Plasmacytoma is a malignant disease that present either in bone marrow (medullary plasmacytoma), within the bone (solitary plasmacytoma of bone), or outside of bone, as the extramedullary plasmacytoma. Extramedullary plasmacytoma accounts for 3% of all plasma cell tumours and approximately 90% of extramedullary plasmacytomas affect the head and neck region commonly affecting the nasal cavity, paranasal sinuses, tonsillar fossa and oral cavity. Multiple extramedullary plasmacytoma is defined when there is more than one extramedullary tumour of clonal plasma cells and such presentations are extremely rare. We report such a rare case of multiple extramedullary plasmacytoma involving gingiva and neck. Here is a case report of a 65-year-old female patient presenting with extramedullary plasmacytoma of the gingiva and soft tissue in neck.
Gingiva, Plasmacytoma, Soft tissue
Case Report
A 65-year-old female of Indian origin visited the Out Paitent Department of M.R. Ambedkar dental college, Bangalore (India) in the year 2007 with a complaint of a growth in her lower jaw front teeth region since four months. It started as a small growth which gradually increased to the present size and the patient had no other associated symptoms like pain, difficulty in chewing, speech or deglutition. No treatment was taken for the same. She also noticed a swelling in the neck two months prior to the onset of the intra oral swelling and was also not associated with any symptoms of that or any other similar lesions anywhere in the body [Table/Fig-1].
On general examination a solitary swelling was found on left side of the neck, approximately measuring about 2cm in diameter. Its borders were not well demarcated. Inferiorly it was 3cm above the clavicle, medially about 4cm away from the midline and superiorly it up extended to the level of the thyroid cartilage. Skin over the swelling appeared to be normal. On palpation inspectory findings were confirmed. There was no local rise of temperature. It was soft in consistency, non-tender and skin over the swelling was pinch able. Lymph node examination revealed sub mental and right submandibular lymph nodes palpable, about 0.5cm diameter, firm, fixed and non tender.
Intraoral examination revealed a solitary well defined, sessile, predominantly pale growth measuring approximately 4.5x3x 4cm and emerging lingually from marginal gingiva of mandibular incisors to the marginal gingiva of the canine and inferiorly about 2cms above the lingual sulcus [Table/Fig-2]. Mucosa over swelling appeared pale and was associated with no discharge. Teeth in area of complaint were Grade I mobile, tender and vital. Growth was firm, non-tender and no discharge was elicited on palpation. It was not fixed to the atesh5underlying bone. TMJ examination was normal with three finger mouth opening.
For the intraoral swelling provisional diagnosis of irritational fibroma was given. Differential diagnosis of pyogenic granuloma, peripheral giant cell granuloma, peripheral ossifying fibroma, soft tissue plasmacytoma, Multiple myeloma was considered.
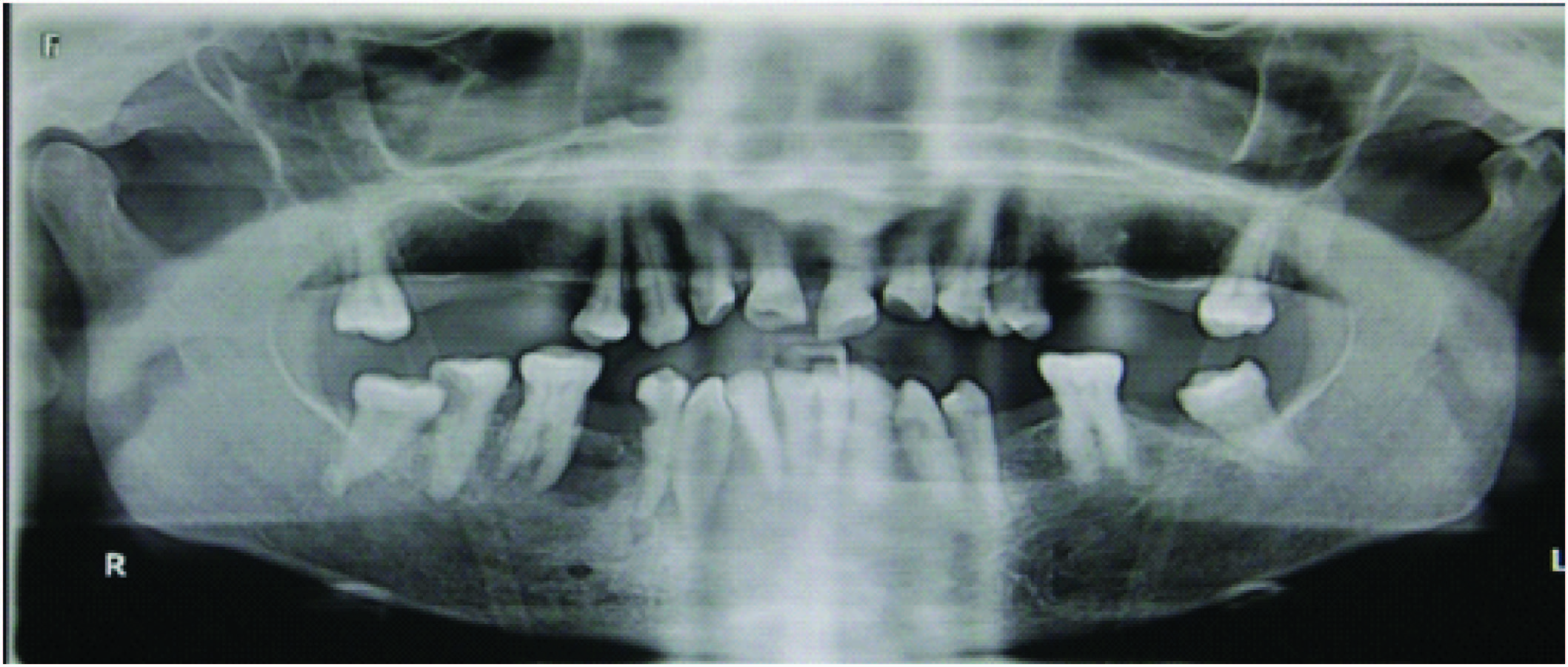
Radiological investigations revealed hazy radiolucency in relation to 42 and 43 [Table/Fig-3]. No cortical changes were observed and OPG also did not reveal any significant changes[Table/Fig-4,5]. Further investigations were carried out which included radiographs of long bones, chest radiography, bone marrow aspiration cytology, serum M-protein. Radiological examinations of long bones were negative. Bone marrow aspiration showed normal plasma cells within normal limits. Urine analysis to check for proteinuria and Bence-Jones protein were found to be negative. Serological investigations revealed calcium level within normal limits and serum M protein was negative. CT scan was not done.
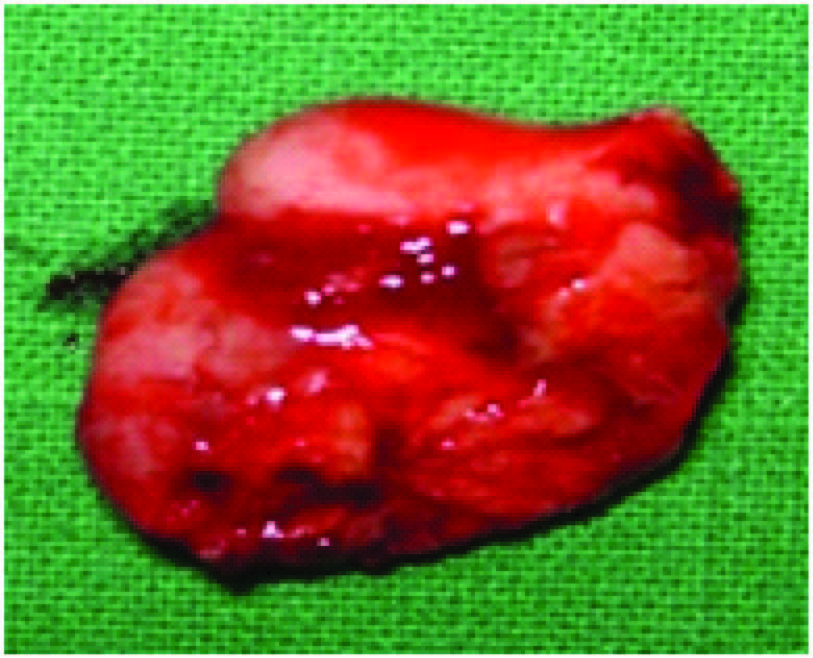
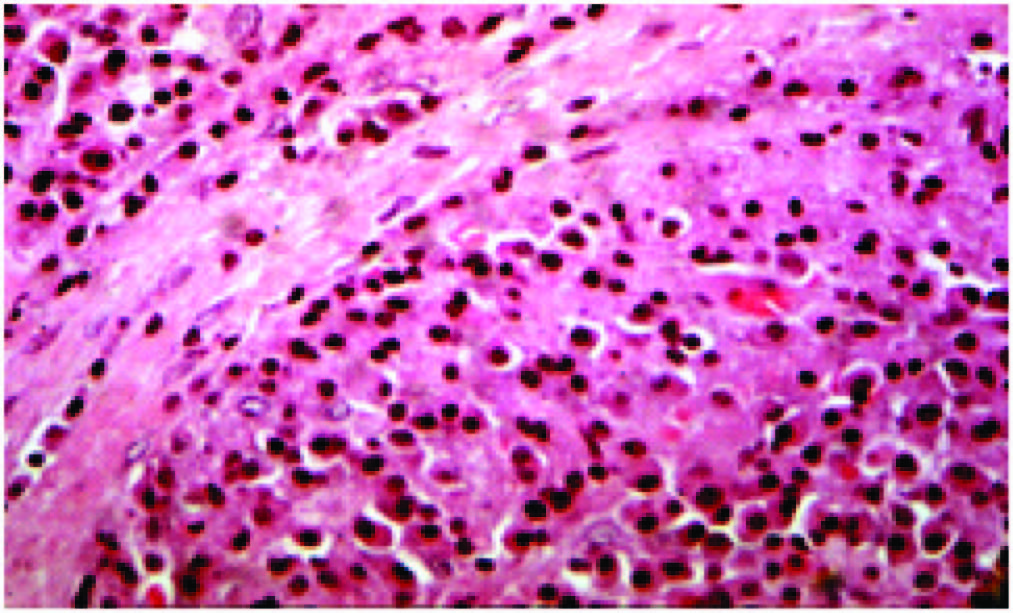
FNAC of the neck swelling was advised. Smear showed good number of plasma cells and lymphocytes and few atypical cells suggesting plasmacytoma. Incisional biopsy of oral growth was performed using electrocautery [Table/Fig-6]. Histopathologic features showed [Table/Fig-7] underlying connective tissue was infiltrated by plasma cells which were closely packed arranged in sheets and islands with varying degrees of differentiation and few atypical plasma cells were present suggestive of extramedullary plasmacytoma. The choice of treatment is radiotherapy as EMPs are very radiosensitive. Our case was referred to undergo the same. Our case did not undergo radiotherapy or chemotherapy as she was not willing for the same. However, she took some naturotherapy treatment and was reported by her relatives to be responding well to the treatment. She had not developed any other growths nor progressed to multiple myeloma. She expired a year later due to cardiac arrest.
Discussion
Plasmacytoma is the accepted nomenclature for a solitary tumour of plasma cells, located either in bone marrow (medullary plasmacytoma), the solitary plasmacytoma of bone, or outside of bone, the extramedullary plasmacytoma [1]. It accounts for 1-2% of human malignancies and occurs at the rate of 3.5/100,000 per year [2-4]. Plasmacytoma may present as one of the three clinical entities: Multiple Myeloma (MM), Extramedullary Plasmacytoma (EMP) or Solitary Plasmacytoma of Bone (SPB) [5-7].
Extramedullary plasmacytoma is defined as the neoplastic proliferation of plasma cells in soft tissues. It accounts for 3% of all plasma cell tumours. Approximately 90% of extramedullary plasmacytomas affect the head and neck region commonly affecting the nasal cavity, paranasal sinuses, tonsillar fossa and oral cavity. The aetiology of this disease is unknown but chronic stimulation, overdose irradiation, viruses, gene interaction especially in the reticuloendothelial system have been suggested as etiological factors [5]. Between 1905 and 1997 there had been more than 400 published reports addressing extramedullary plasmacytomas [8]. From these, Alexiou et al., culled 714 cases (82.2%) that were found in the upper aero digestive tract. Other regions of the body accounted for the sites in 155 cases (17.8%). Typical extramedullary plasmacytoma of the upper aero digestive tract is a solitary, sub mucosal, reddish, sessile or polypoid tumour that is rarely ulcerated. Pedunculated lesions are more often seen in the larynx and pharynx, while sessile tumours have a sinonasal predilection. Friability and softness may indicate a more aggressive lesion. There may be more than one mucosal plasmacytoma in the same anatomic region. Multiple plasmacytomas involve more than one localized area of bone destruction or extramedullary tumour of clonal plasma cells without bone marrow metastasis or related organ or tissue impairment. Multiple Soft tissue localization elsewhere is extremely uncommon.
Multiple Myeloma is a systemic disease and is characterized by neoplastic proliferation of monoclonal immunoglobulin(M protein).It is a disseminated disease involving many bones [9]. Incidence of MM is below 1% of all malignancies and 10% of all haematological neoplasm. Solitary plasmacytomas is seen in 10% of plasmacytomas and is classified as SPB and EMP. Plasmacytoma of bone is twice as common as EMP [9]. EMP as such is a rare occurrence accounting for only 3% of plasma cell tumours and has a male predilection with male: female ratio being (4:1) [8]. Wiltshaw classified soft tissue plasmacytoma into three clinical stages: Stage I - Limited to an extramedullary site; Stage II - Involvement of regional lymph nodes; Stage III - Multiple metastasis (although it is no longer a solitary plasmacytoma [10]. Our case would fall under the category of stage II of wiltshaws classification. Criteria for diagnosis of EMP include: lesions or other tissue involvement, biopsy proven plasma cell tumour, absence of osteolytic bone, bone marrow plasma cell infiltration not exceeding 5% of all nucleated cells, low serum electrophoresis. M-protein concentration if present, and no hypercalcemia or renal involvement due to plasma cell dyscariasis. Our case fulfils all the above criteria required to diagnose it as EMP.
Extramedullary plasmacytomas can be solitary or multiple [11]. The international myeloma working group in 2003 came up with a separate classification of plasmacytomas that occur as multiple sites of disease in soft tissue, bone or both soft tissue and bone as multiple solitary plasmacytomas [12].
Our case presents multiple EMP one in the neck and the other in the gingiva and is in itself a rare entity. EMP occurs in males: female ratio of 4:1 usually under 55y of age [12]. In a comprehensive literature search reviewing over 700 patients with EMPs, the EMPs developed predominately in head and neck region, especially in the upper respiratory tract such as nose, paranasal sinuses, nasopharynx and tonsils. Infrequent sites of involvement include the gastrointestinal tract, liver, spleen, pancreas, lungs, thyroid, breast, testis or skin [13]. EMP affecting the gingiva as a soft and gelatinous growth in the lower anterior region is very rare. It was first described by Martinelli in 1968 as a sessile neoplasm from left to right canine, easily to be confused with chronic gingivitis [14]. Moshreff et al., reported a polypoidal growth in left upper canine clinically similar to peripheral giant cell granuloma [15]. EMP presenting as multiple subcutaneous soft tissue masses on the neck and the oral cavity as in our case is rare. Chronic stimulation of inhaled irritants and constant upper respiratory tract infections are postulated to have some relation to EMP occurring in the aero digestive tracts [9]. Overdose irradiation,viruses, gene interaction especially in the reticuloendothelial system have been suggested as etiological factors [5]. EMP should be differentiated from other inflammatory reactive lesions occurring in the gingiva like pyogenic granuloma, peripheral giant cell granuloma and peripheral ossifying granuloma. The histopathological picture is the best way to rule out other reactive lesions as Extramedullary Plasmacytomas will replace tissues unlike the inflammatory reactive lesions which causes disposition of the tissues with plasma cells and other inflammatory components. This stromal growth pattern, mixedcellularity, polyclonality is what separates the extramedullary plasmacytoma from inflammatory reactive lesions. There is the reduced presence or many a times even absence of Russell bodies in plasmacytomas unlike inflammatory lesions.
Though local lymph node involvement is there in our case it does not necessarily mean a worse prognosis or progression to MM [8]. Radiotherapy is the choice of treatment since plasmacytoma is very radiosensitive [16,17]. Some reports have shown long term control following radiotherapy in a solitary lesion with high likelihood of cure [3,18,19]. Mendenhall et al., have described 94% control rate with solitary plasmacytomas following 40GY radiation for four weeks while some others have shown less favourable results [10,11]. Of all of the plasma cell tumours, EMPs have the best prognosis. Conversion to MM is less than 20% cases and chances of a 10 y survival are seen in more than 70% cases [11].
Swelling in the lateral side of neck


Occlusal radiograph shows no cortical changes
Excisional biopsy done using electrocautery
Histopathology picture showing sheets of plasma cells and some pleomorhic nuclei also visible
Conclusion
A lifelong evaluation for disease progression is necessary with all plasmacytomas. This includes frequent bone marrow aspirations, skeletal survey with CT or MRI modalities, and serum and urine protein electrophoresis to detect the presence of M proteins. Once MM is present, systemic treatment with chemotherapy is recommended using various alkylating agents in combination with glucocorticoids (2-3 y of survival rate). However, it is very important from a clinician point of view to thoroughly elicit the history and do a thorough physical as well as intra oral examination of such a case cause many a times the patients would be reporting first to a dentist considering it to be a minor problem as in our case. Subsequent radiological, urine blood and histipathological tests are mandatorywhen malignant disease is suspected.
[1]. RH Liebross, CS Ha, JD Cox, D Weber, K Delasalle, R Alexanian, Clinical course of solitary extramedullary plasmacytomaRadiother Oncol 1999 52:245-49. [Google Scholar]
[2]. WM Mendenhall, CM Mendenhall, NP Mendenhall, Solitary plasmacytoma of bone and soft tissuesAm J Otolaryngol 2003 24:395-99. [Google Scholar]
[3]. TW Bolek, RB Marcus, NP Mendenhall, Solitary plasmacytoma of bone and soft tissueInt J Radiat Oncol Biol Phys 1996 36:329-33. [Google Scholar]
[4]. YC Nofsinger, N Mirza, PT Rowan, D Lanza, G Weinstein, Head and neck manifestations of plasma cell neoplasmsLaryngoscope 1997 107:741-46. [Google Scholar]
[5]. JJ Pisano, R Coupland, SY Chen, AS Miller, Plasmacytoma of the oral cavity and jaws: a clinicopathologic study of 13 casesOral Surg Oral Med Oral Pathol Oral Radiol Endod 1997 83:265-71. [Google Scholar]
[6]. PA Wingo, T Tong, S Bolden, Cancer statistics, 1995. CA Cancer J Clin. 1995;45:8–30Erratum in: CA Cancer J Clin 1995 45:127-28. [Google Scholar]
[7]. JG Batsakis, Plasma cell tumors of the head and neckAnn Otol Rhinol Laryngol 1983 92:311-13. [Google Scholar]
[8]. C Alexiou, JK Reinhardt, H Dietzfelbinger, Extramedullary plasmacytoma: tumor occurrence and therap eutic conceptsCancer 1999 85:2305-14. [Google Scholar]
[9]. R Ozdemir, O Kayiran, M Oruc, O Karaaslan, U Kocer, D Ogun, Plasmacytoma of the hard palateJ Craniofac Surg 2005 16:164-69. [Google Scholar]
[10]. E Wiltshaw, The natural history of extramedullary plasmacytoma and its relation to solitary myeloma of bone and myelomatosisMedicine 1976 5:217-38. [Google Scholar]
[11]. P Galieni, M Cavo, A Pulsoni, Clinical outcome of extramedullary plasmacytomaHaematologica 2000 85:47-51. [Google Scholar]
[12]. International Myeloma Working group. Criteria for classification of monoclonal gammopathies, multiple myeloma and related disorders: a report from international myeloma working groupBr J Haematol 2003 121:749-57. [Google Scholar]
[13]. R Bataille, J Sany, Solitary myeloma: clinical and prognostic features of review of 114 casesCancer 1981 48:845-51. [Google Scholar]
[14]. C Martinelli, MA Rulli, Primary plasmacytoma of soft tissue (gingiva). Report of a caseOral Surg Oral Med Oral Pathol 1968 25(4):607-09. [Google Scholar]
[15]. M Moshref, Plasmacytoma of the gingivaArch Iranian Med 2007 10:91-93. [Google Scholar]
[16]. S Majumdar, U Raghavan, NS Jones, Solitary plasmacytoma and extramedullary plasmacytoma of the paranasal sinuses and soft palateJ Laryngol Otol 2002 116:962-65. [Google Scholar]
[17]. SB Kapadia, U Desai, VS Cheng, Extramedullary plasmacytoma of the head and neck. A clinicopathologic study of 20 casesMedicine (Baltimore) 1982 61:317-29. [Google Scholar]
[18]. SE Bush, DR Goffinet, MA Bagshaw, Extramedullary plasmacytoma of the head and neckRadiology 1981 140:801-05. [Google Scholar]
[19]. GH Fletcher, H Goepfert, Larynx and pyriform sinus. In: Fletcher GH, edTextbook of Radiotherapy 1980 3rd EditionPhiladelphiaLea and Febiger:286-329. [Google Scholar]