An Unusual Association of Inflammatory Pseudotumor of the Liver and Dorsal Pancreatic Agenesis Presenting as Reversible Portal Hypertension: A Case Report
Ankur Jain1, Naresh Gupta2, Praveen Bharti3
1Postgraduate Resident, Department of Medicine, Maulana Azad Medical College, Bahadur Shah Zafar Marg, Delhi, India.
2Director, Professor and Head, Department of Medicine, Maulana Azad Medical College, Bahadur Shah Zafar Marg, Delhi, India.
3Senior Resident, Department of Medicine, Maulana Azad Medical College, Bahadur Shah Zafar Marg, Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ankur Jain, BL-Taneja Block, Department of Medicine, Maulana Azad Medical College, Bahadur Shah Zafar Marg, Delhi-110002, India.
Phone: 9910265555,
E-mail: drankur589@yahoo.in
Inflammatory pseudotumor of liver although a rare entity is an important differential diagnosis of hepatic space occupying lesions as well as an important cause of portal hypertension, commonly mimicking malignant tumors on imaging and histology. We report a case of a 25-year-old postpartum female who presented to our emergency with seizures and altered sensorium and was found to be having uncontrolled hyperglycemia and metabolic encephalopathy. She had a 2 month history of low grade fever and pain in right hypochondrium. Examination revealed an enlarged, tender, left lobe of the liver, splenomegaly and ascites. CT scan of the abdomen revealed an ill-defined mass lesion in left lobe of the liver with dilated intrahepatic biliary radicles along with dorsal pancreatic agenesis and evidence of portal hypertension in the form of ascites and splenomegaly. Histopathology confirmed the presence of inflammatory pseudotumor in left lobe of the liver. Conservative management of the patient resulted in reduction of the tumor size and regression of splenomegaly and ascites in 1 month. Present case highlights inflammatory pseudotumor of liver as a rare entity, it’s resemblance to malignant conditions, pancreatic agenesis as a previously unreported association as well as a potentially reversible cause of portal hypertension by conservative treatment only.
Agenesis of pancreas, Conservative management, Hepatic pseudotumor, Left lobe of liver, Portal hypertension
Case Report
A 25-year-old young lady presented to the medical emergency department with complaints of seizures and altered sensorium since 1 day. Patient was 5 months postpartum and delivered a healthy baby by normal vaginal route. She began to develop low grade fever, associated with reduced appetie and weight loss after 3 months of delivery. She also complained of pain in right hypochondrium; however she denied jaundice, malena, haemetemesis, cough, hemoptysis, menstrual abnormalities or any history of prior abortions or history suggestive of autoimmune disorder. She developed seizures and went into altered sensorium and was brought to the emergency department. General examination revealed severe pallor and cachexia, however there was no icterus, clubbing, lymphadenopathy, pedal edema and findings of connective tissue disorder. Abdominal examination revealed an enlarged, tender left lobe of the liver, about 6-7 cm below the costal margin and a palpable spleen with free fluid in the abdomen. Neurological Examination of the patient was unremarkable without any focal deficit. Cardiovascular and respiratory system examination were unremarkable.
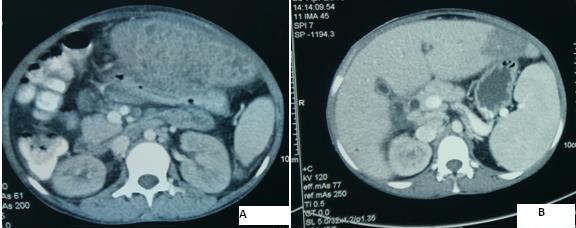
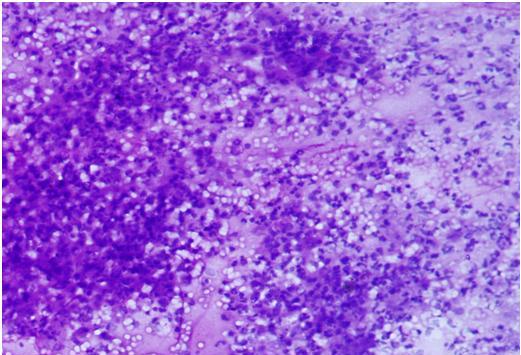
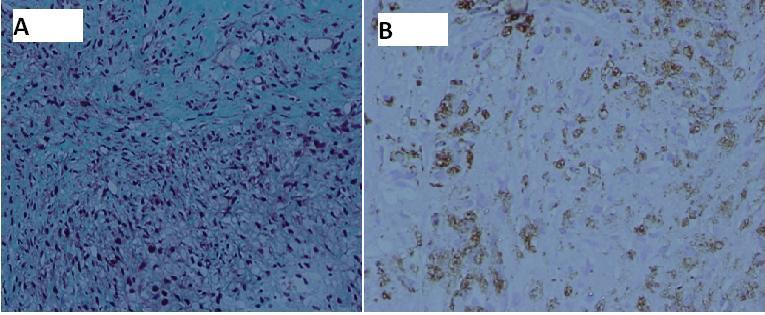
Routine investigations of the patient revealed-Hb-4.7 gm%, total leucocyte count-19620/cumm3, Differential count-Polymorphs 85%, lymphocytes 15%, Platelets-3.15 Lakh/cumm3, ESR-78mm/hr, random blood sugar of 350mg% without any evidence of ketoacidosis and Glycated Hemoglobin was 8.7%. Peripheral smear revealed normocytic normochromic anemia with occasional presence of microcytic hypochromic cells without any atypical cells. Liver function tests revealed ALP-540U/L; total protein-5.2 gm%, Serum albumin-2.1 gm%, AST-35U/L, ALT- 46U/L. Total calcium-8.0mg%, phosphorous-4.0mg% and renal function tests were normal. Tuberculin skin test was negative; induced sputum examination revealed no acid fast bacilli (AFB) and was negative hypertensionfor fungal elements. CSF was acellular with sugar-67mg%, proteins-56mg% and results of gram’s staining, ZN staining and India ink, culture and PCR for Mycobacterium tuberculosis were negative. Patient’s Chest X-ray, non contrast CT head and MRI brain were normal and her blood cultures, amoebic serology and hydatid serology were negative. Patient’s serology for antinuclear antibodies (ANA), anti-double stranded DNA, anti-LKM, anti-SMA, anti-SLA, p-ANCA, and c-ANCA, Thyroid function tests, Serum Angiotensin converting enzyme (ACE) levels was normal. Serum carcino-embryonic antigen (CEA), alpha fetoprotein (AFP) and CA-125 levels were normal. HIV antigen 1 and 2, Australia antigen and anti-HCV were negative. Ultrasound of the abdomen revealed an enlarged liver (17.5 cm), enlarged spleen (14 cm), a heterogenous lesion in the left lobe of the liver about 8x8 cm in diameter without any internal vascularity and the presence of free fluid. Ascitic fluid analysis revealed a transudative ascites: serum albumin ascitic ratio (SAAG)-1.4, total cell count-50, Polymorphs 60%, lymphocytes 40%, Sugar-100mg%, Proteins-0.6mg%, Adenosine deaminase (ADA)-15U (normal). Results of gram’s stain, culture, ZN stain were negative. Serum Ceruloplasmin levels were normal and slit lamp was negative for KF ring. Upper GI Endoscopy was normal. Contrast enhanced CT scan of the abdomen revealed irregular bilobar Intrahepatic biliary radical dilatation with focal narrowing of common bile duct at porta hepatis with enlarged left lobe of liver with an ill-defined hypodense lesion in left lobe measuring 9X6X10 cm in size along with dorsal pancreatic agenesis, splenomegaly and ascites [Table/Fig-1a]. Further imaging with Magnetic resonance cholangiopancreatography (MRCP) abdomen revealed an ill-defined heterogenously enhancing lesion in segment-3 of the liver with bilobar intrahepatic biliary dilatation and dilated common bile duct with splenomegaly and ascites. Fine needle aspiration cytology (FNAC) of the lesion revealed sheets of inflammatory cells mainly polymorphs, lymphocytes and macrophages suggestive of acute on chronic abscess [Table/Fig-2]. Stain for AFB was negative. Trucut biopsy of the lesion was done which revealed that the liver was replaced by fibrous tissue and showed the presence of CD-68 positive histiocytes in the lesion with chronic inflammatory cell infiltrate consisting of lymphocytes and fibroblasts [Table/Fig-3a,b]. The findings were consistent with the diagnosis of inflammatory pseudotumor of the liver. Patient was managed initially by insulin infusion for uncontrolled hyperglycemia and was given injectable antibiotics including metronidazole and ceftriaxone along with blood transfusions. Patient improved during hospital stay and her fever subsided after 4 weeks of treatment. Alkaline phosphatase levels and total leucocyte counts decreased gradually and clinically patient’s liver and spleen size reduced over a period of 1 month. Patient was discharged after 1 month and after 2 months of follow up, showed significant reduction of lesion on repeat CT scan without ascites and normal spleen size [Table/Fig-1b].
Discussion
Inflammatory pseudo-tumor (IPT) is a rare benign condition first described in 1939 in the lung and described first by Pack and Baker in the liver in 1953 [1]. Etiology of IPT remains uncertain although infection, chemotherapy and radiation have been suggested as possible etiologies [2]. IPT has been associated with a number of conditions including diabetes mellitus, Crohn’s disease, chronic ascending cholangitis, Sjögren’s syndrome, gout, primary sclerosing cholangitis, acute myeloblastic leukemia, Kostmann’s disease, autoimmune pancreatitis, HIV, stem cell transplantation, gastro-intestinal stromal tumours and pregnancy [3,4]. Right lobe of liver represents the commonest location although Weiss et al., have reported a case of hepatic IPT with multicentric lesions [5]. Isolated left lobe IPT of liver however, is uncommon. Biliary obstruction, portal hypertension and cirrhosis can complicate hepatic IPT, particularly those involving the hilum [5]. Due to non-specific clinical, histological and radiological appearance of the lesions, diagnosis of IPT is challenging and can be easily confused with granulommatous conditions like tuberculosis, sarcoidosis, lymphomas, and most importantly hepatocellular carcinoma, the fact which underscores the importance of correctly identifying this lesion [6]. Diagnosis relies upon percutaneous biopsy of the lesion although usually made after hepatic resection in various case series [7]. Although spontaneous regression of IPT has been reported with conservative management with antibiotics, steroids and Non steroidal anti-inflammatory agents, surgical resection is the treatment of choice especially in cases of diagnostic dilemma, non-response to conservative treatment and is especially indicated in cases complicated by biliary obstruction and portal hypertension [4]. Ueda et al., reported a case of IPT involving hepatic hilum and complicated by obstructed jaundice and portal hypertension which was managed with hepatic resection [8]. Present case represents a unique case of portal hypertension due to IPT localized to the left lobe of the liver and associated with pancreatic agenesis, an association never been described earlier. Pregnancy was probably the triggering factor and response to antibiotics makes infection a likely etiology in our case. Portal hypertension is considered a classical indication of surgical resection in a case of hepatic IPT, however, our patient showed dramatic response to antibiotics in one month without the use of glucocorticoids, not only with regression of the lesion, but with reversal of portal hypertension as well. Isolated hepatic IPT of the left lobe, its association with pancreatic agenesis, and reversible nature of the portal hypertension with only conservative management makes this the first such reported case of hepatic IPT.
Pretreatment contrast enhanced CT abdomen of the patient showing a heterogenous mass lesion in the left lobe of the liver measuring 9X6X10 cm in size (1a) and CT scan of the same patient after 1 month of the treatment showing a significant reduction in size of the lesion (1b)
Fine needle aspiration cytology (FNAC) of the lesion showing an inflammatory infiltrate composed of Polymorphonuclear and mononuclear cells
Biopsy of the lesion showing that liver is replaced by fibrous tissue as shown by Masson’s trichrome stain (3a) and lesion containing CD-68 positive histiocytes (3b)
Conclusion
Hepatic IPT is a rare condition, but should be remembered as a cause of space occupying lesion and portal hypertension especially when imaging features suggests malignancy. Trucut biopsy is recommended for diagnosis as FNAC can be unrevealing. A trial of conservative treatment should be given due to potentially reversible nature of the lesion, including portal hypertension. we conclude that a diligent search for other associated conditions should also be made which can help in better patient management.
[1]. GT Pack, HW Baker, Total right lobectomy. Report of a caseAnn Surg 1953 138:253-58. [Google Scholar]
[2]. J Fangusaro, K Klopfenstein, J Groner, S Hammond, RA Altura, Inflammatory myofibroblastic tumor following hematopoietic stem cell transplantation: report of two pediatric casesBone marrow Transplant 2004 33:103-07. [Google Scholar]
[3]. W Faraj, H Ajouz, D Mukherji, G Kealy, A Shamseddine, M Khalife, Inflammatory pseudo-tumor of the liver: a rare pathological entityWorld J Surg Oncol 2011 9:1-5. [Google Scholar]
[4]. T Al-Jabri, P Sanjay, I Shaikh, A Woodward, Inflammatory myofibroblastic pseudotumour of the liver in association with gall stones - a rare case report and brief reviewDiagn Pathol 2010 5:53 [Google Scholar]
[5]. GA Weiss, DB Shor, P Schachter, Inflammatory pseudotumor of the Liver: an unlikely cause of multiple hepatic lesionsIsr Med Assoc J 2007 9:894-95. [Google Scholar]
[6]. A Nitinas, D Kardassis, D Miliaras, K Tsinoglou, A Dimitriades, D Vrochides, Inflammatory pseudotumor of the liver: a case report and review of the literatureJ Med Case Rep 196 5:196-99. [Google Scholar]
[7]. GD Calomeni, EB Ataíde, RR Machado, CA Escanhoela, LB Costa, IF Boin, Hepatic inflammatory pseudotumor: A case seriesInt J Surg Case Rep 2013 4:308-11. [Google Scholar]
[8]. M Ueda, Y Yukihide, K Ogawa, H Haga, Y Ogura, T Ito, A case of inflammatory pseudotumor of the liver hilum successfully treated with aggressive hepatectomyJ Pediatr Surg 2003 3:9-11. [Google Scholar]