Sarcoidosis Presenting as Isolated Gingival Enlargement: A Rare Case Entity
Pragya Tripathi1, Jaihans Aggarwal2, Deepak Chopra3, Sukhchain Bagga4, Kanika Sethi5
1Senior Lecturer, Department of Periodontology and Oral Implantology, Affiliated by- Chaudhary Charan Singh University, Inderprastha Dental College and Hospital, Ghaziabad, U.P., India.
2Professor, Department of Conservative Dentistry, Affiliated by- Chaudhary Charan Singh University, Inderprastha Dental College and Hospital, Ghaziabad, U.P., India.
3Professor, Department of Periodontology and Oral Implantology, Affiliated by- Chaudhary Charan Singh University, Inderprastha Dental College and Hospital, Ghaziabad, U.P., India.
4Reader, Department of Periodontology and Oral Implantology, Affiliated by- Chaudhary Charan Singh University, Inderprastha Dental College and Hospital, Ghaziabad, U.P., India.
5Senior Lecturer, Department of Oral Pathology, Affiliated by- Chaudhary Charan Singh University, Inderprastha Dental College and Hospital, Ghaziabad, U.P., India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Pragya Tripathi, Flat no 11, sector 5/119, Raj Nagar, Ghaziabad , (U.P) -201002, India. Phone : 91-9999977571,
E-mail: dr.pragya.trip@gmail.com
Sarcoidosis is a non-caseating granulomatous disease . It is a multiorgan inflammatory disorder of unknown etiology. Conditions affecting skin or other organs frequently involve oral cavity and rarely manifest as gingival disease. Here we are reporting a rare case in which gingival hyperplasia was the initial symptom which finally led to the diagnosis of sarcoidosis. Oral mucous membrane needs to be examined carefully as it may constitute in presenting first sign of systemic sarcoidosis.
Granulomatous lesion, Isolated gingival enlargement, Non-caseating granuloma
Case Report
A 42-year-old male patient reported with a chief complaint of intraoral localized painless swelling on the gums at the upper front region with one month duration. There was no history of trauma, infection, allergy, endocrine abnormality and intake of drugs. Family history of similar swelling was noncontributory.
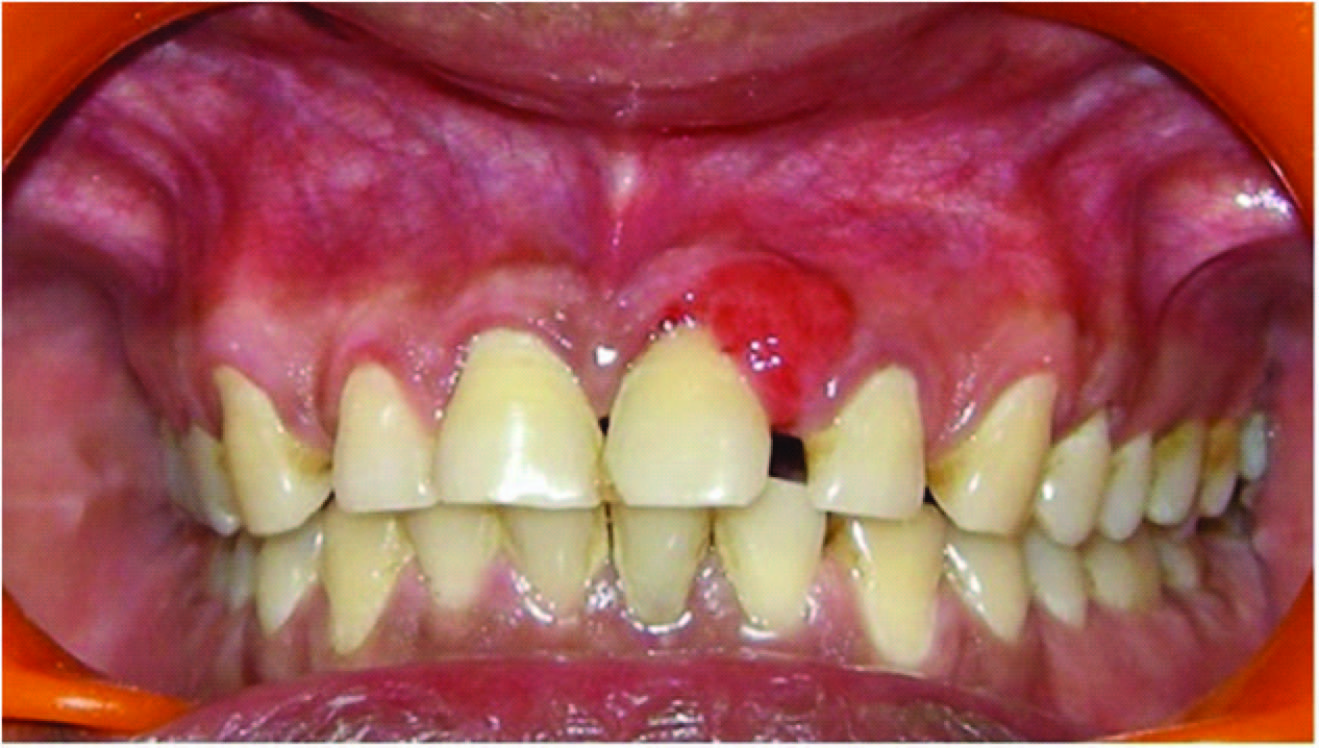
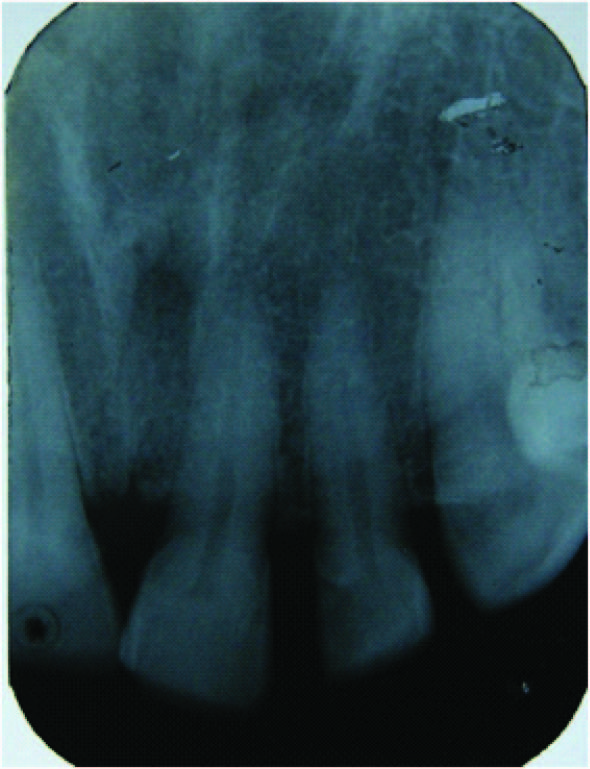
No abnormality was detected on extraoral examination and lymphnodes were not palpable. Intra oral examination showed a well demarcated round, soft, sessile, non-tender, non-ulcerated reddish pink swelling on the left side of maxillary anterior gingiva measuring 1 x 1 cm in diameter [Table/Fig-1]. There was no history of tobacco, beetel nut chewing or smoking reported by the patient. Oral hygiene status was good and no carious lesions and subgingival deposits were identified. IOPA x-ray was done which revealed no abnormal finding [Table/Fig-2].
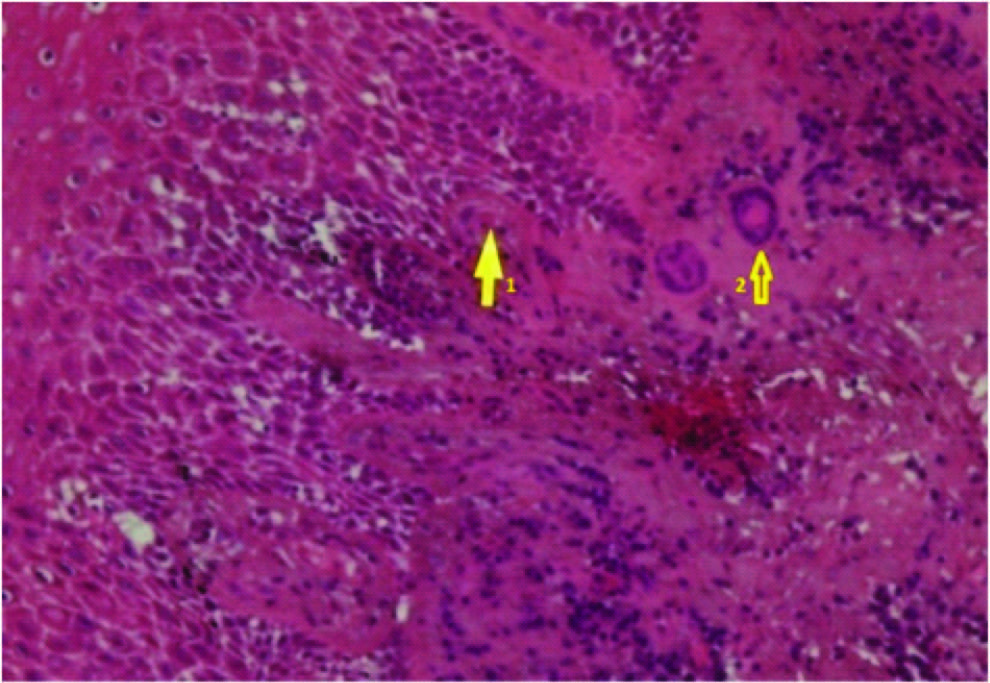
Treatment consisted of oral prophylaxis and excisional biopsy of the gingiva [Table/Fig-3] from maxillary right anterior region and tissue was sent for histopathologic assessment .Microscopic examination of the biopsy sample revealed focal aggregates of chronic inflammatory cells mainly plasma cells, lymphocytes, eosinophils and multinucleated giant cells admixed with fibrous stroma giving the appearance of non- caseating granuloma with an overlying spongiotic parakeratinized stratified squamous epithelium [Table/Fig-4]. All these were suggestive of a granulomatous lesion.
Differential diagnosis of granulomatous lesion include systemic diseases such as Sarcoidosis, Crohn’s disease, tuberculosis as well as lesions localized to the orofacial region such as Orofacial granulomatosis.
Based on these findings complete haemogram, Montoux test and PCR for M.tuberculosis on tissue sample was advised. Haemogram was within normal limits. Mountoux and PCR was reported negative.
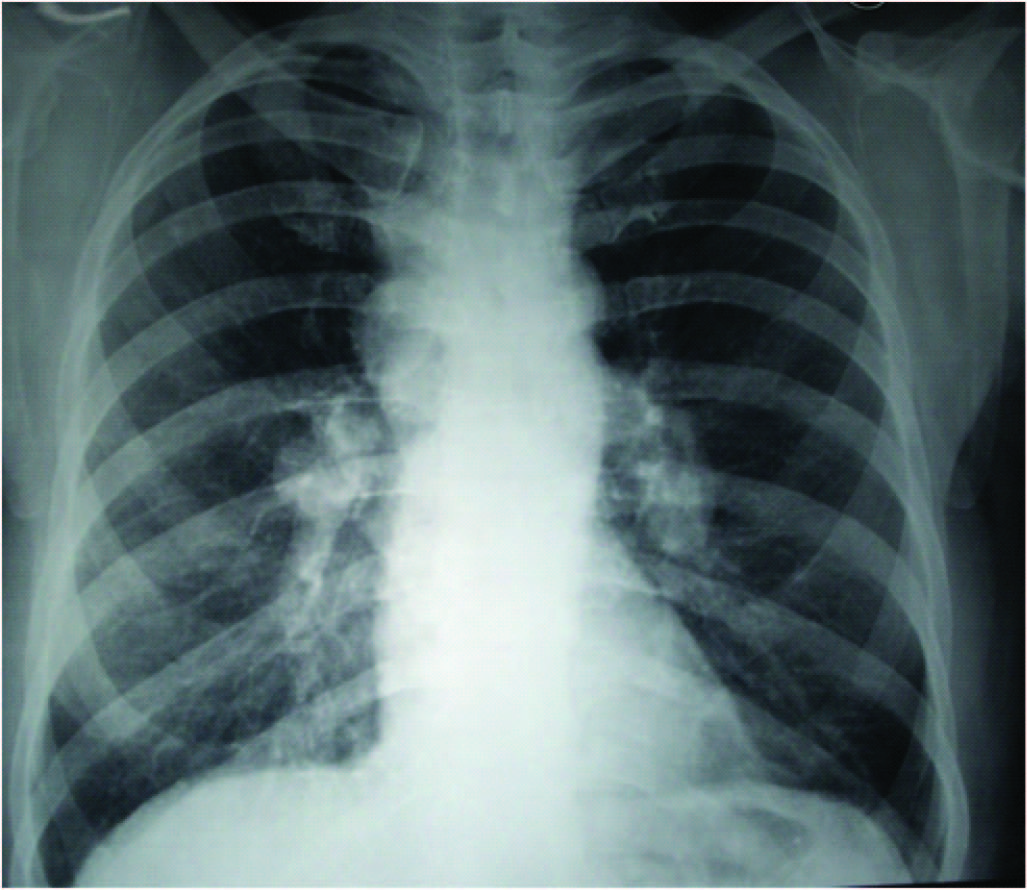
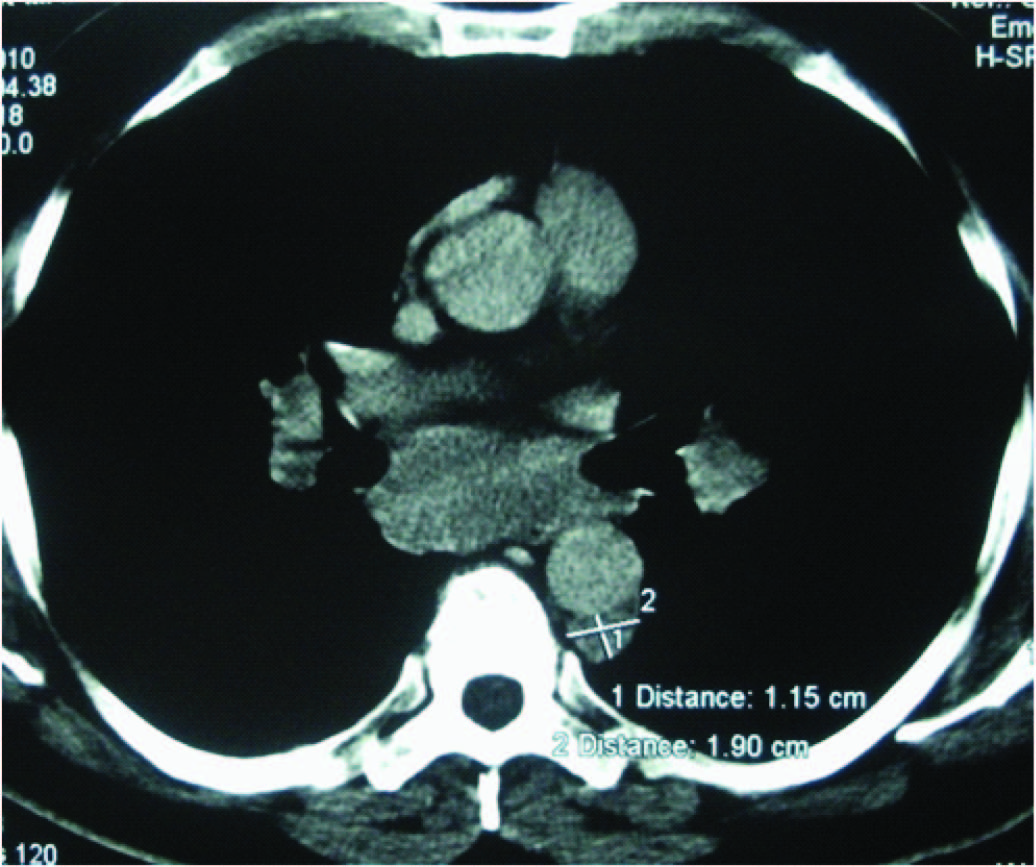
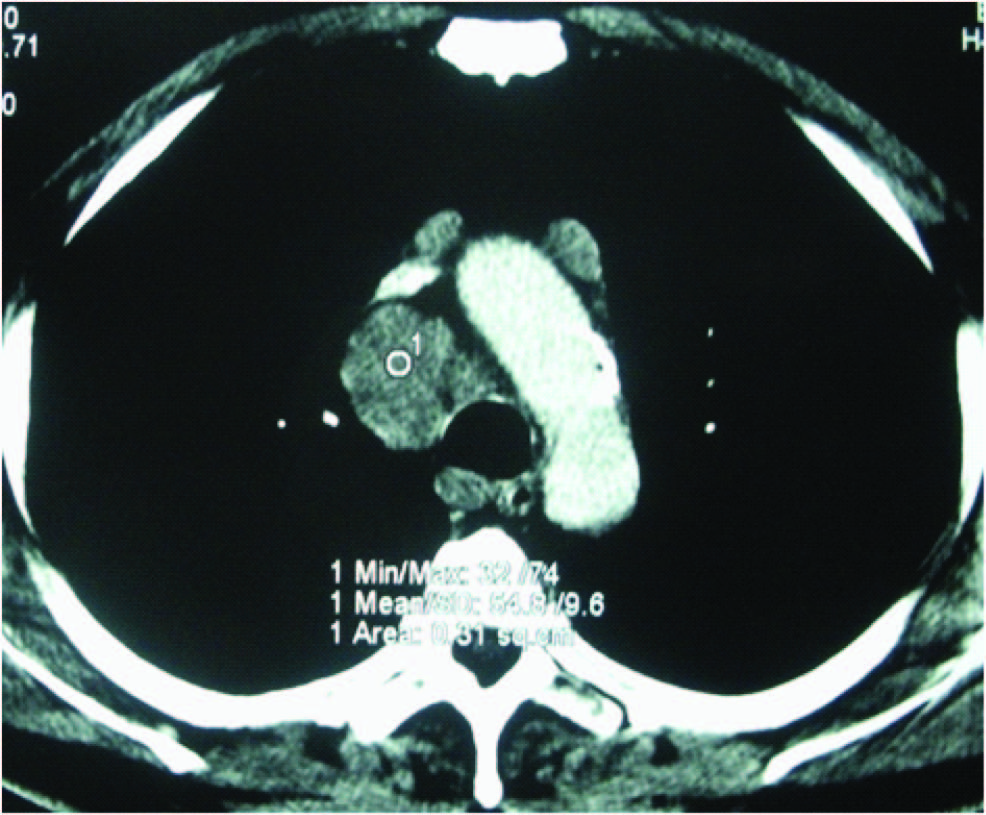
Patient was referred to general physician for further investigations. Montoux, complete haemogram were repeated and serum angiotensin converting enzyme (S-ACE) blood test were organized. Again Montouxtest was negative while S-ACE levels were elevated above the normal (83u/L). Further investigations included a chest X-ray and CT scan. Chest X-ray showed lymphadenopathy [Table/Fig-5] which was further confirmed by chest CT scan.
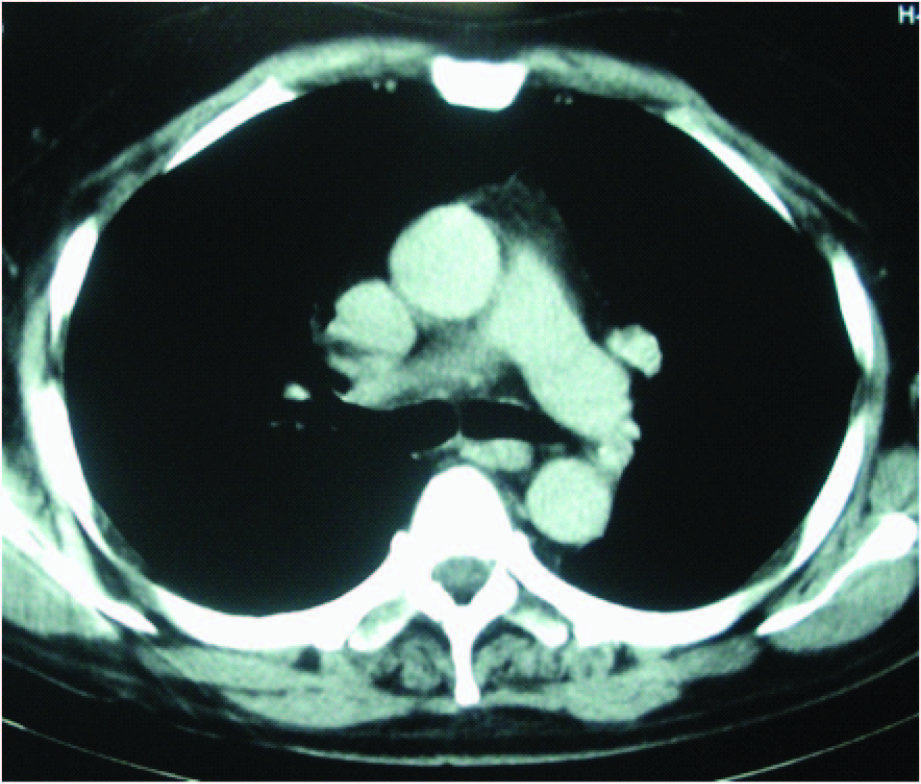
CT scan of chest showed lymphadenopathy in subcarinal (4x3), pretracheal (3cm) and tracheobronchial nodes (3cm) with bilateral hilar lymph nodes enlargement (2cm) whereas lungs appeared to be normal [Table/Fig-6,7].
On the basis of CT findings, Endoobronchial ultrasound (EBUS) with transbronchial needle aspiration was advised by the physician and collected sample was sent for histopathological examination.
Collective Interpretation of the imaging (CT Scan) in conjunction with the clinical information, haematological, biochemical investigations, and histopathology ruled out tuberculosis and confirmed the diagnosis of sarcoidosis.
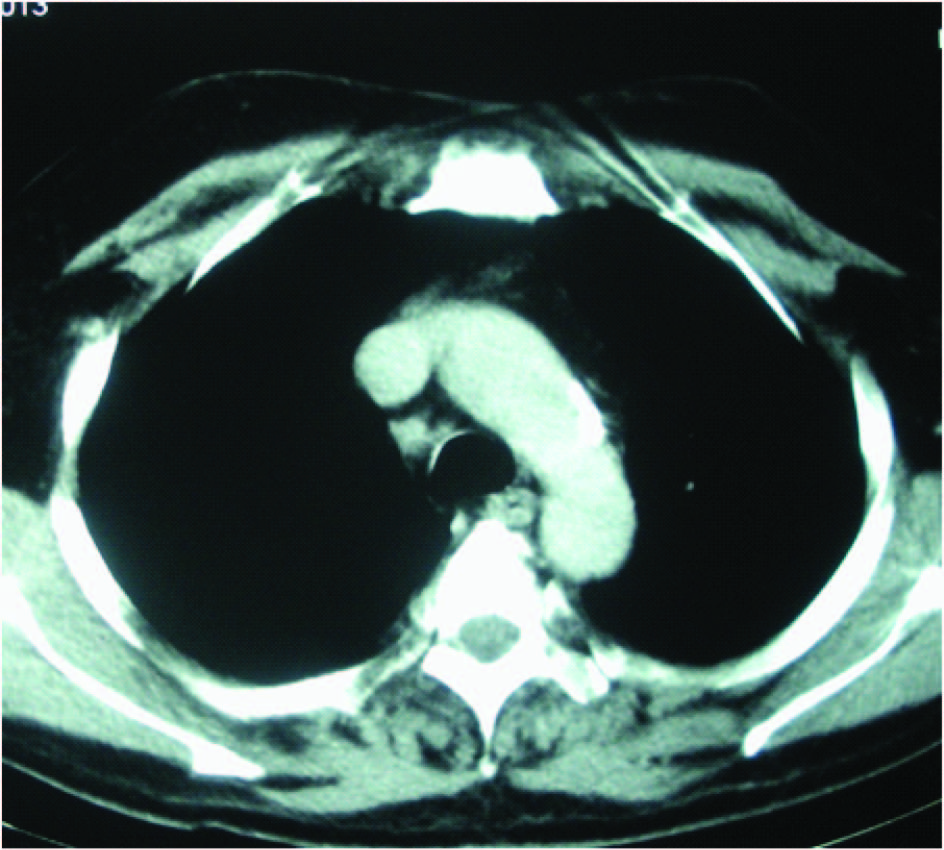
Patient underwent systemic steroidal therapy for the management of sarcoidosis as prescribed by the physician. Regular follow up showed marked improvement which was confirmed by repeat CT scan after one year [Table/Fig-8,9]. S-ACE level was in the normal limits and CT scan revealed decreasein size of lymph nodes. Clinical examination on one year follow up showed normal gingiva without any sign of recurrence [Table/Fig-10].
Discussion
Sarcoidosis is a granulomatous disorder that is characterized by non caeseating granuloma that may affect any organ [1]. Head and neck lesions of sarcoidosis are manifested in 10 to 15% of patients [2,3]. Oral involvement of sarcoidosis is relatively rare and usually the buccal mucosa, lips, gingivae, tongue and palate are the affected sites [1,4]. Oral manifestation of sarcoidosis has been described and includes multiple nodular painless indistinct ulceration of gingiva, buccal mucosa, labial mucosa and palate [5]. This case reports an unusual and uncommon presentation of sarcoidosis. In this case gingival swelling presentation was distinct isolated, diffuse and painless.
The diagnosis of sarcoidosis is established when clinical features as well as chest X-ray are supported by histopathological evidence of typical non-caseating epithelioid granuloma and exclusion of other non-caseating granulomas [6,7] by taking the patients history of weight loss, bowel discomfort and other systemic symptoms to exclude other non caseating granulomas such as Crohns disease and Orofacial granulomatosis.
The majority of cases of sarcoidosis have lung involvement (90%) in the form of pulmonary infiltration and involvement of thoracic lymph nodes [8]. Medical and radiographical examination usually reveals pulmonary hypofunction and chest X-ray shows typical bilateral hilar lymphadenopathy. Hematological and biochemical tests may show elevated lymphocytopenia, increased liver enzymes, hypercalcemia and increased serum angiotensin enzyme (S-ACE) [1,9]. S-ACE is positive in 80% cases of sarcoidosis [9,10]. Histopathological examination shows the typical non-caseating granulomas which contain epitheloid macrophages surrounded by lymphocytes and presence of Multinucleated giant cells .
Endobronchial ultrasound (EBUS) with transbronchial needle aspiration is reliable tool for diagnosis of sarcoidosis or tuberculoosis with intrathoracic lymphadenopathy [11,12].
In this case EBUS played a significant role in exclusion of tuberculous lesion and confirmation of sarcoidosis.
Sarcoidosis of gingiva as a primary or initial lesion must be considered highly unusual as there are relatively few reports of gingival sarcoidosis. Thus the treatment of sarcoidosis is indivisualised based on severity of disease and symptoms [13]. Accurate diagnosis of sarcoidosis is a challenge to clinician. This disease is a disease of uncertainity in terms of its cause presentation and clinical course.
IOPA-X-ray (preoperative)

Histopathological view depicting a dense population of chronic inflammatory cells, separated by a fibrous septa. Mainly the plasma cells, lymphocytes and eosinophils (1) with presence of multinucleate giant (2) cells are seen. Connective tissue is highly fibrous in nature (High power magnification)
Postoperative 1 year after healing

Conclusion
Early diagnosis is a crucial step to prevent and cure unsightly sequelae and sometimes avoid progression of systemic potentially life-threatening sarcoid-related diseases. Considering the variable clinical onset of sarcoidosis, a dentist, may be a first consulted health care professional and hence plays an important role in detecting a disorder.
[1]. L Suresh, L Radfar, Oral sarcoidosis: a review of literatureOral Dis 2005 11(3):138-45. [Google Scholar]
[2]. AV Samtsov, Cutaneous sarcoidosisInt J Dermatol 1992 117:203-07. [Google Scholar]
[3]. LS Newman, CS Rose, LA Maier, EH Kass, SarcoidosisgN Engl J Med 1997 336:1224-35. [Google Scholar]
[4]. A Kasamatsu, H Kanazawa, T Watanabe, O Matsuzaki, Oral sarcoidosis: report of a case and review of literatureJ Oral Maxillofac Surg 2007 65(6):1256-59. [Google Scholar]
[5]. Jr Greer RO, RJ Sanger, Primary intraoral sarcoidosisJ Oral Surgery 1977 35(6):507-09. [Google Scholar]
[6]. I Marie, A Proux, H Levesque, S Bony-Rerolle, P Chenal, Tongue involvement Revealing sarcoidosisQJM 2008 101(11):909-11. [Google Scholar]
[7]. J Müller-Quernheim, Serum markers for the staging of disease activity of sarcoidosis and other interstitial lung diseases of unknown etiologySarcoidosis Vasc Diffuse Lung Dis 1998 15(1):22-37. [Google Scholar]
[8]. E Fernández Fabrellas, Epidemiology of sarcoidosisArch Bronconeumol 2007 43(2):92-100. [Google Scholar]
[9]. III English JC, PJ Patel, KE Greer, SarcoidosisJ Am Acad Dermatol 2001 44(5):725-43. [Google Scholar]
[10]. CW Turton, E Grundy, G Firth, D Mitchell, BG Rigden, M Turner-Warwick, Value of measuring serum angiotensin I converting enzyme and serum lysozyme in the management of sarcoidosisThorax 1979 34(1):57-62. [Google Scholar]
[11]. G Hong, KJ Lee, K Jeon, WJ koh, GY Suh, Usefullness of Endobronchial ultrasound guided transbronchial needle aspiration for diagnosis of sarcoidoosisYonsei Medical journal 2013 54(6):1416-21. [Google Scholar]
[12]. N Navani, PL Molyneaux, RA Breeen, DW Conneell, A Jepson, Utility of Endoobronchial ultrasound guided transbronchial needle aspiration in patients with Tuberculous intra thoracic lymphadenopathy: A multicenter studyThorax 2011 66(10):889-93. [Google Scholar]
[13]. MM Ali, AA Atwan, ML Gonzalaz, Cutaneous sarcoidosis:Updates in the pathogenesisJ Euro Dermatol and Venereol 2010 24(7):247-55. [Google Scholar]