences with additional sequences of gradient and diffusion weighted imaging. In case of cerebrovascular events MR venography & angiography using time of flight (TOF) sequences were performed. All results were reported in priority bases irrespective of time & intimated immediately to the referring consultants.
Results
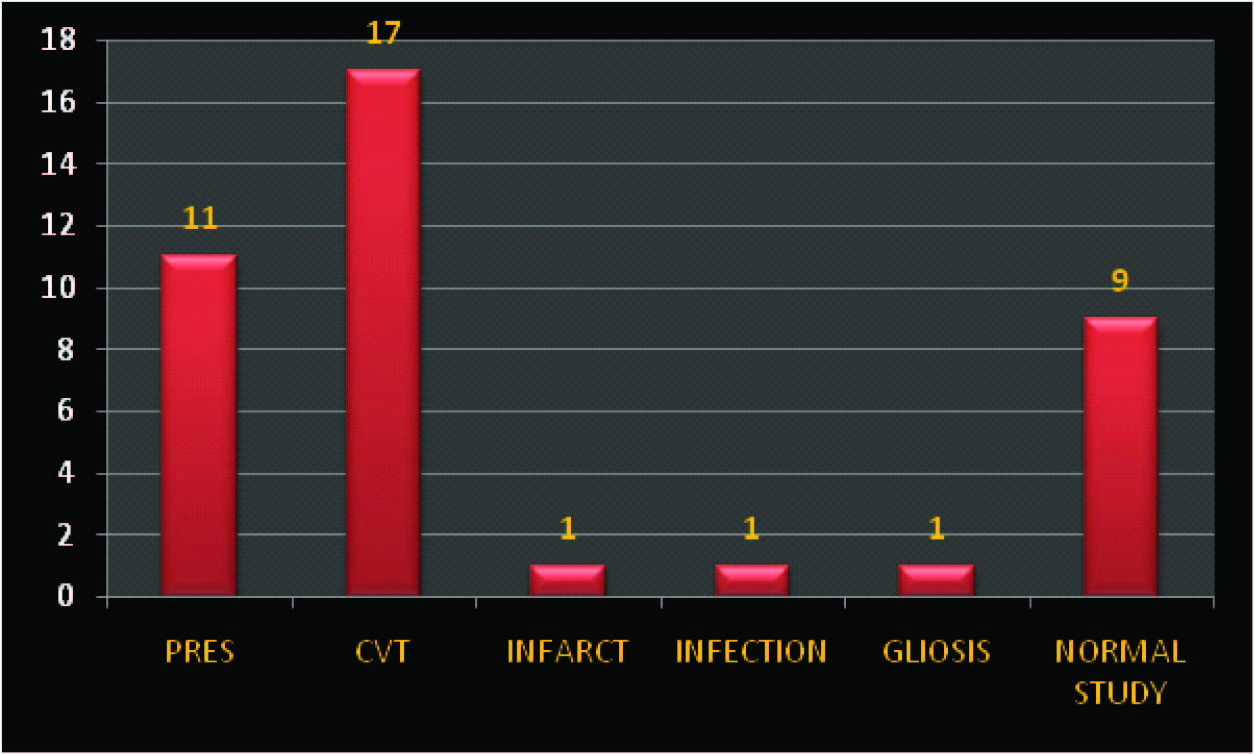
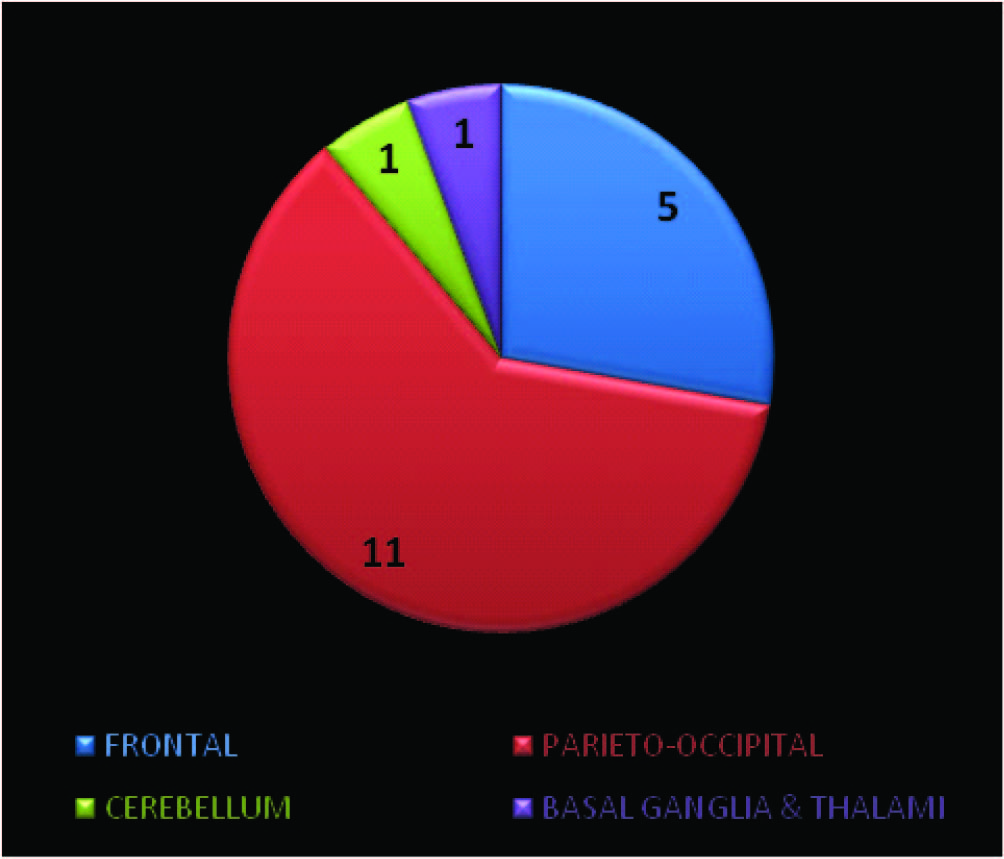
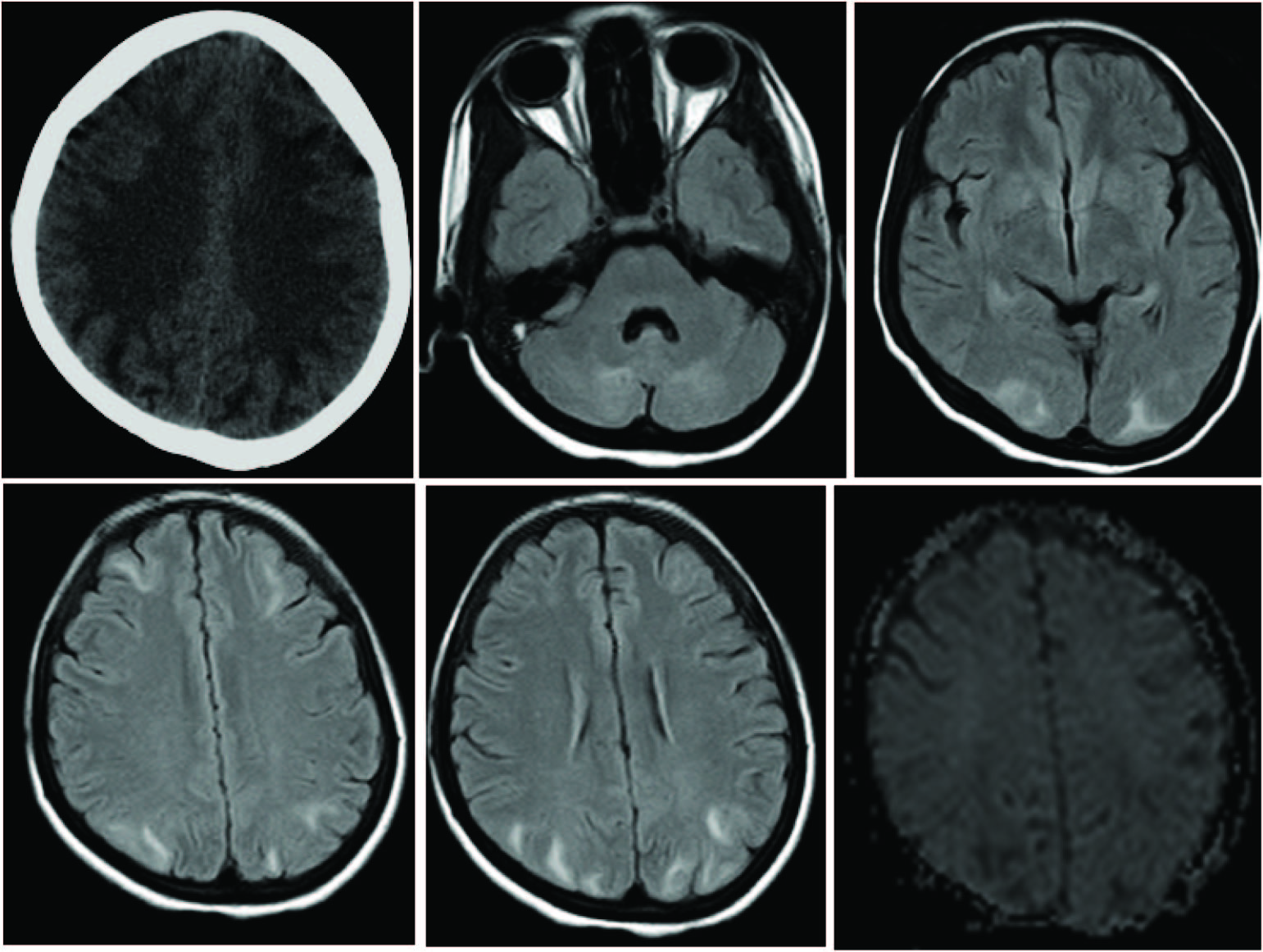
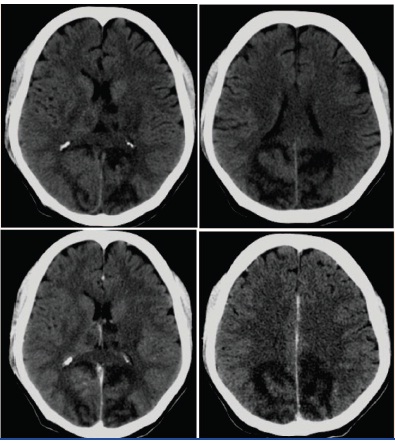
Nine patients with complaints of post partum headache and seizures had no imaging abnormalities in brain. Out of 40 subjects, 11 patients showed features of posterior reversible encephalopathy syndrome (PRES) [Table/Fig-1]. All 11 patients had a history of eclampsia. But out of 15 subjects who presented with complaints of post partum headache and seizures with known eclamptic features, four showed no parenchymal abnormalities in brain on imaging. On CT PRES revealed ill defined subtle white matter hypodensities in bilateral frontal, parietal & occipital regions with variable levels of lobar involvement in different patients [Table/Fig-2]. Few patients showed atypical features of PRES with involvement of both thalami and cerebellar hemispheres [Table/Fig-3]. On MR imaging the white matter lesions were hyperintense on T2, hypointense on T1 and showed free diffusion on diffusion weighted imaging (DWI) [Table/Fig-4].
Distribution of cases of peripartum headache & seizures according to the causative factor
Lesion distribution in PRES
Unenhanced CT (first image), axial FLAIR (next four images) & DWI (second row last image)of patient with PRES. Vasogenic edema is noted in bilateral frontal, parieto-occipital & cerebellar hemispheres with free diffusion on DWI
Unenhanced CT sections of patient with PRES. White matter hypodensities in bilateral parieto-occipital region with atypical involvement of bilateral thalami & basal ganglia
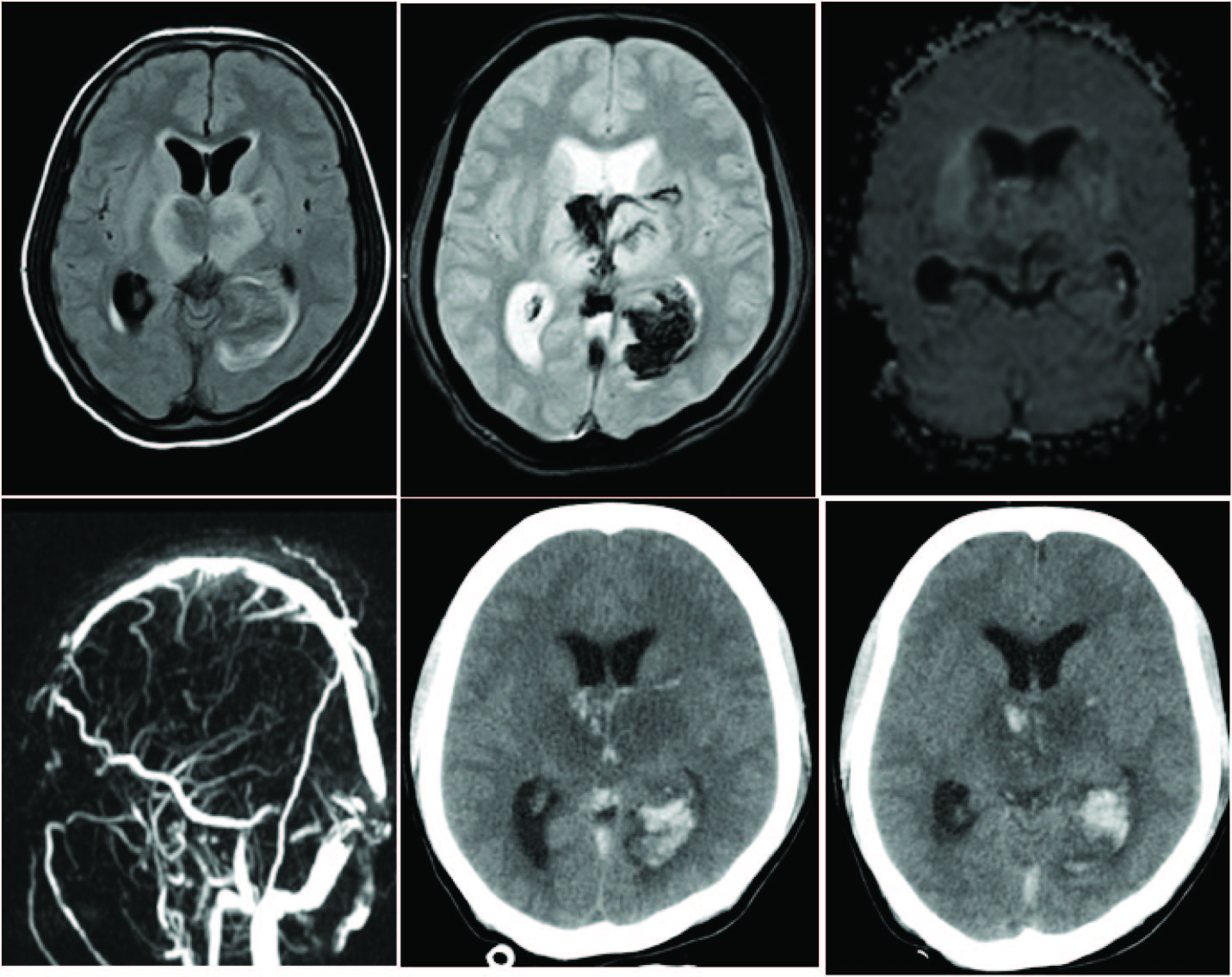
Fourteen patients showed cortical venous thrombosis with parenchymal changes. Distribution of thrombosed cerebral vein with affected parenchymal changes is given in [Table/Fig-5]. Most of the patients with cerebral cortical venous thrombosis had headache, seizures and even unconsciousness status. Three out of 40 patients had cortical venous thrombosis with no evidence of parenchymal changes. Two patients had thromboses of transverse sinus & one had superior sagittal sinus thrombosis. Patients with cortical venous thrombosis showed hyperdense venous sinuses with parenchymal changes on plain CT. Parenchymal changes may be simple vasogenic oedema, ischemic infarct or hemorrhagic infarct. On MR imaging the lesions were heterogeneously hyperintense on T2 & FLAIR sequences & showed mixed free & restricted diffusion on DWI [Table/Fig-6, 7]. On gradient sequences depending on hemorrhage blooming was noted. The affected cortical venous sinuses showed absent flow void on T2 weighted images with blooming on gradient sequences.
Distribution of thrombosed cerebral vein with affected parenchymal changes
| S. No. | Name of thrombosed cortical vein | Region of the brain with parenchymal changes | Number of CVT with parenchymal changes | Number of CVT without parenchymal changes |
|---|
| 1 | Superior sagittal sinus | Unilateral or bilateral fronto-parietal lobes and basal ganglia | 6 | 1 |
| 2 | Transverse sinus | Ipsilateral Parieto-occipito-temporal lobes | 4 | 2 |
| 3 | Deep cerebral vein | Bilateral thalamic, basal ganglia & occipital lobes | 2 | 0 |
| 4 | Straight sinus | Splenium of corpus callosum | 1 | 0 |
| 5 | Superficial cortical vein | Frontal lobe | 1 | 0 |
Axial FLAIR (first image), T2 gradient(second image), DWI (third image), MRV (first image, second row) & unenhanced CT (last two images of second row) sections of patient with deep cerebral vein thrombosis. Parenchymal changes with mixed free & restricted diffusion are noted in bilateral thalami & basal ganglia. Note parenchymal hemorrhage with intraventricular extension
Axial T2 (first image), FLAIR (second image), T2 gradient (third image), DWI (second image, second row), MRV (last image, second row) & axial T2 at lower section (first image of second row) sections of patient depicting left transverse sinus thrombosis resulting left parieto-temporo-occipital parenchymal changes with hemorrhage & mass effect. Parenchymal changes with mixed free & restricted diffusion are noted in left parieto-temporo-occipital lobe with hemorrhage & mass effect. Note hyperintensity in the left transverse sinus with absent flow void on T2 weighted image (first image of second row{Arrow})

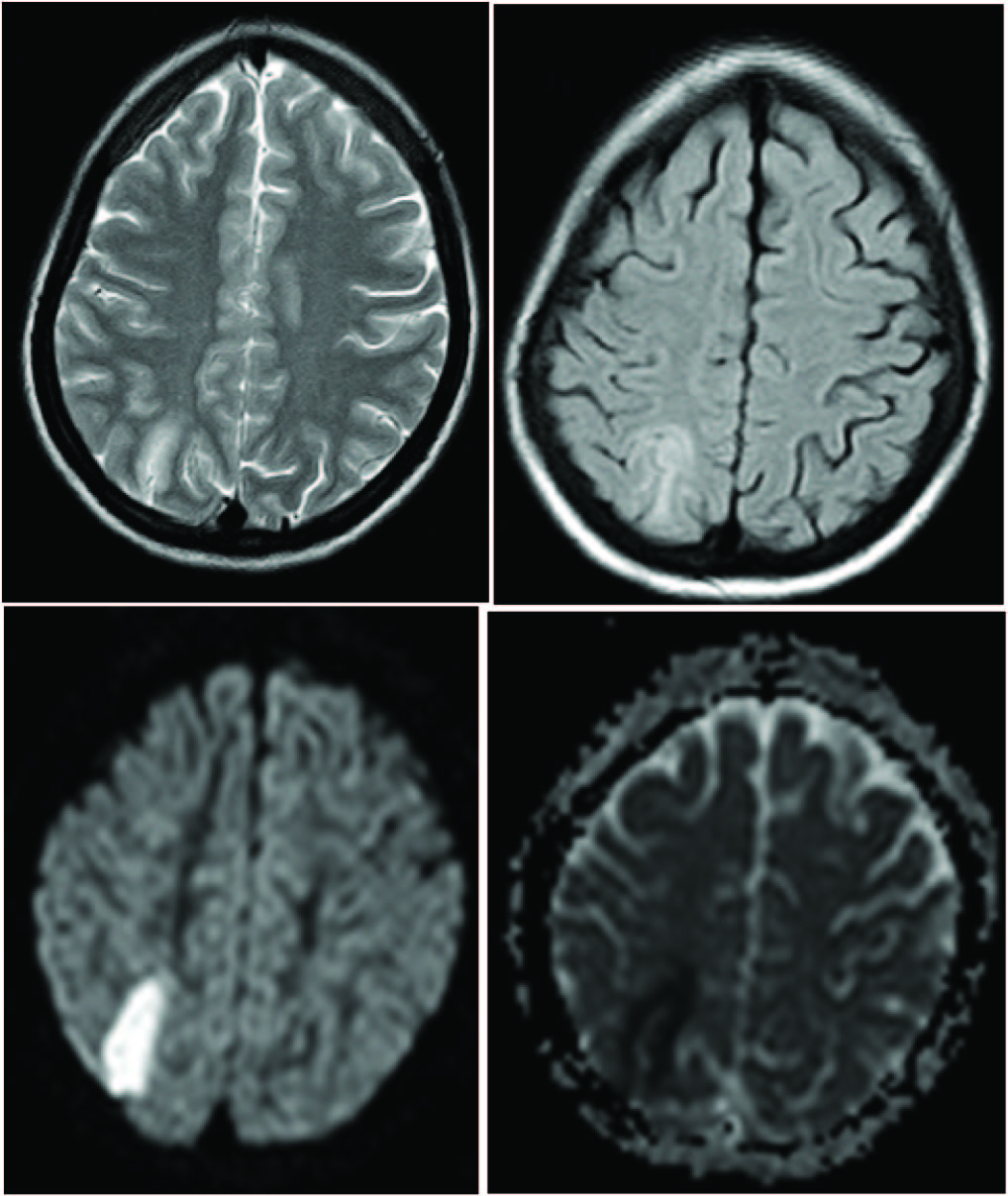
One patient showed watershed territory infarct in right high frontal region between anterior cerebral artery (ACA) & middle cerebral artery (MCA) territories. On CT a well defined band of hypodensity was noted in right high parietal region between ACA & MCA territories. On MR imaging the lesion was hyperintense on T2 and FLAIR and hypointense on T1 weighted images. The lesion showed restricted diffusion on DWI [Table/Fig-8].
Axial T2 (first image), FLAIR (second image), DWI (first image, second row) and ADC (last image, second row) sections of brain of patient with water shed territory infarct. Well defined band of increased signal intensity in right high parietal lobe on T2 & FLAIR with restricted diffusion on DWI & ADC.
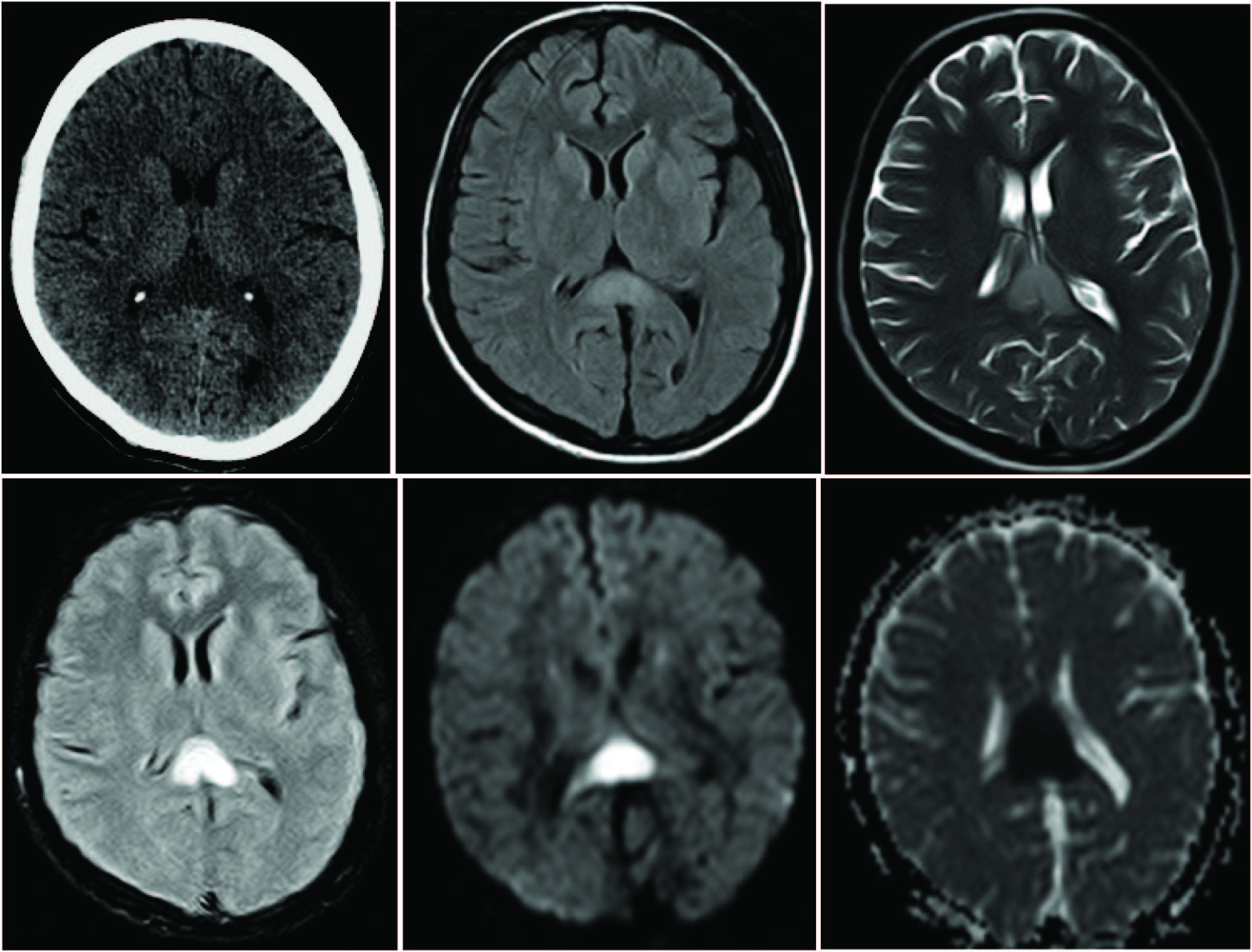
One patient had history of fever, headache & seizures, in which initial CT scan showed mild cerebral oedema. The patient underwent MR imaging of brain with contrast, which revealed non enhancing parenchymal focal lesions with enhancing meninges [Table/Fig-9]. In this case possibility of meningoencephalitis was considered. Later CSF analysis correlated with imaging findings and patient improved with antibiotic course.
First row- Axial T2 (first image) & FLAIR images (next two images ) shows parenchymal signal changes in left deep gray nuclei and bilateral deep white matter. Second row – DWI (first image ) & ADC (second image) show free diffusion in these lesions. Second row – last image and entire third row images – contrast enhanced T1 weighted images show meningeal enhancement with non enhancing parenchymal changes. The features depict menigoencephalitis.

Another patient underwent CT plain and contrast, which revealed a well defined non enhancing CSF density lesion in left caudate nucleus. Apart from this gliotic region no other abnormality were detected in the brain and the seizure focus was thought to be old gliotic lesion.
Discussion
Peripartum seizures are a significant problem which contributes to maternal morbidity and mortality including their unborn children [3]. History of seizures for the first time in peripartum period poses biggest diagnostic muss. Similarly the headache remains the commonest complaint in pregnancy and peripartum phase due to intracranial pathologies [4]. There are diverse group of pathologies leading to peripartum seizures and headache with resultant significant maternal morbidity and mortality. Causes can be classified depending on the conditions specific to physiological process of reproduction like eclamptic encephalopathy, postpartum cerebral angiopathy, subarachnoid hemorrhage and cortical venous thrombosis with or without parenchymal changes and the conditions not related to pregnancy like arterial infarcts, infections, gliotic focuses, and primary or metastatic brain tumours. Early recognition of these conditions and appropriate treatment improves the prognosis and outcome [2]. Imaging with CT and MRI plays an important role in recognition and characterization of these lesions and helps in future management.
Out of all the various causes eclamptic encephalopathy and cortical venous thrombosis are major causes for post partum headache & seizures [3]. In this study 70% of patients suffered from either eclamptic encephalopathy or cortical venous thrombosis, where as 7.5% of patients suffered from other causes.
The incidence of eclampsia in the developing world is reported to be 1 in 100 to 1 in 1700 pregnancies [5]. Eclampsia may result in posterior reversible encephalopathy syndrome, mechanism of which remains unknown [2]. Predilection to the posterior circulation and water shed zones is explained by its sparse vasomotor sympathetic innervations [6].
The current study shows that eclamptic encephalopathy is second most common cause for peripartum seizures and headache accounting for 27.5%. These patients who underwent MR imaging with features of PRES showed free diffusion on DWI.
In eclamptic encephalopathy most commonly involved brain regions are parieto-occipital, frontal, temporal and sometimes even cerebellar hemispheres [7]. In atypical cases even basal ganglia, thalamus & brainstem are involved [8]. In the present research the most commonly involved regions are parieto-occipital (100%) followed by frontal lobe (45%) [Table/Fig-2]. One patient each showed involvement of cerebellum & thalami. In study conducted by Richard B et al., in 20 patients with eclamptic encephalopathy, most commonly involved region was occipital lobe followed by parietal lobe [9]. In his research two patients showed changes in the cerebellum [9]. Another study conducted by Bartynki et al., showed that parieto-occipital lobe involvement is seen in 98% followed by frontal lobe involvement in 68% [10]. Changes in the cerebellar hemispheres were noted in 32 % of patients in his research [10].
Venous thromboembolism including cerebral venous thrombosis (CVT) is well established complications in pregnancy and puerperium, secondary to physiological changes in the coagulation system [11]. The incidence of CVT accounts for 20% of pregnant patients with mortality rate ranging from 4% to 33%. Young mothers and cesarean section are two most important risk factors in peripartum phase for the development of cerebral venous thrombosis. Clinically the patients with CVT come with history of head ache, vomiting, seizures, mental status changes & even in coma [12,13]. It is important to differentiate this condition from other causes of headache and seizures like PRES and post partum cerebral angiopathy.
MRI is more sensitive in picking up lesions and their extent than CT. In CVT the parenchymal changes on MRI can be sub classified by doing DWI as parenchymal abnormalities with vasogenic oedema or cytotoxic oedema with or without hemorrhages [Table/Fig-10]. In some patients mixture of all patterns may coexist [14]. Diagnostic merit of MRI can be enhanced by performing MR venography (MRV) with contrast or without contrast using time of flight sequences.
First row- First image unenhanced axial CT, axial FLAIR (second image), axial T2 (third image), axial T2 gradient (second row – first image), axial DWI & ADC (second row – last two images) sections of patient with straight sinus thrombosis with venous infarct in the splenium of corpus callosum. Subtle hypodensity is noted in the splenium of corpus callosum on CT, which is hyperintense on T2 and FLAIR with restricted diffusion on DWI & ADC.
In the current study CVT is the major cause for the peripartum headache and seizures accounting for 42.5%. Out of 17 patients with cerebral venous thrombosis, three patients showed no parenchymal changes. Most commonly thrombosed sinus in CVT is superior sagittal sinus in non specific conditions, where as lateral and cavernous sinuses are involved secondary to sepsis. In our study most commonly involved sinus is superior sagittal sinus in seven cases (41.1%) followed by transverse sinus in six cases (35.2%).
Ischemic strokes are not uncommon essence in the peripartum period, as pregnancy & puerperium are hypercoagulable states. Stroke associated with pregnancy has significant morbidity and mortality [2]. There are various causes for ischemic stroke including cardiac emboli or paradoxical emboli in cardiac diseases, coagulopathies and arterial dissections [15]. Water shed infarcts are known entities in peripartum period secondary to the dissections of arteries and serious post partum hemorrhages [2]. In the present study one patient showed water shed territory infarct in right high parietal lobe.
Meningitis and menigoencephalitis are common in peripartum period due to obstetric spinal anesthesia. Patients presents with complaints of fever, headache and seizures. Out of 40 patients, one patient had features of menigoencephalitis with enhancing meninges & parenchymal signal changes on contrast enhanced MRI.
Fibrillary gliosis resulting from prior brain injury bordering the normal neuronal tissue can trigger epilepsy by impairing the homeostasis of extracellular potassium ions [16]. In late 1940s Penfield and co workers established that glial scar is a irritable source for the focal seizures, which develop either by anoxic or traumatic brain damage [16]. One patient in the present research had post gliotic seizures due to traumatic gliotic scar in the brain.
There are other important causes of peripartum headache and seizures like subarachnoid hemorrhages (SAH), post partum cerebral angiopathy and neoplastic lesions (primary or metastatic). None of our patients had SAH, posterior cerebral angiopathy or neoplastic lesions.
As we come across spectrum of causes for peripartum headache and seizures including both cerebrovascular disorders and neoplastic disorders, the imaging plays an important role in their management. Every causative event has characteristic imaging findings which excludes the other causes and helps in fine tuning of the treatment. Sometimes imaging findings may be non specific, but awareness of increased frequency of certain disorders in peripartum period may narrow the differential diagnosis. Most of maternal mortalities in these conditions are due to delayed diagnosis and reluctance of CT & MR imaging. Hence, earlier and liberal use of cross sectional imaging and proper diagnosis of peripartum headache and seizures can bring down the mortality by establishing proper management.
Conclusion
PRES and CVT are two most important causes of peripartum head ache & seizures. Proper clinical judgement and bounteous use of cross sectional imaging in these patients helps in pinning down the diagnosis, providing appropriate treatment and thereby reducing the maternal mortality & morbidity.