Pancytopenia is reduction in all the three major cellular elements of blood; hence it is the simultaneous presence of anaemia, leucopenia and thrombocytopenia. It is not a disease entity but a triad of findings that may result from various disease processes, primarily or secondarily involving the bone marrow [1]. The complete hematological work up with good clinical correlation is of utmost importance to evaluate the cause of pancytopenia and planning further investigations [2]. Bone marrow aspiration and biopsy are indispensable adjunct to the study of hematopoetic disorders. The final interpretation requires the integration of peripheral blood findings, bone marrow aspirate and trephine biopsy evaluation, together with the results of supplementary tests such as immunophenotyping, cytogenetic analysis and molecular genetic studies as appropriate [3]. Bone marrow examination is indicated in all cases of pancytopenia where the underlying cause is not quite obvious. This is particularly needed in case of hypoplasia/aplasia and to exclude leukaemia or other malignant infiltration [4]. Routine aspiration smears may have to be combined with trephine biopsies as quite often aspiration might yield dry or bloody tap. Few clear recommendations can be found as to the optimal investigative approach to pancytopenia. Some experts suggest that marrow examination is essential to the diagnosis, but it has not been established whether the procedure is necessary in all pancytopenic patients [5]. The present study was undertaken to evaluate the role of Bone marrow aspiration and Bone marrow biopsy in cases of pancytopenia.
Materials and Methods
The present study is a prospective clinicohematological study undertaken from November 2011 to November 2013 on fifty patients of pancytopenia fulfilling the inclusion criteria (i.e. Hemoglobin < 9 gm/dL, Total Leucocyte count < 4×109/L and Platelet Count <100×109/L). Informed consent was taken from all patients prior to enrollment in the study. Relevant history and physical examination findings were recorded. Hematological investigations included a complete hemogram including hemoglobin percentage, TLC, DLC, platelet count, red blood cell indices, peripheral blood examination and reticulocyte count. Bone marrow aspiration and biopsy were performed simultaneously in all cases. Perl’s stain for grading of bone marrow iron stores were done in all cases and special stains like MPO, PAS and reticulin were done wherever necessary. Various causes of pancytopenia were studied based on aspiration and biopsy findings. Significant parameters like aetiology, age, gender, clinical features, hematological parameters, peripheral blood film, bone marrow aspiration and bone marrow biopsy findings in different cases of pancytopenia were compared with various studies published in literature.
Results
The age of patients included in study ranged from 6 to 78 years. Maximum numbers of cases were seen in the age group of 10 to 30 y and least seen in age group 70 years and above. Of the total number of cases, 64% cases were males and 36% cases were females with over all male to female ratio of 1.8:1
In the present study aplastic anaemia was found to be the most common aetiology of pancytopenia followed by normoblastic erythroid hyperplasia, and megaloblastic anaemia. Other causes included acute leukemias, myelofibrosis, dimorphic erythroid hyperplasia, lymphoid neoplasia and iron deficiency anaemia [Table/Fig-1].
Etiological distribution of pancytopenia
| Etiology | Number | Percentage |
|---|
| Aplastic Anaemia | 13 | 26% |
| Normoblastic erythroid hyperplasia | 11 | 22% |
| Megaloblastic Anaemia | 8 | 16% |
| Acute Leukemia | 7 | 14% |
| Myelofibrosis | 4 | 8% |
| Dimorphic erythroid hyperplasia | 4 | 8% |
| Lymphoid neoplasia | 2 | 4% |
| Iron deficiency anaemia | 1 | 2% |
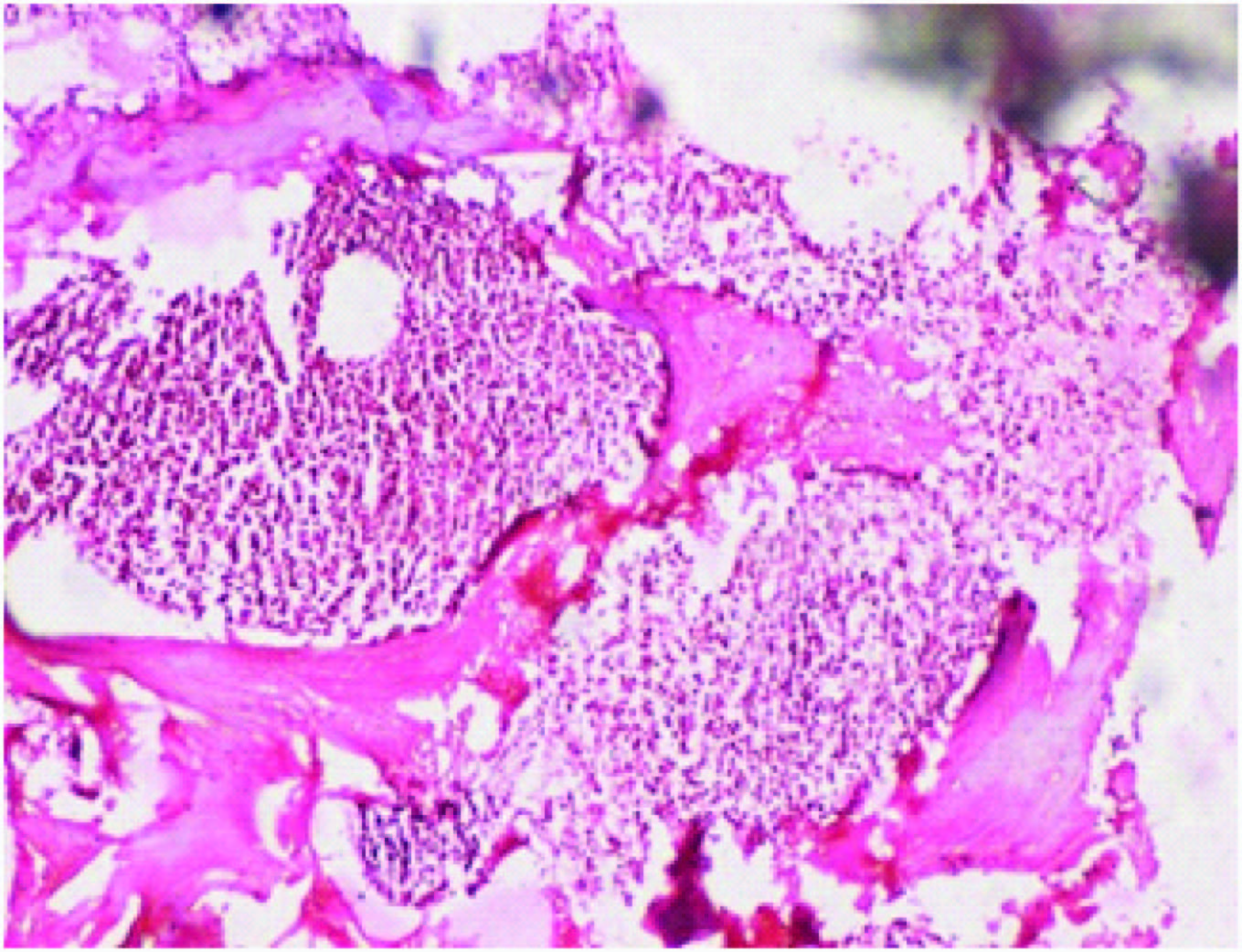
Cellularity of the bone marrow was assessed taking in consideration the age of the patient. It was seen that 48 % patients presented with hypercellular marrow, 34% with hypocellular marrow and 18% with normocellular marrow. Out of 17 patients with hypocellular marrow, 76.5% patients were due to aplastic anaemia and 23.5% presented with myelofibrosis. Out the 24 cases presenting with hypercellular marrow 62.5% presented with erythroid hyperplasia, 29.2% with acute leukemias and 8.3% with lymphoid neoplasia. Amongst 9 cases of nomocellular marrow, 14% showed normoblastic erythropoiesis, 2% megaloblastic and 2% dimorphic erythropoiesis.
A total of 24 bone marrow aspirations showed erythroid hyperplasia in a normocellular or hypercellular marrow [Table/Fig-2]. The bone marrow aspiration showed normoblastic erythropoiesis in 45.8%, megaloblastic in 33.3 %, dimorphic 16.7% and micronormoblastic picture in 4.2%.
Bone marrow trephine biopsy section showing hypercellular marrow. (H&E, X200)
Significant past history included jaundice and viral hepaptitis. There was also history of blood transfusion in majority of patients and alcohol consumption. The most common clinical presentation was weakness (75%) followed by fever (71%), weight loss (21%) and bleeding tendencies (8%). Common physical examination findings included pallor seen in 75% of patients, hepatomegaly (16%) and splenomegaly (8%).
Eight patients out of 24 patients with erythroid hyperplasia showed a megaloblastic picture. There was significant drug history and history of multiple blood transfusions. The most common finding on peripheral film was anisopoikilocytosis. Hypersegmented neutrophils and nucleated RBCs were also seen. Reticulocyte count varied from 1.0% to 1.9%.
On bone marrow aspiration, 87.5% patients showed hypercellular bone marrow and 12.5% patients showed normocelular marrow but biopsies of same patients showed hypercellular marrow with erythroid hyperplasia in 100% patients. Grading of bone marrow iron stores was done on bone marrow aspiration film using Perls’s Prussian blue reaction. 62.5% of patients showed increased iron stores, 25% showed normal iron stores and 12.5% showed decreased iron stores. The increased stores could be due to associated chronic malabsorption syndrome or autoimmune disorder.
Ten patients out 24 cases of erythroid hyperplasia on aspiration showed normoblastic erythropoiesis out of which 3 were further evaluated for hemolytic anaemia. The anaemia was predominantly dimorphic seen in 63.9 % patients, normocytic (18.1%), microcytic (9%) and macrocytic (9%). Reticulocyte count varied from 0.5% to 1.6%. On Bone marrow aspiration, 87.5% showed a normocellular marrow. On further examination of biopsy it was seen that 3 patients showed hypercellularity on biopsy (37.5%). Grading of bone marrow iron stores was done on bone marrow aspiration film using Perls’s Prussian blue reaction. Increased stores in 91% patients and normal iron stores were seen in 9% cases.
Hemolytic anaemia was suspected in three cases. History of jaundice was present in one patient and raised serum bilirubin and hepatosplenomegaly was seen in two patients. History of recent blood transfusion was present in all three cases. The predominant blood picture on peripheral blood film was dimorphic (66.7%) and increased polychromasia was seen in one patient (33.3 %). Reticulocyte count varied from 1.2 to 1.6% Bone marrow aspiration showed hypercellular marrow with erythroid hyperplasia predominantly of intermediate normoblasts with normoblastic erythropoiesis in 100% patients. Bone marrow biopsy presented with hypercellular marrow with erythroid hyperplasia in 100% patients. Two patients were found deficient in G6PD enzyme. Increased iron stores were seen in 100% patients. This could be attributed to the multiple blood transfusions received by such patients or associated chronic disease.
Out of 24 cases with erythroid hyperplasia, a single case showed micronormoblastic erythropoiesis on aspiration. Bone marrow aspiration and biopsy showed hypercellular marrow with erythroid hyperplasia. Bone marrow showed decreased iron stores (Grade 2).
In present study seven patients presented with subleukemic leukemia. The age of the patients ranged from 6 to 45 y. The male to female ratio was 2.5:1. The most common presenting symptoms were fever seen in 100% of cases and weakness seen in 71.5 %. Other clinical features included weight loss (42.8%) and bleeding tendencies (28.8%). The most common physical examination findings were pallor found in 100% of patients and hepatosplenomegaly seen in 85.7 % of patients. Lymphadenopathy was seen in 14.3 % of patients. Reticulocyte count ranged from 0.5 to 2.5 %. The predominant blood picture was dimorphic (71.4%). Macrocytic (14.3%) and microcytic (14.3%) blood picture was also seen.
Out of seven patients five presented as AML and 2 patients presented as ALL. One patient of AML presented as bloody tap. All cases were diagnosed based on morphology of blast cells and use of cytochemical stains such MPO stain and PAS stain in peripheral film or bone marrow aspiration. Further subtyping based on morphology of blast could be done in 3 cases of AML and both patients of ALL. One patient with AML required immunohistochemistry for further subtyping. Fibrosis was also seen in H&E stained specimen and grading with reticulin stain showed Grade 2 fibrosis in 2 patients with AML and grade 1 fibrosis in one patient with ALL. The iron stores were found to be increased in 100 % cases of acute leukemia. The grade varied from grade 3 to grade 5.
In the present study two patients were diagnosed with lymphoproliferative disorder. The most common presenting symptom was fever seen in both patients. Other symptoms were weakness, weight loss and bleeding tendencies. One patient presented with bloody tap and initial diagnosis was made on bone marrow imprint smear. Biopsy showed hypercellular marrow in both cases. Fibrosis was seen in one patient on biopsy (Grade 2). Bone marrow iron stores was increased in both patients(grade 4 and 5).
A total of 17 patients presented with hypocellular marrow. Two patients presented with dry tap and diagnosis was made on bone marrow biopsy.
Amongst 17 patients with hypocellular marrow, 13 presented with aplastic anaemia. The diagnosis was made on the bone marrow biopsy specimen which showed increase in marrow adipose tissue and overall decrease in marrow cellularity with relative increase in marrow lymphocytes and plasma cells [Table/Fig-3,4]. Reticulin staining of bone marrow biopsy showed no fibrosis in all cases. The most common symptoms were weakness (76.9%) and fever (61.5%). Other symptoms were weight loss (23%) and bleeding tendencies (15.4%).Most common sign was pallor seen in 92%. Spleen was palpable in one patient that presented as a case of pyrexia of unknown origin and jaundice. Splenomegaly could be attributable to underlying infectious causes.
Bone marrow aspiration smear showing increased fat spaces with trapped lymphocytes and plasma cells in Aplastic anaemia (Leishman stain, X100)

Bone marrow trephine biopsy section showing increased fat spaces and decreased cellularity in Aplastic anaemia. (H&E stain, X200)
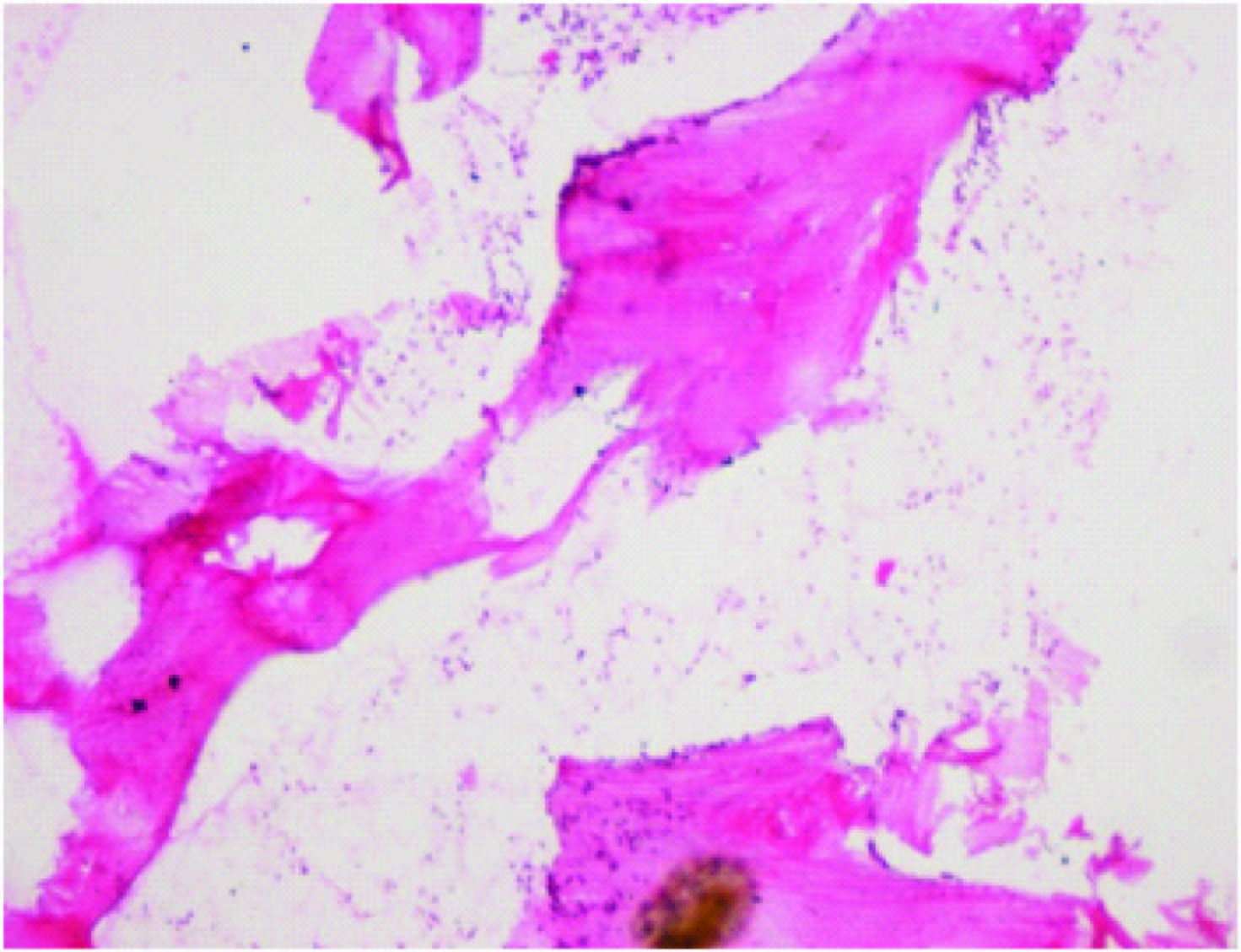
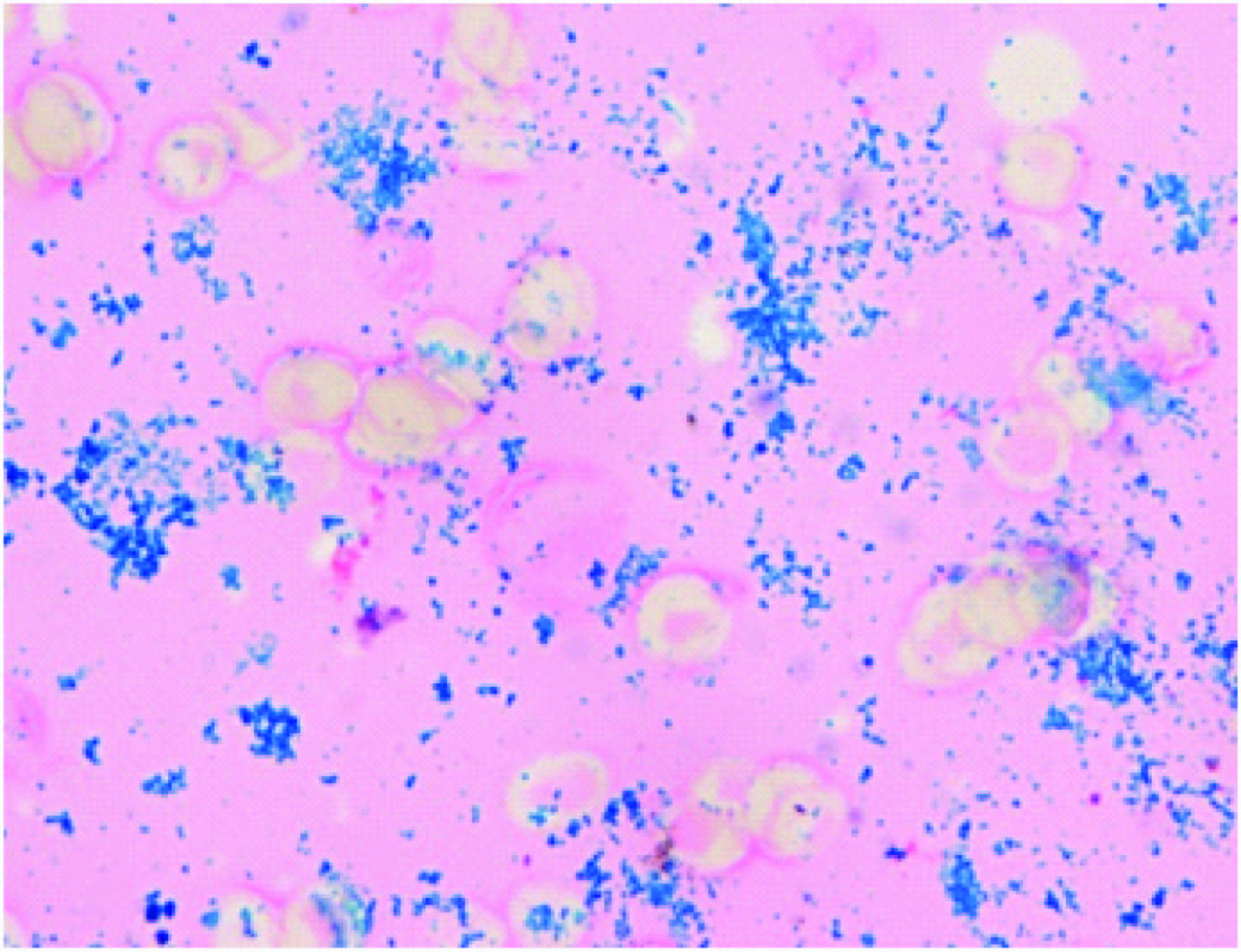
The reticulocyte count varied from 0.5 to 3.2%. Reticulocytopenia was seen in 23% patients. Predominant blood picture was dimorphic seen in 61.5% patients. Macrocytosis was seen in 23% patients and microcytosis seen in 15.5% patients. Most common finding in peripheral film was anisopoikilocytosis seen in 47% patients. A single patient presented with a reticulocyte count of 3.2% which indicates bone marrow regeneration which could be due to treatment therapy. Out of 13 cases presenting with hypocellular marrow, 3 presented with patchy hypocellularity with cellularity varying from 25 to 50% and10 patients with cellularity less than 25%. In all cases reticulin staining on bone marrow biopsy showed no fibrosis. All patients presented with increased stores of iron on aspiration i.e. Grade 3 (53.8%) and Grade 4 (38.5%) and Grade 5 (7.7%) [Table/Fig-5]. A single case presented as dry tap and iron grading was done on biopsy.
Bone marrow aspiration smear showing dense large clumps of large dense granules. Aplastic anaemia with bone marrow iron stores grade 5 (Perl’s, X400),
Out of 17 cases with hypocellular marrow, 4 cases presented with fibrosis in the bone marrow biopsy which was detected on H&E [Table/Fig-6] and reticulin staining of the biopsy specimen. Grading of the fibrosis was done using reticulin stain on bone marrow biopsy specimen.
Bone marrow biopsy section showing fibrotic phase of myelofibrosis, (H&E, X200),

The most common presenting features were fever (75%), weakness (75%), bleeding tendencies (66.7%) and weight loss (25%). The most common sign was found to be pallor in all 4 patients (100%). Other common findings were splenomegaly (50%) and hepatomegaly (25%). Lymphocytosis was seen in 50% patients. Reticulocyte count range was 0.9 to 2.6%. The predominant blood picture was dimorphic. Anisopoikilocytosis was the most common finding. It was seen that out of the 4 cases of myelofibrosis a single case presented with dry tap. All patients presented in the fibrotic phase with grade 2 and 3 fibrosis [Table/Fig-7]. Bone marrow iron stores were found increased in all cases of myelofibrosis with Grade 4 iron stores seen in 75% patients and grade 5 in 25% patients.
Dis, Bone marrow trephine biopsy section showing grade 3 fibrosis in myelofibrosis. (Reticulin, X200)

Discussion
There is a wide range of disorders that manifest as pancytopenia. The underlying etiology of pancytopenia varies across different geographical regions. The most common cause of pancytopenia reported from various studies across the world is aplastic anaemia and its frequency varies from 10% to 52.7% [6–8] which corroborates with our study in which aplastic anaemia was found in 26% of the patients. Various studies conducted in the Indian Subcontinent show megaloblastic anaemia to be the most common cause of pancytopenia followed by aplastic anaemia [9]. However, in few studies aplastic anaemia constituted the most common cause of pancytopenia [10,11]. Studies done in India show the most common age involved to be in the third decade with male preponderance [7,9] which corroborates with our study. Megaloblastic anaemia was found to be predominant in various Indian studies because of high prevalence of nutritional anaemia in the Indian subcontinent. Most common complaints in our study and other Indian studies were fever followed by weakness and bleeding tendencies. Pallor was the most common sign followed by hepatosplenomegaly. Peripheral blood film showed hypersegmented neutrophils and dimorphic blood picture in most of the studies which corroborated with our study [1,9]. The peripheral blood smear and bone marrow examination are important diagnostic tools in diagnosis of megalobalstic anaemia and there is a high correlation for aspiration and biopsy especially in the case of megaloblastic anaemia with erythroid hyperplasia[1]. In the present study normoblastic erythropoiesis was present in18% of patients similar to other studies in which that normoblastic erythroid hyperplasia was second most common of pancytopenia following aplastic anaemia [7]. The relationship of normoblastic erythroid hyperplasia to pancytopenia is found to be uncertain. It is suggested that there is a possibilty that some of these cases represent one phase in the evolution of hypoplasia/aplasia, while some may be cases of refractory anaemia. Criteria for differentiation of these groups remain unsatisfactory and these patients should be kept under regular hematological follow up [7,12]. In the present study three patients were diagnosed with hemolytic anaemia correlating clinical findings, blood investigations and bone marrow aspiration findings. History of jaundice was present in 66.7% while hepatosplenomegaly was present in 33.3%. All three patients presented with hypercellular marrow with normoblastic erythropoiesis. Studies show that a bone marrow aspiration in patients presenting with hypersplenism and pancytopenia may reveal an underlying hematological malignancy or an infectious process [9–13]. The presence of hemolytic anaemia may be due to associated DIC. In the present study all the cases presented with normal bone marrow studies. Auto immune disorders like Grave’s disease, pernicious anaemia and celiac disease can also present with pancytopenia and associated autoimmune hemolytic disease [14]. In the present study all three patients had history of significant drug intake. It has been seen that drugs like cefoxitin can induce hemolytic anaemia and pancytopenia. The physicians should be made aware of drug induced hematological toxicities and blood counts should be monitored in patients receiving such medications [15]. It is always important to evaluate a patient presenting with hemolytic anaemia carefully as there are various underlying aetiologies for the cause of haemolysis. A single patient with pancytopenia and severe iron deficiency anaemia (Hb-5.5%) showed a micronormoblastic picture on aspiration with erythroid hyperplasia on biopsy and decreased bone marrow iron stores. It has been shown in various studies that iron deficiency presenting with pancytopenia is rare and can be made worse with iron replacement therapy due to decline in leucopoiesis and thromboboiesis [16].
In the present study 17 patients presented with hypocellular marrow on aspiration and in each patient the bone marrow biopsy was also evaluated with reticulin for fibrosis. Amongst that, 13 cases were diagnosed as aplastic anaemia and four patients were diagnosed as mylefibrosis which showed grade 2 and 3 fibrosis on reticulin staining. Myelofibrosis can be idiopathic or secondary. In the present study two patients have given significant drug history. One patient presented with HIV infection and was on treatment and the second patient presented with rheumatoid arthritis on treatment. Both patients could be examples of secondary myelofibrosis as shown by other studies in which secondary myelofibrosis was also found to be reversible on stopping treatment and dose dependent. The survival of patients with moderate-to-severe fibrosis is significantly worse than that of patients with no or mild fibrosis, both because of an increase of non-leukemic death and because of the increased rate of leukemic evolution. Hence, grading of marrow fibrosis in bone marrow has prognostic significance [17]. In the present study there was also a single case of aplastic anaemia that presented few months later as a case of acute myeloid leukemia with a normal total leucocyte count. Aspiration confirmed the diagnosis while biopsy showed a hypercellular marrow. Aplastic anaemia converting to acute myeloid leukemia is considered a rare phenomenon.
The prevelance of subleukemic leukemic in our study was 14% which was in corroborance with other studies done in the Indian subcontinent in which it ranged from 3% to 18% [2,7,9]. The value of bone marrow biopsy is found in mainly accurate assessment of cellularity and blast cell numbers. It is also found to be essential in diagnosis of hypoplastic AML [18]. Fibrosis was also seen in H&E stained specimen and grading with reticulin stain showed Grade 2 fibrosis in two patients with AML and grade 1 fibrosis in one patient with ALL-L1. Studies on the clinical significance of bone marrow fibrosis in patients with acute leukemia show that low RFD (Reticulin Fibre Density) values correlated with more favorable outcome than patients with high RFD [6].
Imprint smears are essential for studying the morphology of cells and making a diagnosis in case an aspiration is a dry tap or a bloody tap. In our study also, patients with dry or bloody tap were diagnosed on bone marrow imprint smears especially in the case of acute leukemia’s and lymphoid neoplasia. Studies on the comparison of touch imprints with aspiration smear show that there is no difference in the differential count between touch smears and aspiration in normocellular marrows. There was 78% positive correlation between aspirate and biopsy and 84.3% between imprint and biopsy in a study [19]. It has been suggested that evaluating touch imprints be considered a standard practice in examining the bone marrow [19].
Two patients in our study presented with lymphoid neoplasia with pancytopenia. Amongst them, one presented with bloody tap on aspiration and diagnosis was made on the basis of imprint smear. Bone marrow biopsy revealed hypercellular marrow and showed diffuse involvement in both cases which was comparable to other studies [20]. The presence of fibrosis in lymphoid neoplasia always points an abnormal marrow [20]. One patient in present study presented with grade 2 fibrosis. Thus examination of the bone marrow is of central importance in the diagnosis and staging of lymphoma.
Conclusion
Bone marrow aspiration is used principally for cytological assessment of the marrow and more valuable than trephine in studying morphology of cells. It also helps in further subtyping of anaemias and leukemias.
Biopsies are better at assessing overall cellularity of the bone marrow and architectural features like detection of fibrosis and infiltration and hence are more valulable in the diagnosis of aplastic anaemia and myelofibrosis. Trephine biopsies are useful in lymphoid neoplasia for assessing pattern of infiltration of bone marrow. In case of dry tap or bloody tap on aspiration, seen in patients with aplastic anaemia, subleukemic leukemia and lymphoid neoplasia, trephine biopsy is invaluable in reaching a diagnosis.
Bone marrow evaluation is especially useful in subleukemic leukemia where blast counts can be as low as 2% in the peripheral blood film but high in the marrow. Aspiration and biopsies are valuable in assessing bone marrow iron stores by Perls’ Prussian blue reaction. It is important to understand that either bone marrow aspiration or bone marrow biopsy is found to be more superior than the other in varied causes of pancytopenia, thus they be regarded as complementary to each other and should be performed together in all patients of pancytopenia. Thus, it is only through the correlation of important clinical, hematological and bone marrow examination findings, proper evaluation and management of patients presenting with pancytopenia can be done.