An Unusual Complication of Esophageal Stenting for Corrosive Acid Injury
Kirti Katherine Kabeer1, N. Ananthakrishnan2, S. Manoj Karthik3, R. Pajanivel4, M. Ravishankar5
1 PG Training, Department of General Surgery, Mahatma Gandhi Medical College and Research Institute, Pondicherry, India.
2 Professor, Department of General Surgery, Mahatma Gandhi Medical College and Research Institute, Pondicherry, India.
3 Associate, Professor, Department of General Surgery, Mahatma Gandhi Medical College and Research Institute, Pondicherry, India.
4 Professor, Department of General Surgery, Pulmonary Medicine, Mahatma Gandhi Medical College and Research Institute, Pondicherry, India.
5 Professor, Department of Anaesthesiology, F.R.C.S., Mahatma Gandhi Medical College and Research Institute, Pondicherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Kirti Katherine Kabeer, PG Training, Department of General Surgery, Mahatma Gandhi Medical College and Research Institute, Pondicherry-607402, India. Phone : +91 7639285303, E-mail : kirti.katherine@gmail.com
Corrosive acid, Esophageal stenting
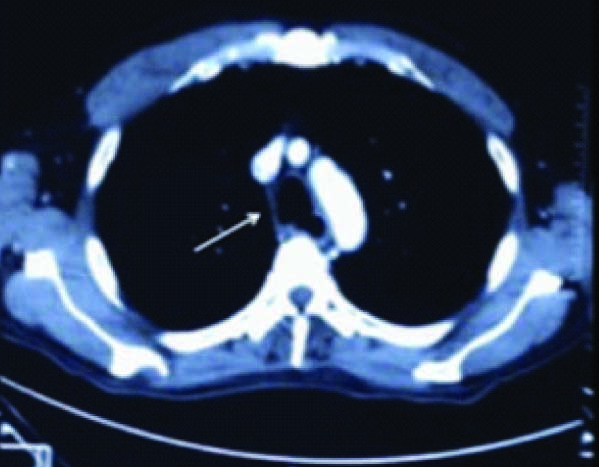
A 50-year-old male, presented with history of accidental ingestion of toilet cleaning acid a month before admission. Due to respiratory embarrassment an emergency tracheostomy and feeding jejunostomy were done at another hospital. A subsequent CT thorax at the same hospital showed a tracheo-esophageal fistula proximal to the carina [Table/Fig-1]. Upper Gastrointestinal Endoscopy(UGIE) showed a large fistulous communication between the esophagus and trachea at 30cms. A self-expanding 15 cm. long covered metal stent was placed with the proximal end at 23cms. The time interval between the initial acid injury and placement of the stent was two weeks. As the patient had developed a tracheo-esophageal fistula within the first two weeks of injury, the treating team could not wait for fibrosis to set in prior to stenting. The tracheostomy was closed and the patient was discharged with the feeding jejunostomy.
CT Thorax showing the trachco-esophageal fistual
Two months later, the patient was re-admitted with complaints of persistent cough with expectoration. Chest X-ray was normal, UGIE showed a complete block at the level of the crico-pharynx. The cough was attributed to aspiration consequent to high esophageal obstruction. The patient was then referred to us.
Repeat CT neck and thorax showed the metal stent in the esophagus to be entering the trachea, the left main bronchus and partly into the right main bronchus. There was no tissue shadow between the esophagus and distal trachea indicating complete disruption of the tracheal and esophageal walls [Table/Fig-2]. UGIE could not be repeated, as there was total obstruction at the pharyngo-esophageal junction.
CT Thorax and brochoscopy image the esophageal stent in the trachea with absence of tissue between the trachea and esophagus
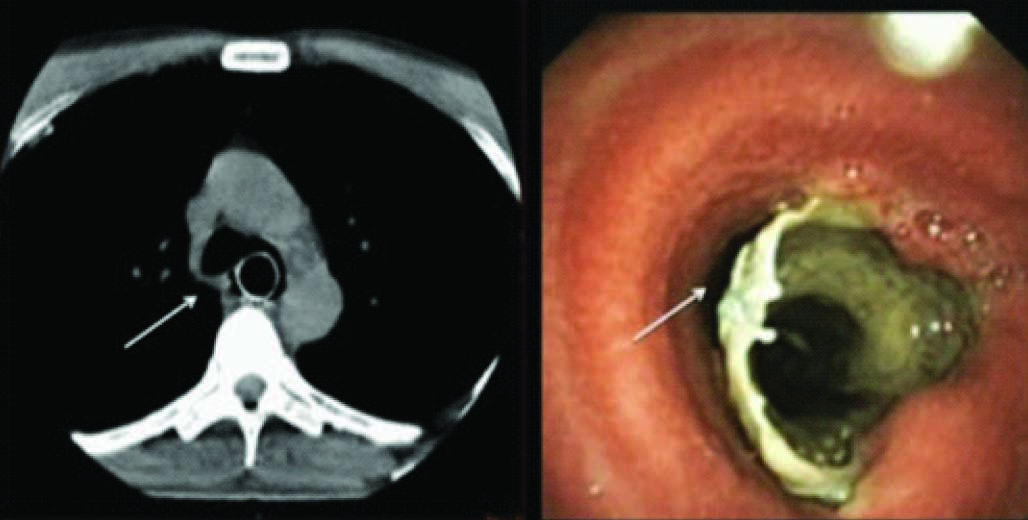
Bronchoscopy visualized the proximal end of the stent in the trachea [Table/Fig-2]. A small slit like passage was seen anterior to the stent on bronchoscopy through which the patient was maintaining ventilation. The distal end of the stent opened into the supra-diaphragmatic esophagus, which led to the stomach.
The plan to do a pharyngo-colic bypass had to be abandoned as the anaesthetist felt that a satisfactory airway couldn’t be established in this patient for ventilation. On attempting to intubate and ventilate the patient, most of the ventilatory gases would have gone through the stent into the stomach. Endo-bronchial intubation was considered, but the lumen of trachea that was patent was too narrow.
Discussion
Stenting remains the standard treatment for corrosive tracheo-esophageal fistula. Several complications are known to be associated with esophageal stents. Stent migration is the most common, occurring with a frequency of 7-75% [1,2]. The stent placed in the esophagus in this patient was found to have eroded through the intervening esophageal and bronchial tissue entering the bronchus converting the two passages in to a single lumen. Consequently, regurgitation of gastric contents led persistent cough. This complication is rare and has been reported previously in cases where esophageal stent placements were done for neoplastic trachea-esophageal fistulae [3].
[1]. Hindy P, Hong J, Lam-tsai Y, Gress F, A Comprehensive Review of Esophageal StentsGastroenterology & Hepatology 2012 8(8):526-34. [Google Scholar]
[2]. Adam A, Stenting of the Upper Gastrointestinal Tract Current StatusCardiovasc Intervent Radiol 2010 33:690-705. [Google Scholar]
[3]. Katsanos DD K, Sabharwal T, Koletsis E, Fotiadis N, Roy-Choudhury S, Adam A, Direct erosion and prolapse of esophageal stents into the tracheobronchial tree leading to life-threatening airway compromiseJournal of Vascular Interventional Radiology 2009 20(11):1491-95. [Google Scholar]