Orbito-Rhino-Antro Access Osteotomy For Anterior Skull Base Lesions
Sumanth K Sreeramaneni1, Vivekanand. S Kattimani2
1 Reader, Department of Oral and Maxillofacial Surgery, SIBAR institute Of Dental Sciences, Guntur, AP, India.
2 Assistant Professor, Department of Oral and Maxillofacial Surgery, SIBAR Institute Of Dental Sciences, Guntur, AP, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vivekanand S. kattimani, Assistant Professor, Department of Oral and Maxillofacial Surgery, SIBAR institute of Dental Sciences, Guntur-522509, AP, India. Phone : 9912400988, E-mail : drvivekanandsk@gamil.com
Even with advent of endoscopic assisted surgeries the access osteotomy plays an important role for accessing the pathological lesions of anterior skull base since beginning of the era of surgery. This report introduces the orbito–rhino–antral access osteotomy for the removal of juvenile nasio angio fiboma extending in to the cranial base. This osteotomy provides good access to the lesion with lesser morbidity and without hampering the occlusion as in lefort osteotomies. It is safe, easy and faster to perform. Osteotomised segment is easy to replace and gives ease for the surgeon to access without any hindrance. The osteotomised segment act as free graft and there are no complications postoperatively even after 48 mnth of follow-up.
Access osteotomy, Anterior skull base lesions, Nasio angio fibroma, Nasal pathology, Orbito-rhino-antro osteotomy
Case Report
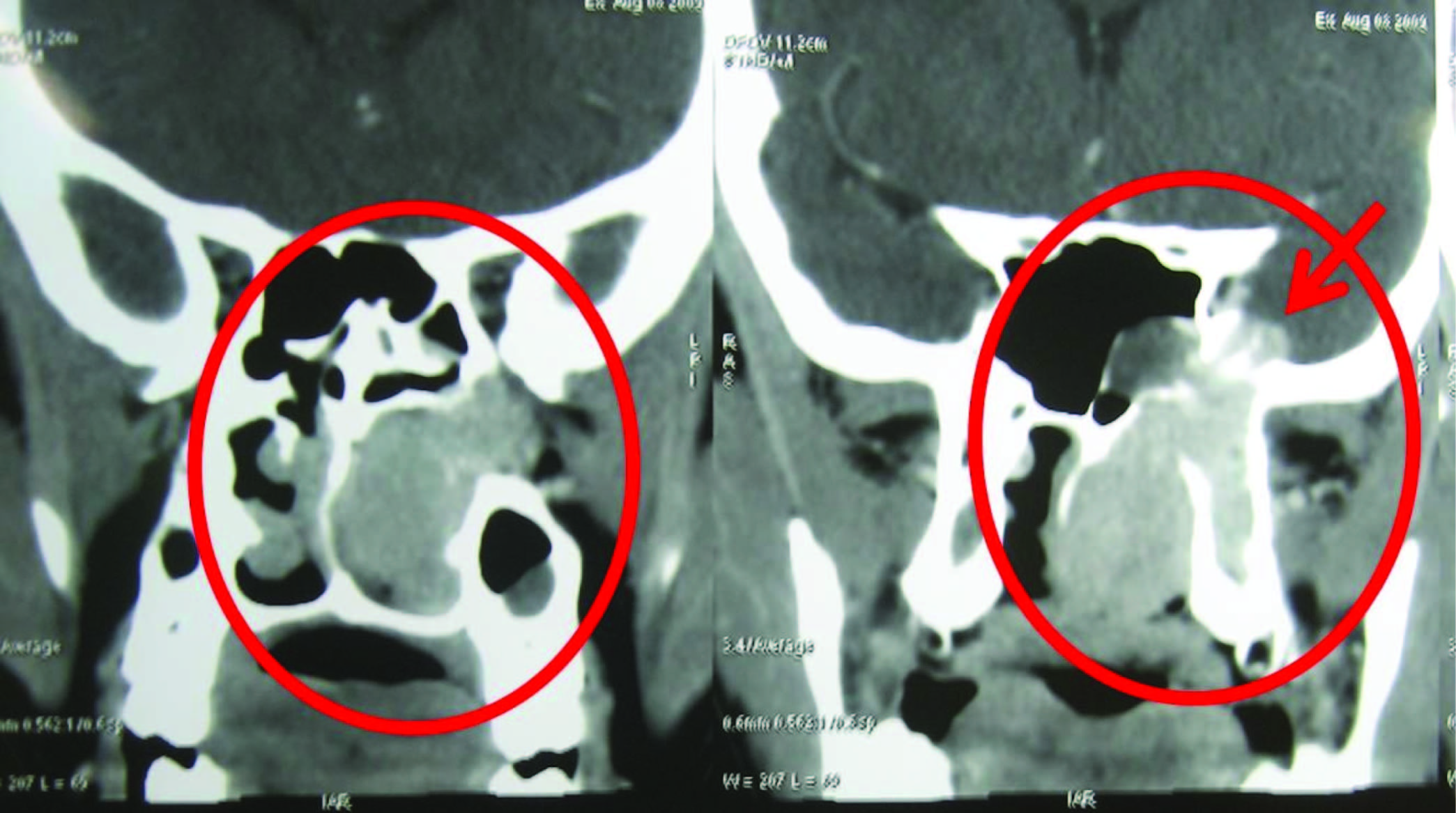
A 14-year-old moderately built and moderately nourished boy presented with complaints of blocked left side nose since 9-10 months and occasional epistaxis since 3 months. Diagnosis of nasioangiofibroma involving the entire left maxillary sinus, nasopharynx and which is extending superiorly to the interorbital space was made [Table/Fig-1] after thorough radiological (i.e. contrast enhanced CT) and histopathological examination (of biopsied lesion). Three months prior to his visit, the patient had undergone an attempt for excision of the tumour (mistaken as an antrochoanal polyp) through an endoscopic approach, which had to be aborted because of haemorrhage. The Surgery was undertaken after the necessary preoperative investigations and consent. The surgical strategy of separating the osseous walls from the tumour, and then in turn separating the tumour from its tenuous attachments, was achieved by the orbito-rhino-antral access osteotomy. Since the infra orbital extension came within easy reach. The main bulk of the tumour was removed by displacing downwards towards the space created by orbito-rhino-antral access osteotomy. Since the tumour could be excised with its capsule intact, the overall blood loss was very less. The fragment repositioned and fixed with miniplates, thereby accurately repositioning the osteotomised segment. Clearance of the tumour was complete. The patient has made good progress [Table/Fig-2] and followed up over period of four years. This report describes the orbito-rhino-antral modified access osteotomy approach for the management of extensive anterior skull base lesions, and provided the rationale for expanding the clinical experience.
Coronal section of CT showing extension of lesion
Three days post-surgery photo showing healing wound with suture in line

Current Surgical Technique
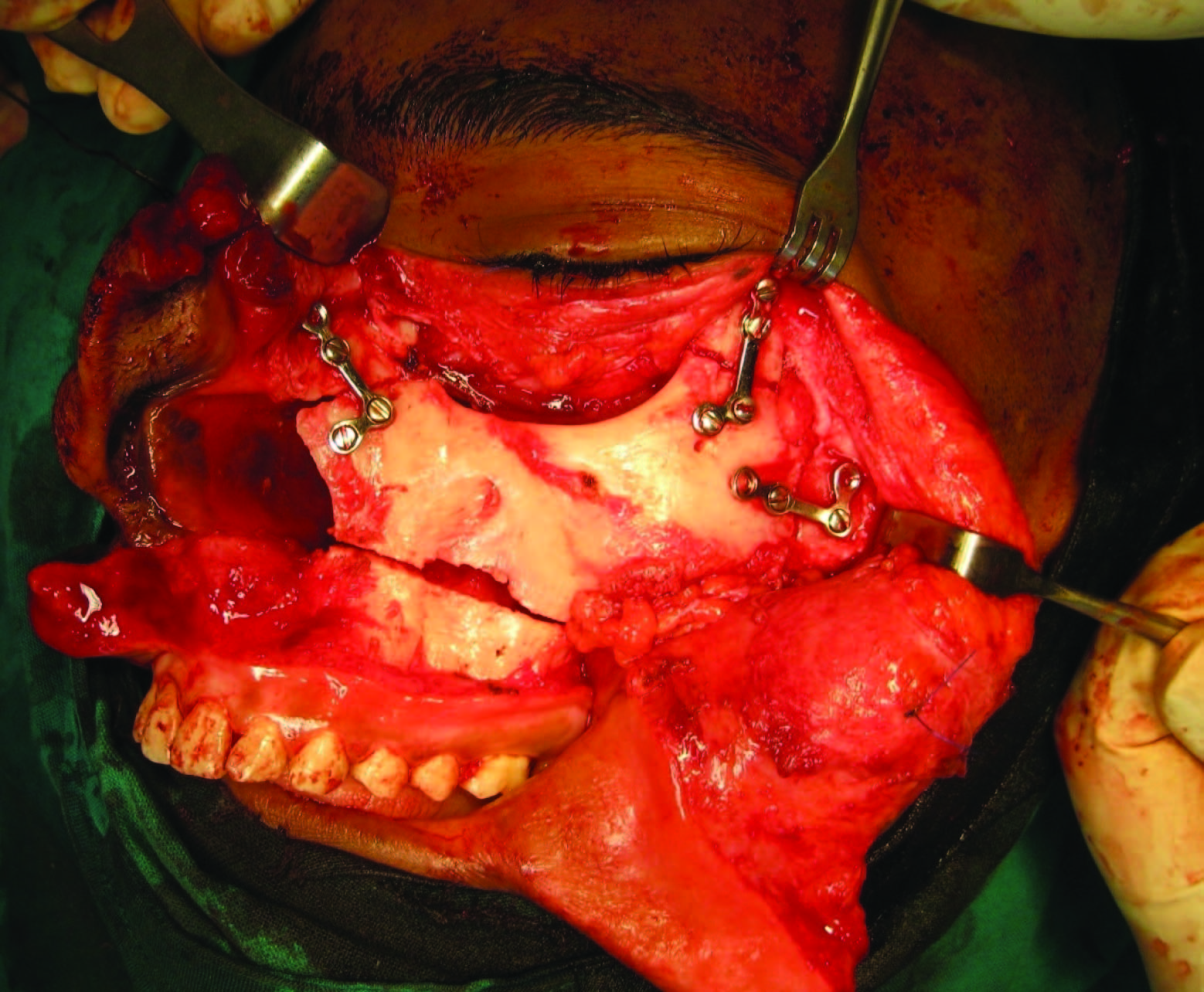
Orbito rhino-antral osteotomy for maxillary removal and reinsertion for anterior cranial base tumours is performed by maxillofacial surgeon in conjunction with team including ENT surgeon and neurosurgeon. Initially, oral intubation was done on the other side. Maxillo-facial surgeon subsequently performed an extended facial degloving through lip split extended Weber Ferguson incision to allow exposure of the midface [Table/Fig-3a&b]. Stainless-steel miniplates were shaped before bone cuts were made. We used L-shaped miniplates for fixing (1.5-mm screw diameter) the orbital osteotomy and maxillary osteotomy sites. Cuts were made so that the piriform aperture lateral margins were included as a rigid base for the transposed maxilla, which also widens the area of exposure. The lateral nasal osteotomy cuts were made at right angles to the bone surface of the frontal process of the maxilla, in order to minimize the risk of damage to the nasolacrimal apparatus or displacement of the medial canthal ligament. Further osteotomy cuts, to permit the mobilization of the anterior wall of the maxillary sinus and part of the inferior orbital rim were made. The orbital rim was transected and the cut was continued along the floor of the orbit to the lateral margin, where a vertical cut was made over the zygomatic bone. An unilateral Lefort- I level horizontal cut was made, which communicates with both the lateral nasal as well as the vertical cut over the zygomatic bone. The orbital floor osteotomy was joined medially to the lateral nasal osteotomy, taking care not to damage the coronal plane. The entire segment was mobilized. The infraorbital nerve bundle was incised when the rim is partially separated. Further exposure and additional space for the delivery of the lesion was obtained by extending the cuts already made into a standard or unilateral Le Fort I osteotomy. This procedure provides an access to the entire central and lateral aspects of the anterior skull base [Table/Fig-4]. It is also possible to move the orbito-maxillary components separately. The incision can also be extended over the frontal region if a frontal craniotomy is required for access to the anterior fossa.
Intraoperative photograph showing line of incision

Intraoperative Photograph showing exposure for osteotomy

Intra operative Photograph showing access osteotomy.,

The osteotomies allowed removal of the maxillary bone, providing wide exposure to the anterior cranial base. The tumour was then resected with the intracranial disease [Table/Fig-5]. The maxillary bone segment was replaced into normal anatomic position and rigidly fixated using the previously contoured craniofacial miniplates [Table/Fig-6]. The maxillary osteotomies can also be modified to include a larger portion or all of the malar bone to provide lateral exposure. We have not involved nasal septum to decrease postoperative nasal crusting.
Photograph of excised tumour mass

Intra operative photo showing fixed osteotomised segment with miniplates
Discussion
Varieties of benign and malignant lesions are found at the anterior skull base. These lesions are often difficult to visualize owing to their location. This difficulty in visualization contributes to the delayed diagnosis and the presence of extensive disease at the time of treatment. Advances in cranial base surgical techniques provide improved access for complete resection of clinically detectable lesions [1–4]. However, these surgical procedures can create functional and/or cosmetic deformities. The challenge of creating an adequate surgical access, with minimal postoperative morbidity remains the main goal. Approaches to the anterior skull base can involve the resection of a portion of the midface, primarily to provide access to the lesion [5]. Those anatomic structures directly involved with the malignant neoplasms need to be resected. However, some surgical approaches have been described in the literature to access the anterior skull base which includes resecting of the noninvolved mid-facial bones solely to provide access [6–12]. Transposition of the nose greatly facilitates access to the anterior cranial base. The "swinging" nasofrontal bone flap for gaining access to the anterior skull base tumours described by Panje WR et al., [6] is useful in the management of isolated anterior skull base tumours; with paranasal sinus involvement and extension into the pterygoid region which necessitates a greater exposure. The transfacial lateral rotation technique as described by Altemir FH [7], gives good access to the retromaxillary area but is inadequate if the inter orbital area has to be approached. An alternative approach involving maxillary removal to allow resection of the lesion with immediate reinsertion of the maxillary bone graft has been previously described by Schuller et al., [8] and has been used for a variety of lesions since 1990.
The ability of surgeons to resect lesions of the anterior skull base continues to improve owing to better imaging and surgical techniques. With some techniques, obtaining surgical access to the anterior skull base often involves resecting portions of the bony midface, which provides exposure to the lesion [6–12], but may also create permanent functional and cosmetic deformities. Trans facial osteotomy [6] has three main limitations with regard to extensive lesions. Firstly, since the nose is not transposed, no access to inter orbital region is possible. Secondly, in the case of tumours involving both the nasopharynx and the paranasal sinuses, the lateral mobilization of the maxillary segment inevitably results in disruption of the tumour margins. Thirdly, the access to the retromaxillary region is through the maxillary sinus, therefore, the pterygoid region can be visualized only after the maxillary antral space is cleared of the tumour. Lateral rhinotomy approach, is impossible in the case of extensive lesions to remove the base of the tumour [8]. Transpalatal, transzygomatic, transcervical and even transmandibular approaches have, therefore, also been suggested [9,10]. Orbito rhino-antral osteotomy provides maxillary removal and reinsertion as an alternative surgical technique that provides adequate exposure to the extra cranial component of the disease which can be combined with a midline mandibular osteotomy to provide exposure from the anterior cranial fossa superiorly and paraesophageal space inferiorly. It is possible to modify the described technique in several ways. The nose alone can be translocated in case of smaller lesions, or transposed to the opposite side to which the orbitomaxillary segment is moved [9]. It limits the potential for postoperative morbidity by preserving the maxillary fragment that provides the functional support to the orbital contents and the aesthetic benefit of preserving the entire orbital rim and malar bone [9]. This type of osteotomy not involves occlusion like our technique [8,10]. The preservation of nasal septum prevents postoperative nasal deviation and crusting. Our surgical procedure provides excellent exposure to the skull base, but reinsertion of the maxillary segment essentially represents a free bone graft [8,10]. This is a possible source of complication [8,10]; but evaluation of the patient who underwent Orbito rhino-antral access osteotomy revealed no complications even after more than 48 months of follow-up.
Conclusion
Orbito-rhino antral osteotomy technique for maxillary removal and reinsertion provides excellent visualization and access to the anterior skull base. There are no major complications observed. This procedure represents a method to decrease operative morbidity by preserving function and aesthetics, while allowing excellent surgical access to the skull base lesions.
[1]. Schuller DE, Hart MC, Goodman JH, The surgery of benign and malignant neoplasms adjacent to or involving the skull baseAm J Otolaryngol 1989 10:305-13. [Google Scholar]
[2]. Schuller DE, Goodman JH, Miller CA, Reconstruction of the skull baseLaryngoscope 1984 94:1359-64. [Google Scholar]
[3]. Schuller DE, Goodman JH, Mountain RE, Brown BL, Frank JE, Ervin-Miller KJ, Adjunctive treatment of cranial base malignanciesJ Craniofac Surg 1995 6:69-74. [Google Scholar]
[4]. Janecka IP, Sen CN, Sekhar LN, Arriaga M, Facial translocation: a new approach to the cranial baseOtolaryngol Head Neck Surg 1990 103:413-19. [Google Scholar]
[5]. Sisson GA, Bytell DE, Becker SP, Ruge D, Carcinoma of the paranasal sinuses and cranial-facial resectionJ Laryngol Otol 1976 90:59-68. [Google Scholar]
[6]. Panje WR, Dohrmann GJ, Pitcock JK, The transfacial approach for combined anterior craniofacial tumour ablationArch Otolaryngol Head Neck Surg 1989 115:301-07. [Google Scholar]
[7]. Hernández Altemir F, Transfacial access to the retromaxillary areaJ Maxillofac Surg 1986 14:165-70. [Google Scholar]
[8]. Schuller DE, Goodman JH, Brown BL, Frank JE, Ervin-Miller KJ, Maxillary removal and reinsertion for improved access to anterior cranial base tumoursLaryngoscope 1992 102:203-12. [Google Scholar]
[9]. Maniglia AJ, Phillips DA, Midfacial degloving for the management of nasal, sinus, and skull-base neoplasmsOtolaryngol Clin North Am 1995 28:1127-43. [Google Scholar]
[10]. Sharma P K, Schuller DE, Goodman JH, Smith SP, Goldman FP, Raj S, Nicholson RE, Young DC, Maxillary Removal and Reinsertion for Anterior Cranial Base Tumours: long term resultsArch Otolaryngol Head Neck Surg 1998 124:149-52. [Google Scholar]
[11]. Salins PC, The trans naso-orbito-maxillary approach to the anterior and middle skull baseInt. J. Oral Maxillofac. Surg 1998 27:53-57. [Google Scholar]
[12]. Grime PD, Haskell R, Robertson I, Gullan R, Transfacial access for neurosurgical procedures: an extended role for the maxillofacial surgeon. 1. The upper cervical spine and clivusInt J Oral Maxillofac Surg 1991 20:285-90. [Google Scholar]