Waldenstroms Macroglobulinemia Patient Presenting with Rare ’lytic’ Lesions and Hypercalcemia: A Diagnostic Dilemma
Khalid Mehmood1, Iftikhar Haider Naqvi2, Syed Raza Shah3, Nazia Zakir4, Syed Mustafa Ali5
1 Professor and Chairman, Department of Medicine, Dow University of Health Sciences (DUHS), Karachi, Pakistan.
2 Assistant Professor, Department of Medicine, Dow University of Health Sciences (DUHS), Karachi, Pakistan.
3 Medical Student, Dow University of Health Sciences (DUHS), Karachi, Pakistan.
4 FCPS II Trainee, Dow University of Health Sciences (DUHS), Karachi, Pakistan.
5 Houseofficer, Dow University of Health Sciences (DUHS), Karachi, Pakistan.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Syed Raza Shah, Medical Student, Dow University of Health Sciences (DUHS), Karachi, Pakistan. Phone : +92-345-2454610, Email: syedraza91shah@live.com
Waldenstroms macroglobulinemia (WM) is an uncommon B-cell lymphoproliferative neoplasm characterized by lymphoplasmacytic cells infiltrating the Bone Marrow, along with demonstration of an IgM monoclonal gammopathy in the serum. Lytic lesions are considered one of the basis for differentiating a patient of Multiple Myeloma (MM) and WM. However, very few cases have been reported with a patient presenting with lytic lesions in a WM patient, thereby, complicating the disease. By finding the extent of these lytic lesions and bone involvement, Not only can we signify the presence or absence of bone lesions, but we can also direct the more efficient use of skeletal X-rays for documentation of the extent, location, and response of bone abnormalities to interventional chemotherapy and radiation therapy. Our case was mimicking the classic case of MM. Using the International Criteria for diagnosis for WM, diagnosis for MM was excluded and diagnosis for WM was made. After two weeks of therapy, the patient showed marked clinical improvement.
Lytic lesions, Multiple myeloma, Waldenstroms macroglobulinemia
Case Report
A 55-year-old male of average height and built, married and waiter by profession, resident of Karachi, Pakistan presented in OPD with complaints of Low-grade fever off & on since six months, shortness of breath (SOB) on exertion since four months, episodes of blackouts since two months, bleeding from the gums off & on since two months and productive cough since 15-20 d. Detailed inquiry revealed bilateral pain in knee joints for the past 3-4 y, decreased appetite and significant weight loss. There was a history of jaundice three years back. The patient was also operated for inguinal hernia twice. On examination, the patient was febrile, markedly anaemic with red gums showing mild bleeding at a few sites. Liver and spleen were palpable. Rest of the systems examination was unremarkable.
The differential diagnosis for the patient included Tuberculosis, Chronic liver disease, autoimmune hepatitis, Lymphomas, Paraproteinemia and Myeloproliferative disorders. Blood count revealed a low hemoglobin (4.4gm/dl) and a reduced platelet count (33,000/mm3). The Erythrocyte Sedimentation Rate (ESR) was noted to be high (130mm/hr). LFT’s were normal. Serology for Hepatitis B and Hepatitis C was negative, ANA, anti LKML was also negative. The normal LFT’, negative viral serology with negative ANA, AMA, ASMA and anti LKML ruled out the possibility of Chronic Liver Disease. The sputum D/R was normal and culture for AFB showed no growth of mycobacterium. PT and APTT were increased with a normal INR of 1.3. Serum calcium level was high (11.54mg/dl) and so was serum Creatinine level (1.7mg/dl).
The albumin level was normal but the Globulin level was elevated (8.9g/dL) with a significantly reduced A/G ratio of (0.3). Serum Protein Electrophoresis for the patient was done which showed high Total protein levels (11.6g/dL). Urinary Protein Electrophoresis was also done. Urinary electrophoresis showed the presence of gamma globulin and a Total Protein of 831 g/24 h. Traces of albumin were also seen.
Chest X-Ray was done which was normal. The Ultrasound scan of the abdomen showed Hepato-splenomegaly. The Computerized Tomography (CT) scan of the chest and abdomen showed multiple enlarged lymph nodes at perivascular area measuring 1.6 × 1.1 cm and at the right bronchial area, measuring 1.2 × 0.9 cm. The liver was enlarged measuring 19.3 cm with normal parenchymal attenuation. The spleen was enlarged measuring 16.2 cm with no focal mass seen in the splenic parenchyma. Sub-centimetre lymph nodes were present at the para-aortic and retroperitoneal regions.
Overall findings from examinations and investigations concluded hepatosplenomegaly along with mediastinal and abdominal lymphadenopathy which were consistent with lymphoma.
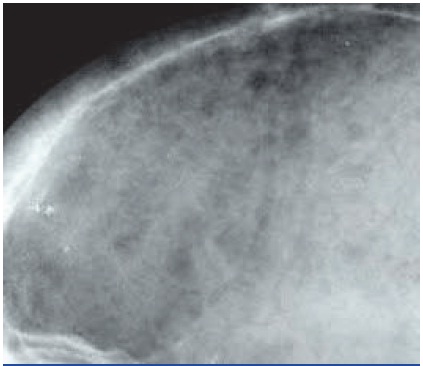
An immunoglobulin quantification was also carried out. IgM came out to be 168.3 g/L (Normal 0.40–2.3g/L). Due to hypercalcemia and increase globulin gap, a skull X-Ray was carried out [Table/Fig-1] which showed few scattered, lytic lesions consistent with Multiple Myeloma.
Skull X-Ray of the patient
Bone Marrow Trephine biopsy was also carried out which showed trilineage hematopoiesis. Megakaryocytes were also seen. Plasma cells were increased up to 9%. Bone marrow trephine (H & E) section showed diffuse infiltration with mononuclear cells comprising of mature lymphoid cells and plasma cells. However, more than 10% of the cells in the bone marrow were lymphoplasmacytoid lymphoma cells.
Overall findings were suggestive of B-cell lymphoproliferative disorder. Findings on immunofixation were consistent with Ig M kappa monoclonal gammopathy. Two important differentials included Multiple Myeloma and lymphoplasmacytic lymphoma (Waldenstroms Macroglobulinemia).Using the International Criteria for diagnosis for Waldenstrom Macroglobulinemia ,which is based on the presence of at least 10% of the cells in the bone marrow being lymphoplasmacytoid lymphoma cells, diagnosis for Multiple Myeloma was overruled and diagnosis for WM was made. A final diagnosis of Waldenstroms macroglobulinemia was made. The patient was started on thalidomide and prednisone. After two weeks of therapy, the patient showed marked clinical improvement, and his subsequent serum protein report showed a reduced Total protein level 3.3 g/dl, Globulin level 1.0 g/dL and an increased A/G ratio of 2.3 g/dL. The albumin levels remained normal.
Discussion
Jan Waldenstrom in 1944, described two patients with oronasal bleeding, anaemia, elevated ESR, thrombocytopenia, low serum fibrinogen and lymphadenopathy. The immunoglobulin was later found to be IgM [1].
Macroglonbulinemia with lytic lesions was first reported in 1956 [2]. Lytic lesions are considered one of the basis for differentiating a patient of Multiple Myeloma and WM [3]. However, very few cases have been reported with a patient presenting with lytic lesions in a WM patient, thereby, complicating the disease. Preliminary data indicates that a pattern of osteoclast-activating factor and osteoprotegerin expression similar to that observed in classic MM is present in IgM myeloma [2].
Renal complications have always been linked to less severity in patients with WM as compared to MM owing to the low hyper-calcemic level in WM patients [4]. However, 4% of the total WM patients have been reported for having hypercalcemia [4]. The cause of hypercalcemia remains unknown but some cases suggest that the cause maybe due to the binding of Calcium to IgM leading to pseudohypercalcemia or are maybe due to PTHrP induced [5,6].
The majority of WM patients do not require immediate therapy because many cases are detected before symptoms occur [7]. Treatment of WM is mainly based on results from phase II trials and expert recommendations [8]. Initiation of therapy is recommended for patients with constitutional symptoms (recurrent fever, night sweats, and fatigue or weight loss), progressive symptomatic lymphadenopathy or splenomegaly, hemoglobin 10 g/dL or fewer platelets [1]. The patient responded well to standard chemo-therapeutic regimen.
Our patient had lytic lesions and all the common signs and symptoms, a Multiple Myeloma patient would present with, including hypercalcemia. The creatinine level was very high as well-indicating some renal function loss, highly indicative of Multiple Myeloma. It is essential to confirm the presence of osteolytic lesions in patients presenting with primary macroglobulinemia. By carefully finding the extent of bone involvement and lytic lesions ,we can signify the presence or absence of these lesions leading to the more direct and more efficient use of skeletal x-rays for documentation of the location, response and extent of bone abnormalities for both interventional radiation and chemotherapy. This case was mimicking the classic case of MM. Using the International Criteria for diagnosis for Waldenstroms Macroglobulinemia, which is based on the presence of at least 10% of the cells in the bone marrow being lymphoplasmacytoid lymphoma cells, diagnosis for Multiple Myeloma was excluded and diagnosis for WM was made. After two weeks of therapy, the patient showed marked clinical improvement.
[1]. Kyle RA, Benson JT, Larson DR, Therneau TM, Dispenzieri A, Kumar S, Progression in smoldering Waldenstrom macroglobulinemia: long-term resultsBlood 2012 119(19):4462-66. [Google Scholar]
[2]. Konduri K, Sahota SS, Babbage G, Tong AW, Kumar P, Newman JT, Immunoglobulin M Myeloma: Evaluation of Molecular Features and Cytokine ExpressionClinical Lymphoma 2005 5(4):285-89. [Google Scholar]
[3]. Schuster S, Dispenzieri A, Rajkumar SV, Aspitia AM, Kyle R, Mikhael JR. IgM Multiple Myeloma: Disease Definition, Prognosis, and Differentiation From Waldenstrom’s Macroglobulinemia. New Orleans, LA. 5-8, 2009 [Google Scholar]
[4]. Dimopoulos MA, Alexanian R, Waldenstrom’s MacroglobulinemiaBlood 1994 83:1452-59. [Google Scholar]
[5]. Side L, Fahie-Wilson MN, Mills MJ, Hypercalcemia due to calcium binding IgM paraprotein in Waldenstrom’s macroglubinemiaJ Clin Pathol 1995 48(10):961-62. [Google Scholar]
[6]. Kremer Richard, MD, Parathyroid-Hormone-Related peptide in Hematolgic MalignanciesThe American Journal of Medicine 1996 100(4):406-11. [Google Scholar]
[7]. Hensel M, Brust J, Plöger C, Schuster D, Memmer ML, Franz-Werner J, Excellent long-term survival of 170 patients with Waldenström’s macroglobulinemia treated in private oncology practices and a university hospitalAnn Hematol 2012 91(12):1923-28. [Google Scholar]
[8]. Kristinsson SY, Eloranta S, Dickman PW, Andersson TML, Turesson I, Landgren O, Patterns of survival in lymphoplasmacytic lymphoma/waldenström macroglobulinemia: A population-based study of 1,555 patients diagnosed in Sweden from 1980 to 2005Am J Hematol 88 :60-65. [Google Scholar]