Secondary Vaginal Atresia Treated with Vaginoplasty Using Amnion Graft: A Case Report
Setu Rathod1, Sunil Kumar Samal2
1 Assistant Professor, Department of Obstetrics and Gynaecology, Mahatma Gandhi Medical College & Research Institute, Puducherry, India.
2 Assistant Professor, Department of Obstetrics and Gynaecology, Mahatma Gandhi Medical College & Research Institute, Puducherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sunil Kumar Samal, 4-D, Type II Staff Quarters, Mahatma Gandhi Medical College, Pillaiyarkuppam, Puducherry-607402, India.
Phone: 07598461660,
E-mail: drsksamal1981@gmail.com
We report a case of 26-year-old primipara with last child birth 1.5 year back who presented with amenorrhoea, cyclical lower abdominal pain and dyspareunia for past six months. Examination revealed vaginal atresia secondary to previous traumatic/mismanaged vaginal delivery with haematocolpos. She was managed by vaginoplasty with amnion graft and regular dilation with soft vaginal mould for six weeks and was advised for regular intercourse after that. On follow up our patient was doing well with restoration of normal coital function.
Amenorrhoea, Mismanaged vaginal delivery, Vaginal mould
Case Report
A 26-year-old primipara with last child birth one year back, presented with dyspareunia and cyclical pain for last four months. She belonged to a tribal community with lower socioeconomic status. There was history of instrumental delivery in previous pregnancy for prolonged second stage of labour with fetal distress. She delivered a term female baby with birth weight 3800 gm in the previous pregnancy. According to her, postpartum period was uneventful and she had normal lochial flow during first two weeks. Following the delivery, the baby was exclusively breast-fed for six months. She had history of two menstrual cycles after four months of delivery which were irregular with scanty flow of 1-2 d duration. Following that she was amenorrhoeic since last six months. She had no urinary or bowel complaints.
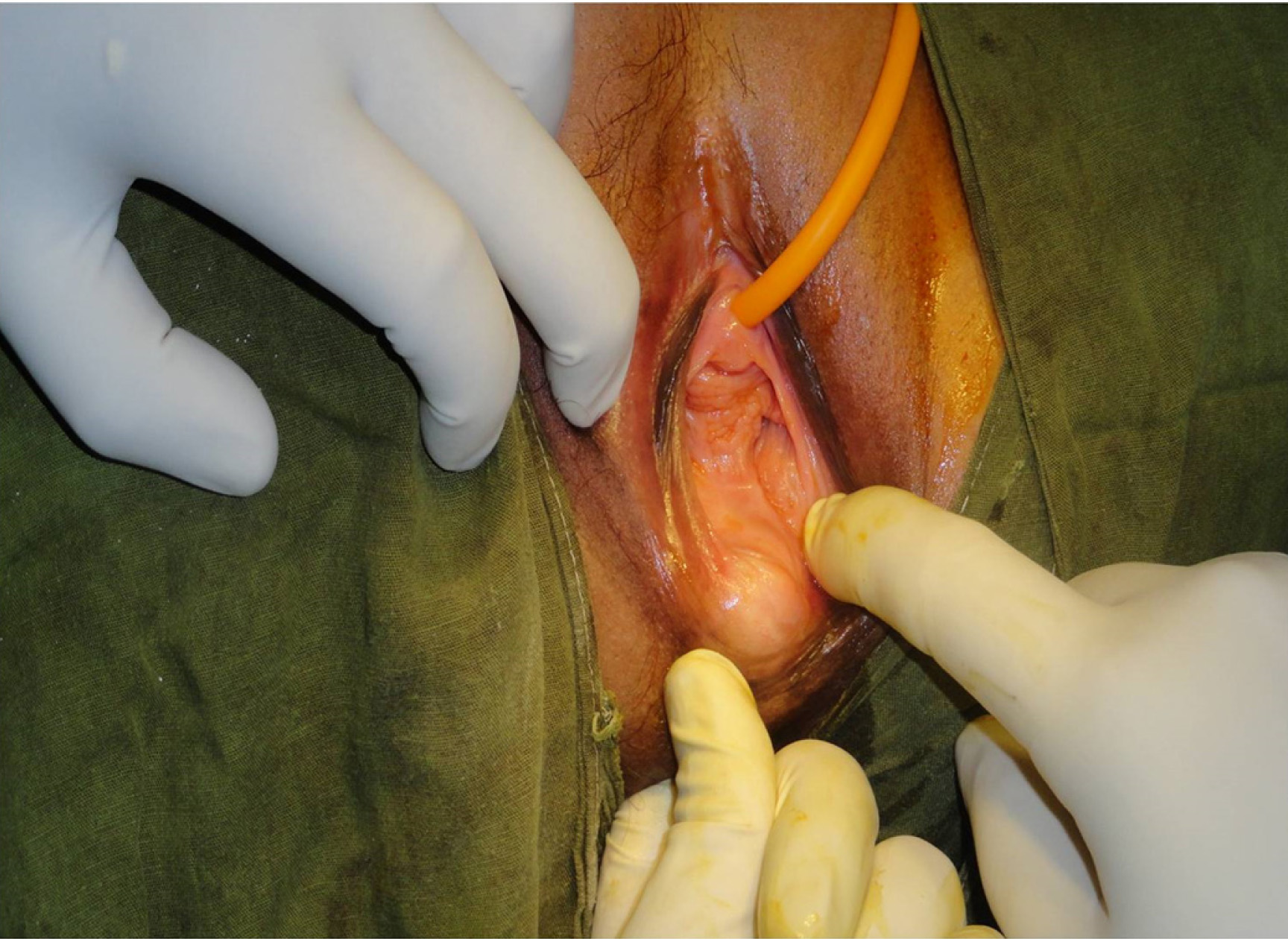
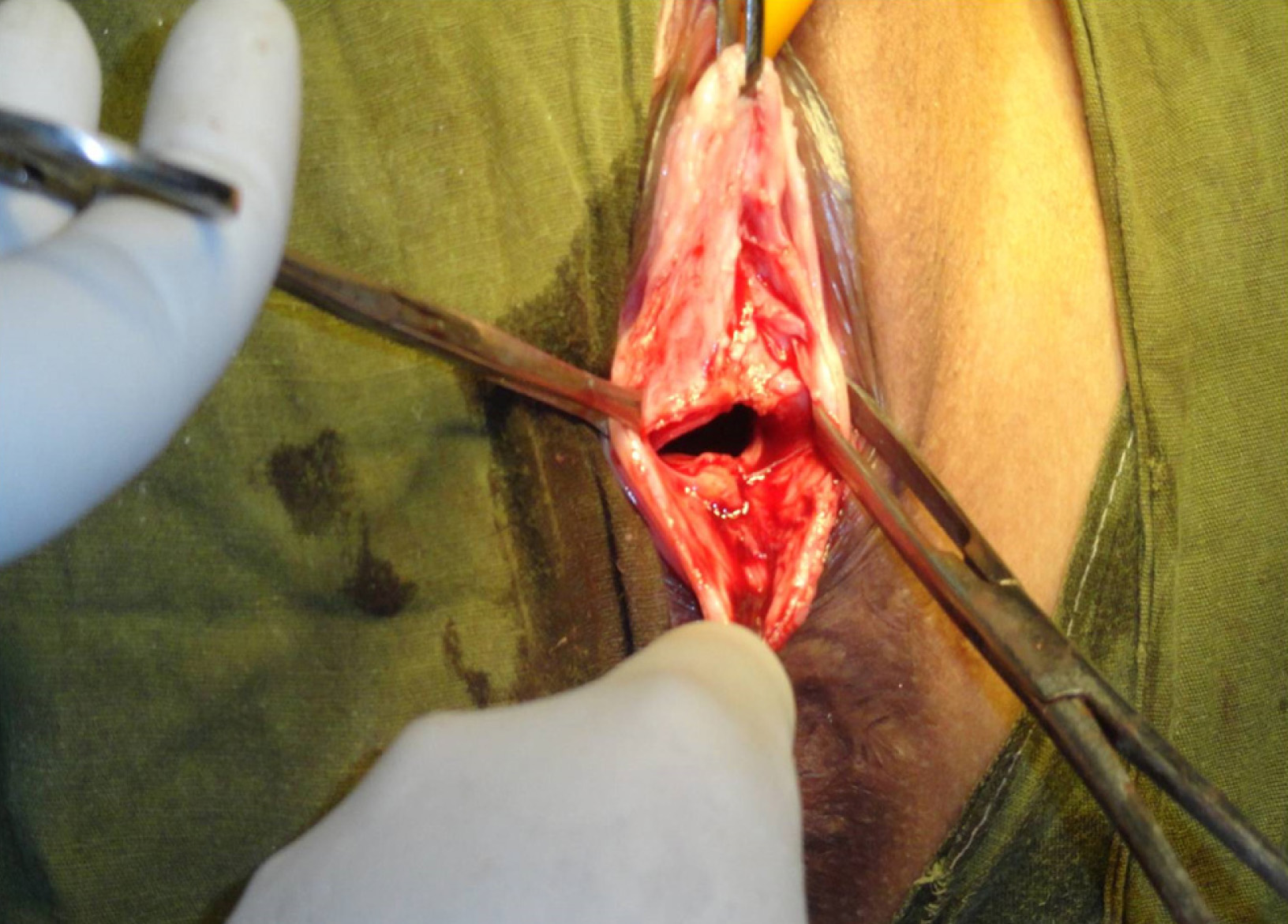
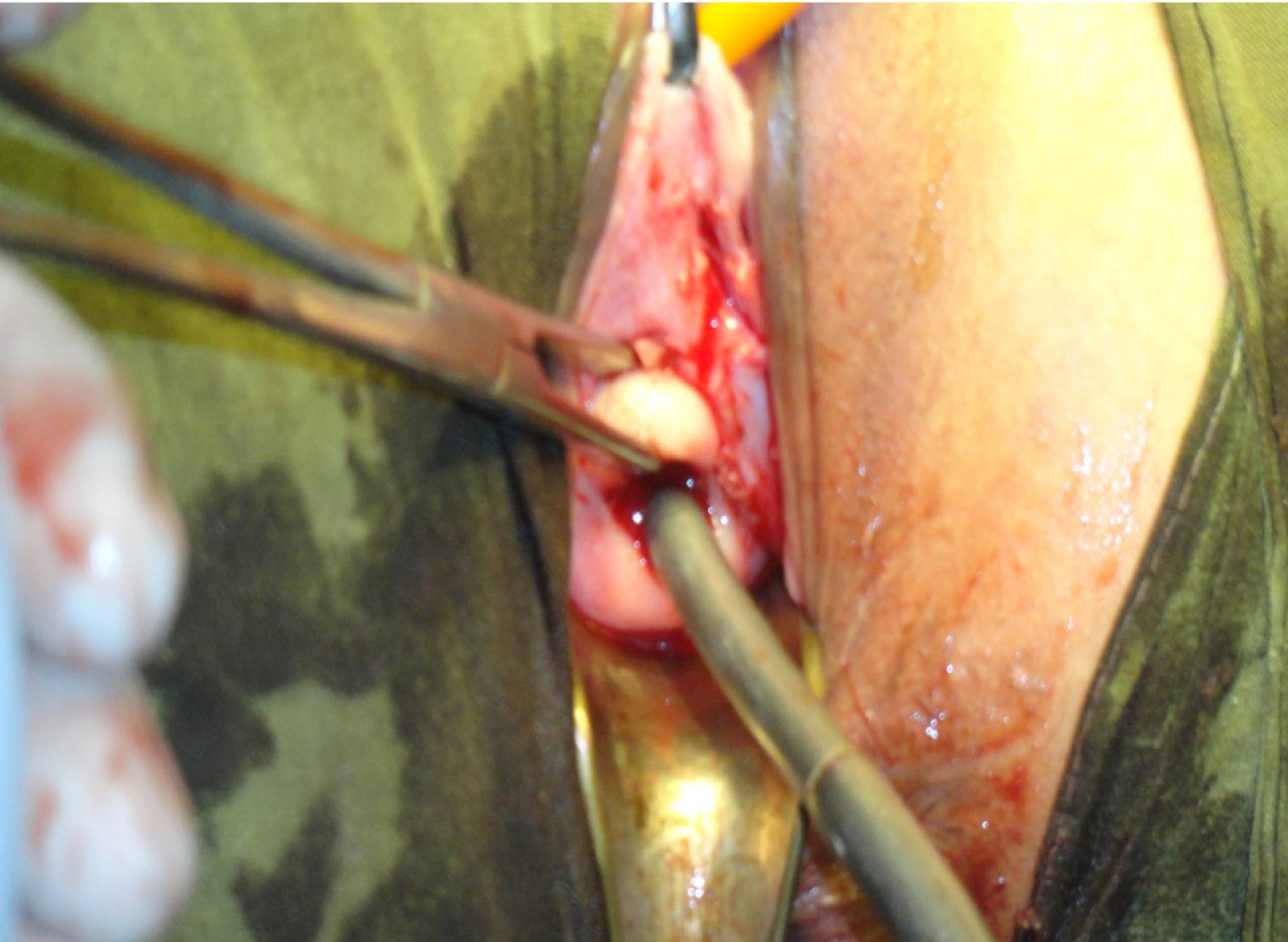
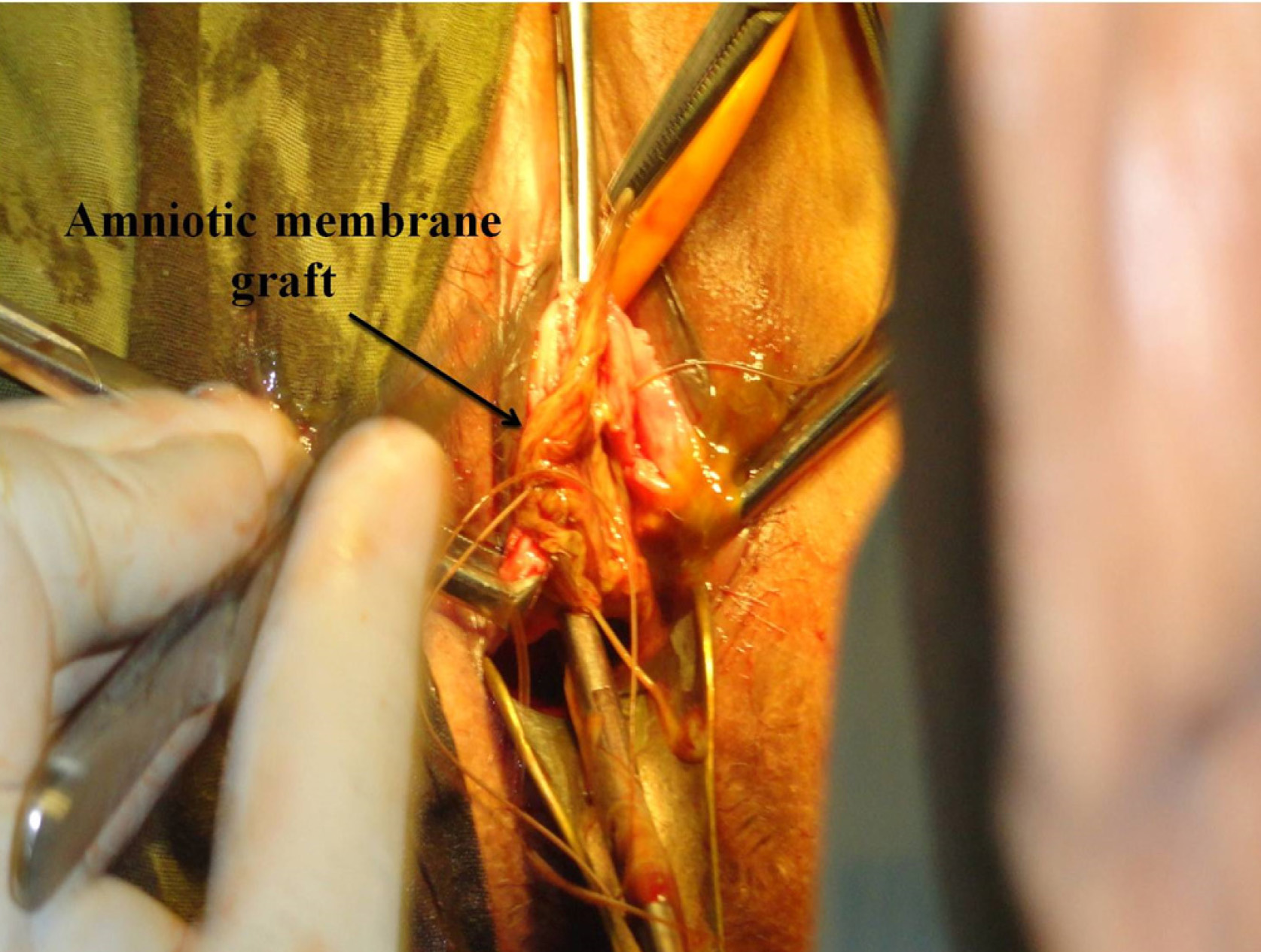
General and systemic examination revealed no abnormality. On per speculum examination, there was fusion of upper vaginal wall with non visualisation of cervix [Table/Fig-1]. The lower part of vaginal canal was intact. The urethral orifice, mons pubis, labia majora and the anus were normal. Blood investigation revealed no abnormality. Ultrasonography of pelvis revealed normal uterus and ovaries with endo-echo 9 mm. Collection was seen in the upper part of vagina. A diagnosis of secondary vaginal atresia following traumatic vaginal delivery was made and the patient was planned for vaginoplasty using human amnion graft. Under anaesthesia, patient was placed in lithotomy position with legs on stirrups. An indwelling Foley’s catheter was placed under aseptic condition and perineal area was painted & draped. Transverse incision was given in the vagina to create a pocket between urinary bladder and rectum. Both the upper and lower lips were lifted up [Table/Fig-2]. About 300 ml of accumulated altered blood was drained out. Cervix was visualized and dilated with size 8 Hegar’s dilator [Table/Fig-3]. The Amniotic membrane graft was taken and placed on the upper and lower vaginal wall [Table/Fig-4]. A soft vaginal mould made up of condom containing soft sponge was placed. On the 7th postoperative day, the mould was removed. Examination revealed that the graft was well taken up and there was no pressure necrosis or ulceration. A new mould was prepared, using soft sponge covered with condom and was advised to place it in the vagina throughout the day and night for six weeks and only at night in the next six weeks, except at the time of defecation and micturition. Follow up was uneventful and the couple had regular intercourse after three months. Contraception was advised and the couple preferred combined oral contraceptive pills. The couple was advised to refrain from pregnancy for one year.
Secondary vaginal atresia following traumatic vaginal delivery
Transverse incision given in the vagina to create a pocket between urinary bladder and rectum with both upper and lower lip lifted up
Cervix was visualized and dilated with size 8 Hegar’s dilator
Amniotic membrane graft taken and placed on upper and lower vaginal wall
Discussion
Vaginal atresia can be congenital or acquired. Females with vaginal atresia lack the lower portion of the vagina, but otherwise have normal external genitalia [1]. The incidence of congenital or primary vaginal atresia is 1 in 4000 to 5000 live female births [2]. Secondary vaginal atresia is relatively rare and the exact incidence has not been reported in literature [3]. It usually occurs secondary to badly managed vaginal delivery causing vaginal injuries and later scarring. Untrained female staffs (dais and Lady Health visitors {LHVs}) play a major role in the increasing incidence of these complications in our country. Neglected foreign bodies in the vagina following induced abortion, pelvic inflammatory disease and radiotherapy have also been documented to result in a similar abnormality [4].
The treatment of females with vaginal atresia is creation of a functional vagina which can be accomplished conservatively or surgically. The non-surgical method may be useful in certain cases of primary vaginal atresia, however, majority of patients require vaginal reconstruction. In congenital or primary vaginal atresia, conservative approach includes progressive invagination of the vaginal dimple to create a canal of adequate size by Frank’s (1938) graduated hard glass dilators which were used initially followed by Ingram’s (1981) dilators fixed to a bicycle seat mounted upon a stool. Currently, firm silicon dilators are available through several medical vendors [1]. A vagina may also be created with repeated coitus. Overall, vaginal dilatation techniques are successful in forming a functional vagina in as many as 90% of cases [5].
Surgical procedures are seen by many as an immediate solution for creation of a neovagina, and are the mainstay treatment for secondary vaginal atresia. The method used most commonly by gynecologists is the McIndoe vaginoplasty where a canal is created within the connective tissue between the bladder and rectum. A split-thickness skin graft obtained from the patient’s buttocks or thigh is then used to line the neovagina [1]. Modifications of the McIndoe procedure include the use of human amnion, sigmoid colon, ileum, caecum [6], pudendal thigh flaps [7] , fasciocutaneous flaps, gracilis myocutaneous flaps, labia minora flaps, flaps raised following tissue expansion of the labial pocket, peritoneum and bladder mucosa, amnion [8], the interceed absorbable adhesion barrier [1], autologous buccal mucosa [4] and recently artificial dermis and recombinant basic fibroblast growth factor [9] as neovaginal linings. Free skin grafts, peritoneal grafts, local skin flaps and bladder mucosal grafts may scar the patient. Bowel segments have the disadvantages of abdominal scarring and the possibility of bowel obstruction, secretions, unpleasant odour and mucosal ulceration.
The human amniotic membrane is a readily available, cost free and has been used as protective biologic dressing for wounds and burns [10]. There is no evidence of immune rejection when amnion is implanted subcutaneously as the amnion does not express HLA-A, B or DR antigens. Amnion has antimicrobial properties as it produces lysozyme, hence it decreases the chances of post operative wound infection. When an uncontaminated amniotic mesenchymal surface is applied to the raw surface of the dissected vaginal tunnel, it adheres firmly, protects the underlying granulation tissue and facilitates epithelialization. The human amniotic membrane is capable of complete metaplasia into mature squamous epithelium. These features make the amnion a perfect tissue graft for covering the artificially dissected vagina. Amnion is obtained aseptically and may be stored in normal saline at 4°C for 48 to 72 h. The amniotic membranes with meconium staining, suspected chorioamnionitis or premature rupture, patients with HIV, Hepatitis B and other transmissible infections should not be used for grafting [2].
The co-operation of the patient is essential in vaginoplasty and the most important step is to maintain the vaginal space during contraction period of wound healing by effective moulds/stents.
Conclusion
The incidence of extensive vaginal tears following neglected and traumatic vaginal deliveries should be prevented by discouraging home deliveries by untrained dais and encouraging institutional delivery equipped with well trained staffs and adequate facilities. The cases of secondary vaginal atresia need counselling of patient and her husband regarding the available treatment options and a team work including both gynaecologist and plastic surgeons. The use of amnion in vaginal reconstruction is a simple, practicable and easily available option to all the treating gynaecologists and surgeons.
[1]. Schorge JO, Schaffer JI, Halvorson LM, Hoffman BL, Bradshaw KD, Cunningham FG, Williams Gynaecology 2008 1st edNew YorkMcGraw Hill MedicalChapter 18, Anatomic disorders ; p. 415-16 [Google Scholar]
[2]. Zafar M, Saeed S, Kant B, Murtaza B, Dar MF, Khan NA, Use of amnion in vaginoplasty for vaginal atresiaJCPSP 2007 17(2):107-09. [Google Scholar]
[3]. Ruttgers H, Leucht W, Kubli F, Secondary vaginal atresia: a case reportAm J Obstet Gynecol 1982 143:595-96. [Google Scholar]
[4]. Lin WC, Chang CYY, Shen YY, Tsai HD, Use of autologous buccal mucosa for vaginoplasty: a study of eight casesHum Reprod 2003 18:604-07. [Google Scholar]
[5]. Croak AJ, Gebhart JB, Klingele CJ, Therapeutic strategies for vaginal Mullerian agenesisJ Reprod Med 2003 48:395 [Google Scholar]
[6]. Hensle TW, Reiley EA, Vaginal replacement in children and youngadultsJ Urol 1998 159:1035-8. [Google Scholar]
[7]. Ganatra MA, Ansari N, Pudendal thigh flap for congenital absence of vaginaJ Pak Med Assoc 2005 55:143-45. [Google Scholar]
[8]. Nisolle M, Donnez J, Vaginoplasty using amniotic membranes in cases of vaginal agenesis or after vaginectomyJ Gynecol Surg 1992 8:25-30. [Google Scholar]
[9]. Noguchi S, Nakatsuka M, Sugiyama Y, Chekir C, Kamada Y, Hiramatsu Y, Use of artificial dermis and recombinant basic fibroblast growth factor for creating a neovagina in a patient with Mayer-Rokitansky-Kuster-Hauser syndromeHum Reprod 2004 19:1629-32. [Google Scholar]
[10]. Simman R, Jackson I, Andrus L, Pre-fabricated buccal mucosa-lined flap in an animal model that could be used for vaginal reconstructionPlast Reconstr Surg 2002 109:1044-49. [Google Scholar]