Postmenopausal Huge Ovarian Leiomyoma: A Rare Presentation
Sasikala R.1, Rupavani K.2, Rekha R.3, Erli Amel Ivan4
1 Professor, Department of Obstetrics and Gynecology, Sri Manakula Vinayagar Medical College, Puducherry, Tamil Nadu, India.
2 Assistant Professor, Department of Obstetrics and Gynecology, Sri Manakula Vinayagar Medical College, Puducherry, Tamil Nadu, India.
3 Postgraduate Student, Department of Obstetrics and Gynecology, Sri Manakula Vinayagar Medical College, Puducherry, Tamil Nadu, India.
4 Professor, Department of Pathology, Sri Manakula Vinayagar Medical College, Puducherry, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rupavani, B2,Thiagaraja Apartments, Thanthai Periyar Nagar, Puducherry,-605005, Tamil Nadu, India.
Phone: 9003550554,
E-mail: obgrupa@gmail.com
Ovarian leiomyoma is one of the rare solid tumours of ovary, accounting for 0.5-1% of the benign tumours of the ovary. We report one such case which presented in a postmenopausal woman. The differential diagnosis includes ovarian fibroma, thecoma, cellular fibroma and sclerosing stromal tumour. Masson’s trichrome staining helps to distinguish fibrous and smooth muscle components of the lesion and confirms the diagnosis of ovarian leiomyoma. Hence, ovarian leiomyoma should be considered in the differential diagnosis of ovarian spindle cell tumours.
Ovarian leiomyoma, Masson’s trichrome stain, Solid tumour
Case Report
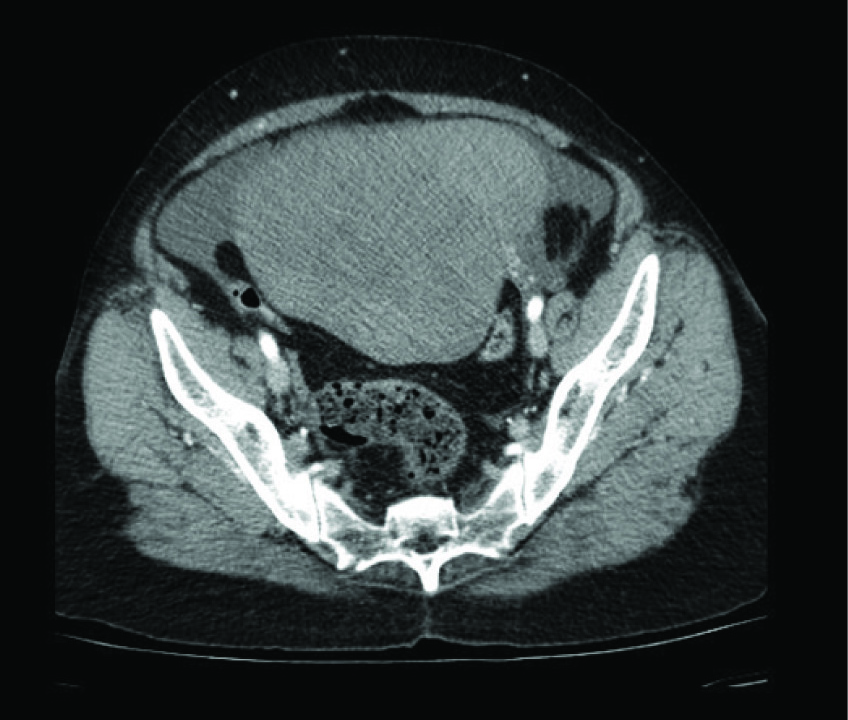
A 53-year-old lady, (P2, L2) who had attained menopause 10 y back, presented with history of abdominal distension for 1month which was associated with dull aching lower abdominal pain. She had no other systemic or menstrual complaints. She was moderately built and nourished and there was no evidence of any generalized lymphadenopathy on general examination. Blood pressure recorded was 150/100mm Hg. On per abdominal examination, an abdominopelvic mass was noticed, which was hard in consistency with regular borders of about 24 wk size. The mass was freely mobile side to side. On pelvic examination, uterus was atrophic in size and felt separately from the mass. CECT abdomen and pelvis [Table/Fig-1] revealed a heterogeneously attenuating mass lesion in abdominopelvic region of size 15.5 × 9.6 × 15.6cm. Uterus was 5.7 × 2.6 cm and seen separate from mass, with minimal ascites. No omental thickening or capsular penetration was noted. All these features were suggestive of left adnexal mass probably, ovarian fibroma.
CT scan picture showing the mass arising from the ovary
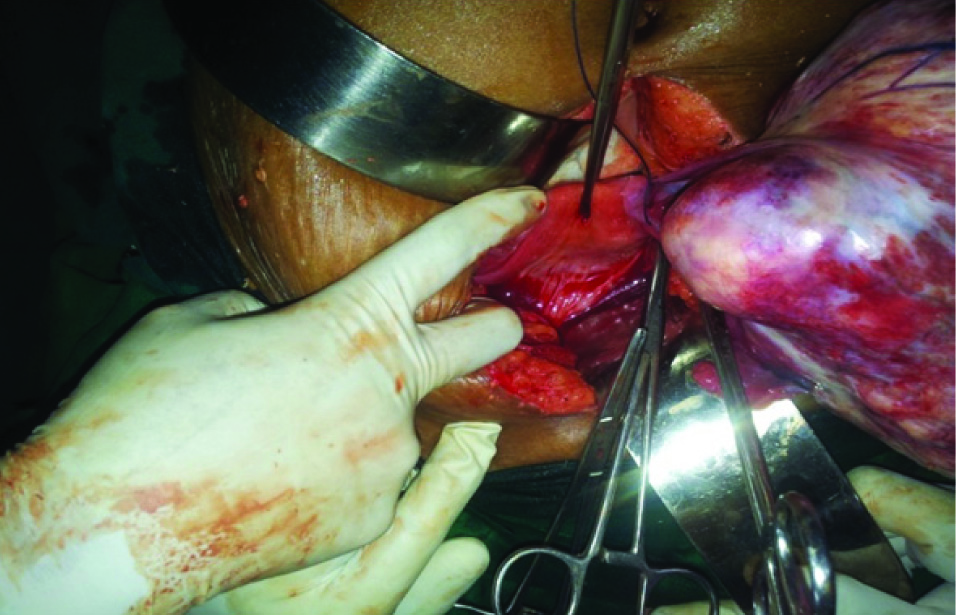
The preoperative workup showed hemoglobin 10g/dl, packed cell volume 31.0%, blood grouping and Rh typing B+ ve, BT 2′30′ and CT 3′30″, random blood sugar 90mg/dl, blood urea 24mg/dl, serum creatinine 0.7mg/dl, free T3 1.4pg/ml and T4 0.6ng/dl, TSH 11.6 mIU/ml, liver function test-total bilirubin 0.8 mg/dl, direct bilirubin 0.3 mg/Dl, SGOT 17 IU/L, SGPT 10 IU/L,alkaline phosphatase 98 IU/L,total protein 7.4 g/dl,albumin 4.2 g/dl,CA125:50 U/ML,ECHO-grade 1 diastolic dysfunction. After controlling her blood pressure and hypothyroid status, this patient was posted for laparotomy under combined spinal epidural anaesthesia. Intraoperatively, there was ascitic fluid of about 25 ml which was collected and sent for cytology which revealed no malignant cells. A pedunculated left ovarian mass measuring 16 × 12cm, solid in consistency was seen [Table/Fig-2 & 3]. There were no adhesions. The right ovary, bilateral tubes and uterus were unremarkable. The omentum appeared normal. Pelvic and para aortic nodes were not palpable. Total abdominal hysterectomy and bilateral salpingo-oophorectomy with omental biopsy was performed.
Uterus seen separately from the left ovarian mass
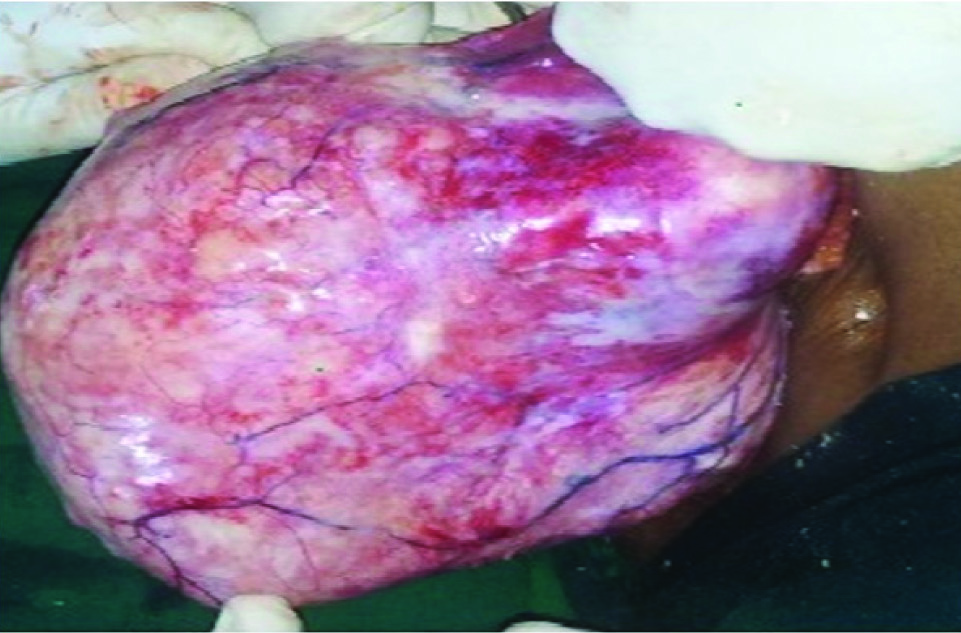
Gross appearance of the solid encapsulated ovarian leiomyoma
The ascitic fluid analysis showed high cellularity predominantly of reactive mesothelial cells arranged in clusters. Neutrophils, macro-phages and lymphocytes were seen. No cellular atypia was noted.
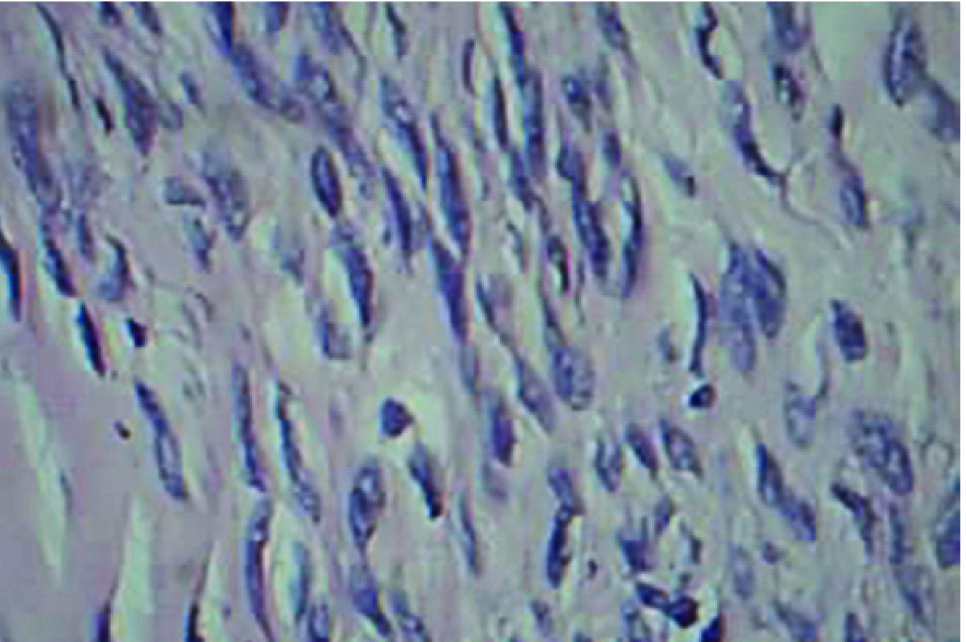
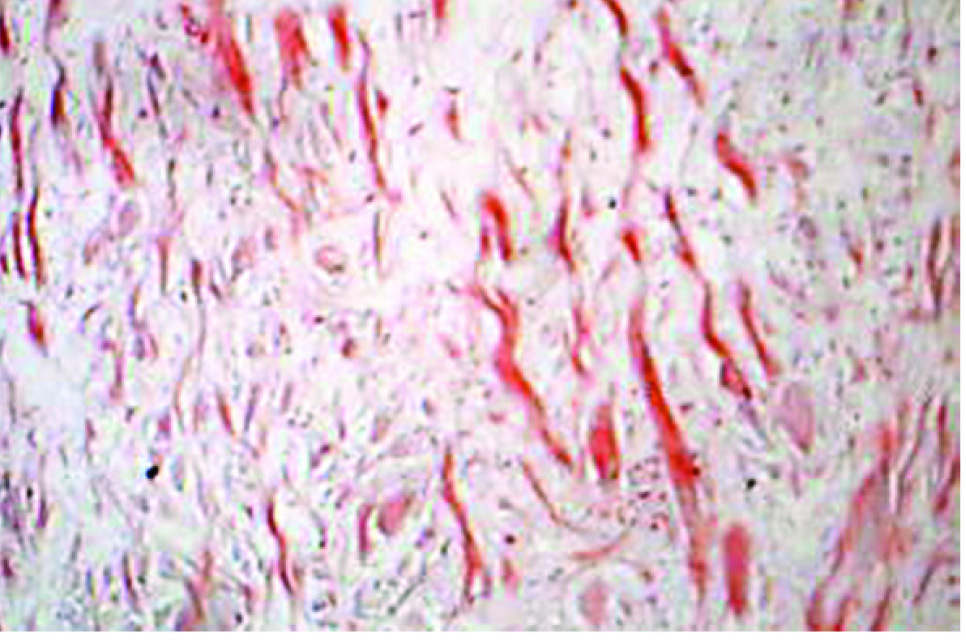
On gross examination, the ovarian mass was measuring 16 × 11 × 12 cm and the cut section of tumour showed hard grey white solid area which was well encapsulated. Microscopically, it showed well encapsulated benign tumour composed of fascicles and interlocking bundles of smooth muscles of fibres with blunt ended nuclei [Table/Fig-4a & b]. Large areas of sclerosis were seen. Thickened blood vessels with areas of haemorrhage were noticed. No cellular atypia was made out. Mitotic activity was sparse, 0-1/10 high-power field. Staining with masson’s trichrome stain showed positivity for smooth muscle fibres [Table/Fig-5]. The uterine endometrium showed senile cystic hyperplasia. Cervix, bilateral tubes and right ovary were unremarkable. Based on these findings, a diagnosis of ovarian leiomyoma was made out.
Microscopy view of ovarian leiomyoma after H &E stain showing tumour with leiomyoma cell with interspersed blood vessels (10x)
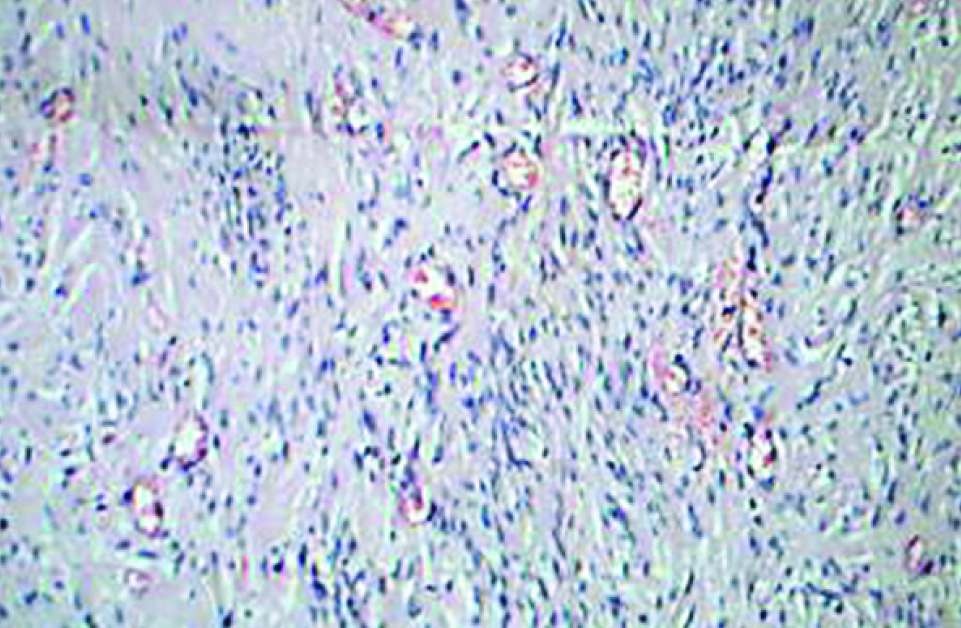
Microscopy view of ovarian leiomyoma after H &E stain showing spindle cell- intersecting bundles of smooth muscle cell(40x)
Masson’s trichrome staining showing positivity for smooth muscle cells(red)
Postoperatively, patient recovered well and she was discharged on the eighth postoperative day.
Discussion
Ovarian leiomyoma is one of the rare solid benign tumours of the ovary. Several theories have been proposed suggesting the origin of ovarian leiomyoma. Lerwil MF et al., suggested that it probably arises from the smooth muscle cells in ovarian hilar blood vessels. Other possible origins suggested include cells in ovarian ligament, smooth muscle cells or multipotential cells in ovarian stroma, undifferentiated germ cells, or cortical smooth muscle metaplasia [1]. Uterine leiomyoma was suggested to be associated with ovarian leiomyoma [2]. But, there was no other fibroid suggesting, the primary origin of the tumour from the ovary in this patient.
Most of the ovarian leiomyomas are asymptomatic and are often accidentally diagnosed during routine clinical examination or on ultrasound. But huge ovarian leiomyomas are often symptomatic. The symptoms described in the literature are variable. They may present with abdominal pain, weight gain, vomiting or meig’s like syndrome [2–5]. Some cases may present with hydronephrosis [6] or acute abdominal pain mimicking appendicitis [7].
The differential diagnosis for ovarian leiomyoma include ovarian fibroma, thecoma, cellular fibroma and sclerosing stromal tumour [8–10] As all these tumours exhibit similar type of clinical picture, histopathological examination plays an important role in the diagnosis. The correct diagnosis of ovarian leiomyoma requires the confirmation of smooth muscle component of the tumour. Masson’s trichrome staining helps to distinguish fibrous and smooth muscle components of the lesion [9,11,12]. and confirms the diagnosis of ovarian leiomyoma. Usually, ovarian leiomyomas have a benign course. Complete surgical resection is the treatment of choice [4].
Conclusion
Ovarian leiomyoma is a very rare solid tumour of the ovary. It should be considered in the differential diagnosis of ovarian spindle cell tumours. Appropriate muscle specific staining helps in correct diagnosis.
[1]. Lerwill MF, Sung R, Oliva E, Prat J, Young RH, Smooth muscle tumours of the ovary: a clinicopathologic study of 54 cases emphasizing prognostic criteria, histologic variants, and differential diagnosisAm J SurgPathol 2004 28(11):1436-51. [Google Scholar]
[2]. Kurai M, Shiozawa T, Noguchi H, Konishi I, Leiomyoma of the ovary presenting with Meigs’ syndromeJ ObstetGynaecol Res 2005 31(3):257-62. [Google Scholar]
[3]. Murakami M, Uehara H, Nishimura M, Iwasa T, Ikawa H, A huge ovarian smooth muscle tumour: a case reportJ Med Invest 2010 57(1-2):158-62. [Google Scholar]
[4]. Jena A, Lakshmi A, Patnayak R, Vijaylaxmi B, Primary ovarian leiomyoma: An uncommon entity – Case report and a brief review of literatureJournal of Basic and Clinical Reproductive Sciences 2013 2(1):54 [Google Scholar]
[5]. Azarpira N, Monabati A, Safaei A, Khanlari M, Large ovarian leiomyoma in a postmenopausal womanIndian Journal of Pathology and Microbiology 2011 54(2):413 [Google Scholar]
[6]. Khaffaf N, Khaffaf H, Wuketich S, Giant ovarian leiomyoma as a rare cause of acute abdomen and hydronephrosisObstetGynecol 1996 87:872-73. [Google Scholar]
[7]. Tomas D, Lenicek T, Tuckar N, Puljiz Z, Ledinsky M, Kruslin B, Primary ovarian leiomyoma associated with endometriotic cyst presenting with symptoms of acute appendicitis: A case reportDiagnPathol 2009 4:25 [Google Scholar]
[8]. Vierhout ME, Pijpers L, Tham MN, Chadha-Ajwani S, Leiomyoma of the ovaryActa Obstet Gynecol Scand 1990 69(5):445-47. [Google Scholar]
[9]. Erkaya S, Kutlay B, Uygur D, Kara F, Tezer A, Primary ovarian leiomyoma in a postmenopausal womanActaObstetGynecolScand 2000 79:79-87. [Google Scholar]
[10]. Lastarria D, Sachdev RK, Babury RA, Yu HM, Nuovo GJ, Immunohistochemical analysis for desmin in normal and neoplastic ovarian stromal tissueArch Pathol Lab Med 1990 114:502-05. [Google Scholar]
[11]. Matamala MF, Nogales FF, Aneiros J, Herraiz MA, Caracuel MD, Leiomyomas of the ovaryInt J GynecolPathol 1988 7:190-96. [Google Scholar]
[12]. Seidman JD, Russell P, Kurman RJ, Surface epithelial tumours of the ovary. In: Kurman RJ, editorBlaustein’s pathology of the female genital tract 2002 5th edNew YorkSpringer-Verlag:791-904. [Google Scholar]