A case of Chronic Bilateral Axillary Hidradenitis
Anji Reddy Kallam1
1 Director & Plastic Surgeon, Department of Plastic Surgery, Asram Medical College, Eluru Wt. Godavri, Andhra Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. K. Anji Reddy, Plastic Surgery Director, ASRAM Medical College, Eluru,Wt. Godavari-534005, Andhra Pradesh, India. Phone : 9652570679, E-mail : reddykanji@gmail.com, anjireddy_asram@yahoo.com
Apocrine sweat glands-Chronic hidradenitissuppurativa-axillae
Case Report
A male patient 44-year-old was referred in plastic surgery department of our hospital in January 2014 with history of chronic, discharging, multiple, communicating sinuses with surrounding pigmentation associated with fibrosis in both axillae [Table/Fig-1,2] and perineal region [Table/Fig-3]. He had restricted axillary movements and was unable to attend his normal work over the last four year. The chronology of events is as follows:



During 2010 October he developed solitary swelling with purulent discharge left axilla and went to a local surgeon where it was diagnosed as Tuberculosis and was treated with anti TB drugs for six months without any improvement and later referred to a Dermatologist.
In 2011 May he went to a dermatologist who advised him to consult plastic surgeon. Patient went to a corporate hospital at Hyderabad (India). All routine investigations were done and antibiotics were given for one week. Patient left the hospital due to lack of proper response.
In 2012 he went to another dermatologist and he gave medical treatment for three months without any improvement. He was advised to undergo surgery. Patient got disappointed and lost all the confidence on doctors and stopped all drugs for six months.
In 2013 he went for Homeopathy treatment for six months which costed Rs.30,000 without any improvement. Altogether he spent more than three lacs rupees over the last three year without any benefit.
On being admitted in our hospital in January 2014, the lesions were examined thoroughly and they were confined to the skin and subcutaneous tissue. A clinical diagnosis of Chronic suppurative axillary hidradenitis—Hurley stage 3, was made [1].
After necessary investigations he was operated for both axillae in two stages at four weeks interval [2,3]. Wide excision and primary skin grafting was done. Skin grafts were harvested from the thighs since local flaps are not feasible in this patient. Necessary splinting of axilla was done to prevent contracture and later physiotherapy was advised. For each operation he stayed in the hospital for two weeks.
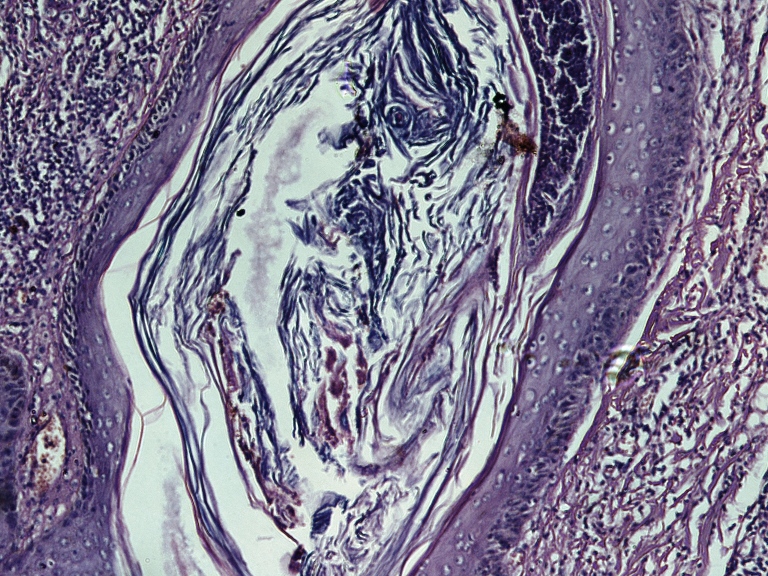
Histopathology (excised specimen)confirmed the diagnosis in both axillae [Table/Fig-4].
Histophotomicrograph showing follicular plugging with hyperkeratosis and microabscess (H&E*100)
The patient is doing well and he came for follow-up after seven months from his first surgery [Table/Fig-5].
Post operative 7 months RT and 6 months LT

Discussion
“HIDRADENITIS SUPPURATIVA” is a skin disease that most commonly affect areas bearing apocrine sweat glands like axillae, perimammaryregion, and inguinoperineal region(infection of the infundibulum of sweat glands). Aetiology still remains unknown but possible triggering factors are genetic, obesity, use of deodorants, depilation products, hot and humid climate etc [2].
It often goes undiagnosed for years because patients are too ashamed to consult medical practitioner. Many times it is mistaken for tuberculous lesion and anti tuberculous drugs are administered erronously for several months. Careful physical examination will avoid this mistake. Patients lose confidence and swap the doctors very frequently.
Even though conservative medical treatment is useful in early cases (Hurley’s stage 1) but for majority of patients with chronic disease wide surgical excision and skin grafting is the procedure of choice even though in early and resistant cases we can avoid skin grafting by layered primary suture. In current case excision of lesions in perineal region was performed and primary repair was done. Whenever feasible we can use parascapular random or fasciocutaneous flaps for resurfacing the axillary defect. In three of our cases belonging to Hurley stage-1, the defect was repaired in layers without the need of skin graft or flap with good result.
This case of chronic bilateral Axillary Hidradenitis as clinician’s corner will be educative and will help physicians for proper diagnosis and advise regarding appropriate treatment.
[1]. Hurley HJ, Axillary hyperhidrosis,hydradenitissuppurativa,and familial benign pemphigus: surgical approach.In:RoenigkHH,editorsDermatologicsurgery 1989 New YorkMarcel Dekker:729-39. [Google Scholar]
[2]. Schwartz”s principles of surgery 2010 9th editionchapter 16, the skin and subcutaneous tissue, pg. 409-10 [Google Scholar]
[3]. Slade DEM, Powell BW, Mortimer PS, Hidradenitissuppurativa: pathogenesis and managementBr J Plast Surg 2003 56(5):451-61. [Google Scholar]