Antimicrobial agents are used for prevention and the treatment of various infections. Antimicrobial agents are used empirically for the treatment of infections without culture sensitivity test [1]. An Intensive Care Unit (ICU) is a designated ward of a hospital where critically ill patient are monitored and treated [2]. Patients may require ventilator support in many critical condition due to respiratory failure and there is higher risk of hospital acquired infections in these patients [3]. Antimicrobial agents are prescribed in ICU for prevention and treatment of critical illnesses and hospital acquired infections [4]. According to American Thoracic Society guideline cephalosporins, carbapenem, piperacillin+tazobactam, aminoglyocsides, quinolones (levofloxacin, ciprofloxacin), vancomycin and linezolid are prescribed empirically in patients on ventilator to prevent hospital acquired infections [5].
There is lack of information about the use of antimicrobial agents in patients on ventilator in the ICU at tertiary care teaching hospital Ahmedabad India hence the present study was conducted with the aim to study use of antimicrobial agents in patients on ventilator in ICU.
Materials and Methods
The study was continuous, prospective, longitudinal and observational conducted at medical, surgical and neurosurgical intensive care unit (ICUs) at tertiary care teaching hospital, Ahmedabad, India for a period of October 2009 to August 2011 (23 months). A study approval was taken from Institutional Ethical Committee (Ref No. EC/Approval/38/10) and Medical Superintendent of institute before starting the study. Investigator visited ICU in the pre defined order every day between 9 and 11 am. Adult patients who were admitted and prescribed antimicrobial agents were included in study. All informations were collected and recorded in the pre formed Case Record Form (CRF). The data were analysed at the end of study by Z and x2 test.
Results
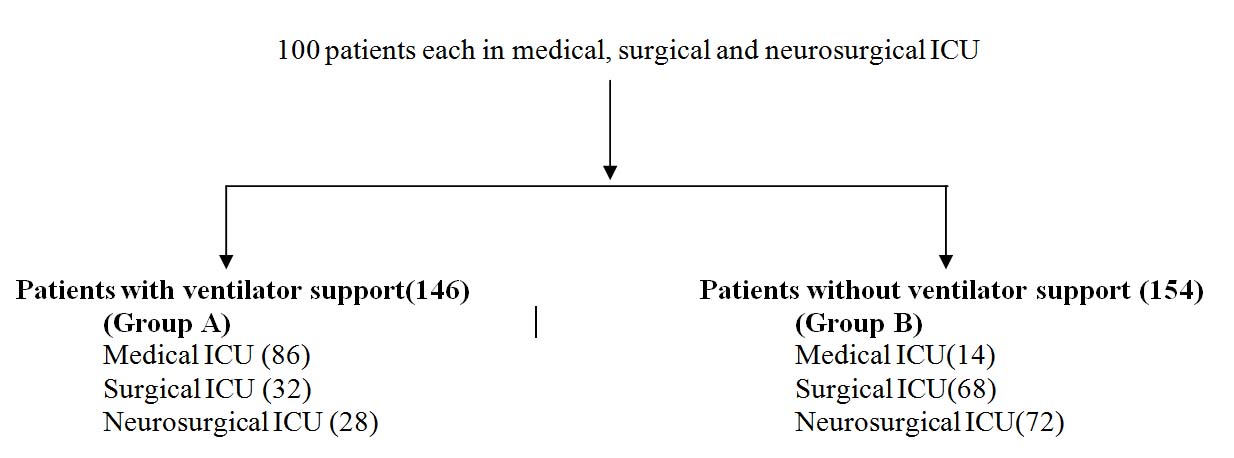
Total 300 patients (100 patients/ ICU) admitted in ICU were prescribed antimicrobial agents and were studied during for 23 month. All patients were followed up till their hospitalization in the ICU. Patients were divided in two groups [Table/Fig-1].
Group of patients admitted in ICU (n=300)
Majority of patients were within 51-60 age group and male patients were higher as compared to female in both groups. It was observed that duration of stay and mortality were significantly higher in group A as compared to group B. It was reported that average number of antimicrobials prescribed was significantly higher in group A as compared to group B. There was statistical significance in prescribing antimicrobial agents by intravenous (IV) route and generic name as compared to other route (s) of administration and brand name respectively in both groups. Number of antimicrobial agents prescribed empirically were significantly higher in group B as compared to group A. There was no significant difference observed in prescribing antimicrobial agents according to WHO, National and State EML in both groups [Table/Fig-2].
Analysis of outcome and prescribed drug therapy in both groups
| Observed parameter | Group A | Group B |
|---|
| Duration of stay in ICU in days (Mean±SEM) | 12.4±1.33* | 8.23±1.21 |
| Mortality observed (%) | 91.70* | 11.03 |
| Average number of drugs prescribed (Mean±SEM) | 14.11±1.34 | 12.24±1.19 |
| Number of drugs prescribed by generic name(%) | 1286(62.38)** | 1232(65.32)** |
| Number of drugs prescribed by brand name (%) | 775(37.62) | 654(34.68) |
| Average number of antimicrobial agents (Mean±SEM) | 4.02±1.81 | 3.38±1.23 |
| Route of administration | IV (%) | 541(92.16)# | 503(96.36)# |
| IM (%) | 8(1.36) | 1 (0.20) |
| Oral/ Ryle’ s tube (%) | 32 (5.45) | 9 (1.72) |
| Topical (%) | 6 (1.03) | 9 (1.72) |
| Number of antimicrobial agents prescribed by generic name (%) | 358 (60.98)** | 360 (68.96)** |
| Number of antimicrobial agents prescribed by brand name (%) | 229 (39.02) | 162 (31.04) |
| Number of antimicrobial agents prescribed by empirically (%) | 442 (75.29) | 430 (82.37)## |
| Number of antimicrobial agents prescribed from WHO Essential Medicine List (%) | 369 (62.86) | 331(63.40) |
| Number of antimicrobial agents prescribed from National and State Essential Medicine List (%) | 419 (71.37) | 387 (72.41) |
*p<0.05 (Z test ) significantly different as compared to group A; ** p<0.05 (x2 test) significantly different as compared to brand name; #p<0.05 (Z test ) significantly different as compared to other route(s) of administration; ## p<0.05 (x2 test) significantly different as compared to group B
Analysis of antimicrobial agents prescribed
Piperacillin+tazobactam, levofloxacin, ceftriaxone, ciprofloxacin and antitubercular agent were prescribed significantly higher in group A as compared to group B. There was statistical significance observed in prescribing cefotaxime, ceftazidime, amikacin and metronidazole in group B.
Antimicrobial agents prescribed according to antimicrobial policy
Analysis of prescribed antimicrobial agents according to antimicrobial policy of hospital revealed that unrestricted antimicrobial e.g levofloxacin, ceftriaxone, ciprofloxacin and antitubercular agents were prescribed significantly higher in group A as compared to group B while cefotaxime, ceftazidime, amikacin and metronidazole were prescribed significantly higher in group B as compared to group A. Restricted antimicrobials e.g. piperacillin + tazobactam, cefoperazone + sulbactam were prescribed significantly (p<0.05) higher in group A as compared to group B while linezolid was prescribed significantly (p<0.05) higher in group B as compared to group A [Table/Fig-3a,b].
Analysis of unrestricted antimicrobial agents according to antimicrobial policy
| Sr. No. | Group of antimicrobial agents | Name of antimicrobial agents | Group A (n=458) | Group B (n=455) |
|---|
| 1. | Penicillin | Crystalline penicillin | - | 3 |
| Amoxicillin-Clavulanate | 46 | 39 |
| 2. | Cephalosporin | Cefoperazone | - | 6 |
| Cefotaxime | 28 | 46** |
| Ceftriaxone | 63* | 28 |
| Cefatazidime | 8 | 27** |
| Cefixime | - | 4 |
| 3. | Fluroquinolones | Ciprofloxacin | 18* | 6 |
| Ofloxacin | - | 11 |
| Levofloxacin | 95* | 17 |
| Gatifloxacin | - | 2 |
| 4. | Aminoglycoside | Amikacin | 73 | 125** |
| Streptomycin | 8* | 1 |
| Neomycin +polymyxin | - | 6 |
| 5. | Macrolides | Azithromycin | - | 4 |
| 6. | Nitroimidazole | Metronidazole | 87 | 117** |
| 7. | Antituberuclar | Isoniazid | 8* | 1 |
| Rifampicin | 8* | 1 |
| Pyrizinamide | 8* | 1 |
| Ethambutol | 8* | 1 |
| 8. | Antihelmintic | Albendazole | - | 1 |
| 9. | Antifungal | Fluconazole | - | 6 |
| Acyclovir | - | 2 |
Analysis of restricted antimicrobial agents according to antimicrobial policy
| Sr. No. | Group | Name of antimicrobial agent | Group A (n=129) | Group B (n=67) |
|---|
| 1. | Penicillins | Piperacillin +tazobactam | 49* | 9 |
| 2. | Cephalosporins | Cefoperazone+sulbactam | 70* | 33 |
| 3. | Carbapenem | Imipenem | - | 1 |
| Imipenem+cilastin | 1 | 1 |
| 4. | Macrolides | Vancomycin | - | 5 |
| Linezolid | 9 | 16** |
| Clindamycin | - | 2 |
*p<0.05 (Z test) significantly different as compared to group B; **p <0.05 (Z test) significantly different compared to group A
Analysis of Culture Sensitivity Test (CST)
It was observed that 74 and 55 samples were collected for CST from 52 and 35 patients in group A and group B respectively. Organisms were isolated in 34 samples in group A and 19 sample in group B. No organism was isolated all remaining samples. Pseudomonas areuginosa and Kleibsella were most commonly isolated in group A compared to group B [Table/Fig-4].
Analysis of organism isolated from samples (n=53)
| Sr. No. | Organism identified | Group A n= 34 (%) | Group B n= 19 (%) | Total n=53 (%) |
|---|
| 1. | S. aureus | 4 (11.76) | 3 (15.78) | 7 (13.20) |
| 2. | Methicillin Resistant S. aureus (MRSA) | - | 1 (5.26) | 1 (1.88) |
| 3. | Acinetobacter | 3 (8.82) | - | 3 (5.66) |
| 4. | P. areuginosa | 14 (41.17) | 5 (26.31) | 19 (35.84) |
| 5. | Kleibsella | 12 (35.29) | 3(15.78) | 15 (28.30) |
| 6. | E coli | 1 (2.94) | 2 (10.52) | 3 (5.66) |
| 7. | Enterococcus | - | 1 (5.26) | 1 (1.86) |
| 8. | Candida albicans | - | 4 (21.05) | 4 (7.54) |
Out of 7 strains of Staphylococcus aureus, resistance to penicillin and its combination with beta lactamase inhibitor were observed in 2 (50%) strains in group A and 1 strain (33%) in group B. MRSA was found in one sample from group B and it was sensitive to only to vancomycin and linezolid. Two strain (66%) of Acinobacter from group A were sensitive only to piperacillin+tazobactam and levofloxacin and resistant to all other antimicrobial agents.
In group A resistance to penicillin and cephalosporin were observed in 13 (92.85%) strain of Pseduomonas aeruginosa and 11 (91.66%) strain of Kleibsella and resistance to penicllin and cephalosporins in combinations with beta lactamase inhibitors were observed in 5 (35.71%) strain of Pseduomonas aeruginosa and 5 (41.66%) strain of Kleibsella. It was reported that levofloxacin, moxifloxacin, imipenem, imipenem+cilastin, meropenem were sensitive to all strains of Pseduomonas aeruginosa and Kleibsella. There was statistically significant difference for resistant pattern of antimicrobial agents between group A and B [Table/Fig-5].
Resistance pattern of antimicrobial agents to microorganisms,
| Sr. No. | Staphylococus aureus | MRSA | Acinobacter | Pseudomonas aeruginosa | Kleibsella |
|---|
| Group A | Group B | Group B | Group A | Group A | Group B | Group A | Group B |
|---|
| Amoxicillin | 50 | 33.33 | 100 | 66.66 | 92.85* | 40 | 91.66* | 33.33 |
| Ampicillin +clavulinic acid | 50 | 33.33 | 100 | 66.66 | 35.71* | - | 41.66* | - |
| Amoxicillin | 50 | 33.33 | 100 | 66.66 | 92.85* | 40 | 91.66* | 33.33 |
| Amoxicillin +clavulinic acid | 50 | 33.33 | 100 | 66.66 | 35.71* | - | 41.66* | - |
| Piperacillin | 50 | 33.33 | 100 | 66.66 | 92.85* | 40 | 91.66* | 33.33 |
| Piperacillin +tazobactam | 50 | 33.33 | 100 | - | 35.71* | - | 41.66* | - |
| Cefazolin | - | - | 100 | 66.66 | 92.85* | 40 | 91.66* | 33.33 |
| Cefaclor | - | - | 100 | 66.66 | 92.85* | 40 | 91.66* | 33.33 |
| Ceftazidime | - | - | 100 | 66.66 | 92.85* | 40 | 91.66* | 33.33 |
| Cefotaxime | - | - | 100 | 66.66 | 92.85* | 40 | 91.66* | 33.33 |
| Cefotaxime+sulbactam | - | - | 100 | 66.66 | 35.71* | - | 41.66* | - |
| Ceftriaxone | - | - | 100 | 66.66 | 92.85* | 40 | 91.66* | 33.33 |
| Ceftriaxone +sulbactam | - | - | 100 | 66.66 | 35.71* | - | 41.66* | - |
| Cefoperazone | - | - | 100 | 66.66 | 92.85* | 40 | 91.66* | 33.33 |
| Cefoperazone +tazobactam | - | - | 100 | 66.66 | 35.71* | - | 41.66* | 50 |
| Cefepime | - | - | 100 | 66.66 | 92.85* | 40 | 91.66* | 33.33 |
| Levofloxacin | - | - | 100 | - | - | - | - | - |
| Amikacin | - | - | 100 | 66.66 | 92.85* | 40 | 91.66* | 33.33 |
| Azithromycin | - | - | 100 | 66.66 | 92.85* | 40 | 91.66* | 33.33 |
| Vancomycin | - | - | - | 66.66 | 35.71* | - | 41.66* | - |
| Linezolid | - | - | - | 66.66 | 35.71* | - | 41.66* | - |
| Tetracycline | - | - | 100 | 66.66 | 92.85* | 40 | 91.66* | 33.33 |
| Chloramphenicl | - | - | 100 | 66.66 | 92.85* | 40 | 91.66* | 33.33 |
| Co trimoxazole | - | - | 100 | 66.66 | 92.85* | 40 | 91.66* | 33.33 |
Value (-) express 0% resistance or 100% sensitive; * p<0.05 (Z test) significantly different as compared to group B
Four strain of S aureus (2 in each group), one strain of Acinobacter (group A), four strain of Pseduomonas aeruginosa (3 in group A, 1 in group B), 3 strain of Kleibsella. (1 in group A ,2 in group B) and 8 strain of others (Candida albicans, E.coli and Enterococcus) were sensitive to all the antimicrobial agents.
Addition or change of antimicrobial agent without CST
Number of antimicrobial agents added without CST was significantly higher in group A (17.37%) as compared in group B (7.68%). Amoxicillin+clavulinic acid, piperacillin+ tazobactam, cefotaxime, ceftriaxone, cefoperazone + sulbactam, levofloxacin and amikacin were added without CST.
Change of antimicrobial treatment after CST
CST was carried out in 52 and 35 patients in group A and group B respectively. Change of antimicrobial therapy after CST was significantly higher in 28 (53.84%) patients in group A as compared to 5(14.28%) patients in group B. Amoxicillin+clavulinic acid piperacillin+tazobactam, cefoperazone+ sulbactam, imipenem, imipenem+cilastin, levofloxacin and vancomycin were prescribed after CST according to sensitivity pattern.
Discussion
The demographic results of our study revealed that majority of the patients were within 51-60 age group in both groups which was similar to a study carried out in Punjab in 2011 [8]. In our study male were higher as compared to female in both groups while Mato et al., from Nigeria reported that there were more female patients admitted in their ICU compared to male [9]. We did not include obstetric patients while study conducted at Nigeria female patients were also studied.
Mortality was significantly higher in group A as compared to group B. In group A patients were admitted for ventilator support and mortality was higher in patients on ventilator due to respiratory failure or complication while majority of the patients in group B were admitted for post operative period [7]. Mean duration of stay in hospitalization was significantly higher in group A as compared to group B. As patients in group A were on ventilator support required longer duration of monitoring while patients in group B were admitted for post operative care and they were discharged in 4 to 5 days from ICU.
It was observed that average number of drugs prescribed per patient was 14.12 ± 1.34 and 12.24 ± 1.19 in group A and B respectively which was similar to study carried out by John et al., where average drug was 11.6 ± 2 [10]. In the ICU, critically ill patients and due to co morbid condition polypharamacy was prescribed [11].
More than 60% drugs were prescribed generically in both groups which was higher as compared to study from Banglore where 30% drugs were prescribed by generic name in their ICU [10]. It was observed that above 60% antimicrobial agents were prescribed generically in both groups. Antimicrobial agents were prescribed by generic name significantly higher as compared to brand name prescription. The probable reason for generic prescription is our hospital being tertiary care teaching hospital and drugs were supplied from the Central Medical Store Organization (CMSO), Government of Gujarat. Drugs were prescribed by brand name in unavoidable circumstance and they were not available from the hospital.
Average number of antimicrobials prescribed was significantly higher as compared to other route(s) of administration. Above 90% antimicrobial agents were prescribed by IV route in both groups while study in the hospital of Israel 64% of antimicrobials were prescribed parenterally [12]. Duration of antimicrobial therapy was significantly higher in group A as compared to group B. Study conducted at Manglore revealed that average duration of antimicrobial therapy was 6 days [13]. Patients were admitted in ICU in our study either critical condition or in postoperative period and required longer duration of antimicrobial therapy.
In all the patients antimicrobial agents were started empirically which was similar to study conducted by Williams et al., who reported that 95% patients were prescribed antimicrobial agents empirically [8]. Biswal et al., reported that 62% patients were prescribed antimicrobial agents empirically in tertiary care unit in Northern India which were lower as compared to our study [14]. Antimicrobial agents prescribed empirically are unrestricted antimicrobial agents as per antimicrobial policy of our hospital. It was observed that above 60% antimicrobials were prescribed according to WHO EML in all ICU while approximately 70% antimicrobials were prescribed according to National and State EML. Our study was conducted at tertiary care teaching hospital and antimicrobial agents were supply from CMSO.
Piperacillin+tazobactam,cefoperazone+sulbactam,levofloxacin and ciprofloxacin were prescribed significantly higher in group A as compared to group B. The reason for that hospital acquired pneumonia and ventilated associated pneumonia (VAP) are most commonly occurred in patient on mechanical ventilation in ICU and multi drug resistant organisms gram negative bacilli were the commonest respiratory pathogens responsible for increased mortality in patients of VAP [7]. Only 5 drugs (ceftazidime, ciprofloxacin, levofloxacin, linezolid and piperacillin+tazobactam) received FDA approval for use in nosocomial pneumonia [5].
Ceftazidime and cefotaxime were prescribed significantly higher in group B as compared to group A while ceftriaxone was prescribed significantly higher in group A as compared to group B. This is due to ceftazidime, cefotaxime and ceftriaxone were used most commonly as empirical therapy in their respective groups. There was statistically significant difference observed in prescribing amikacin and metronidazole in group B as compared to group A. As in group B majority of patient admitted after operative procedures and post operative patient have risk of developing gram negative and anaerobic infection [15]. As amikacin effective against abdominal enterobacteria and metronidazole effective against anaerobes they were prescribed higher in group B as compared to group A [16].
Anti-tubercular agents were prescribed significantly higher in group A as compared to group B because patients suffering from tuberculosis with critical condition were referred for ventilator support. Carbapenem was not frequently prescribed in both groups while in contrast to study from Latin America reported that carbapenem (22%) was most commonly prescribed antimicrobial agent which was higher as compared to our study [17]. Carbapenem is not supply from CMOS as it is not included in EML and sensitivity to other antimicrobial agents is present in our set up.
Pseudomonas aeruginosa (35.84%), Kleibsella (28.30%) and Staphylococcus aureus (13.20%) were most common microorganism isolated in both groups in contrast to study from USA by Lawton RM reported that 6.4%, Kleibsiella species, 6.4% Staphylococcus aureus and 5%, Pseudomonas aeruginosa were isolated from the ICU which was lower as compared to our study [18]. The probable reason for that the frequency and types of infection vary among different ICUs.
In group A 50% of Staphylococcus aureus strain resistant to penicillin was observed while 33.33% strains in group B. European and North American surveillance study reported that resistant to penicillin by Staphylococcus aureus was observed 93.3%, 87.4%, 94.4% 83.8% and 93.3% in ICU of Unites states, Canada, Italy, Germany and France respectively [19]. Penicillin in combinations with beta lactamase inhibitors were prescribed highly as compared to penicillin alone in our set up. In our study strain of MRSA was found in group B and it was sensitive to vancomycin and linezolid similar reports also observed in study at Hyderabad where MRSA was sensitive to vancomycin [20].
Out of 2 strain of Acinobacter in group A, they were sensitive only to piperacillin+tazobactam and levofloxacin while study from USA reported that there was decrease response to piperacillin+tazobacatam in their ICU. This is may be due to higher use of piperacillin+tazobactam in their ICU [21].
Out of 14 strain of Pseduomonas aeruginosa from group A, resistance to amoxicillin, ampicillin, piperacillin, cefoperazone, cefotaxime, ceftriaxone, amikacin were observed in 13 (92.85%) strain which was higher as compared to 2 (40%) strain in group B and also study of Irdem et al., reported that Pseudomonas was resistance ceftazidime (59%), imipenem(32%) ciprofloxacin (62%), piperacillin+tazobactam (41%), amikacin (16%) in patients on ventilator [22]. It was observed that levofloxacin, moxifloxacin, imipenem, imipenem+cilastin, meropenem were sensitive in 5 (35.71%) strains while study at Rohtak reported that meropenem( 22.8%) resistant to Pseduomonas aeruginosa [23].
Out of 12 strains of Kleibsella, from group A, resistance to amoxicillin, ampicillin, piperacillin, cefoperazone, cefotaxime, ceftriaxone, amikacin were observed in 11 (91.66%) strains as compared to 1 (33.33%) strains in group B but similar reports also observed in study at Banglore where ampicillin (98.7%), piperacillin(91.8%), cephazoline (94.3%), ceftazidime (90.5%) cefotaxime (90.5%) ceftriaxone (89.1%) cefotaxime (90%) ciprofloxacin (65.8%) amikacin (23.1%) resistant to Kleibsella [24]. It was observed that levofloxacin, moxifloxacin, imipenem, imipenem+cilastin, meropenem were sensitive in 6(50%) samples while study at Rohtak reported that meropenem (9.1%) resistant was found to Kleibsella [23].
Addition or change of antimicrobial agents without CST was significantly higher in group A as compared in group B as average stay duration in ICU was higher in patient on ventilator so there was more cycling of antimicrobial agents was done.
CST was carried out in 52 and 35 patients in group A and group B respectively. Change of antimicrobial therapy after CST was significantly higher in 28 (53.84%) patients in group A as compared to 5(14.28%) patients in group B. This is due to antimicrobial resistance was observed higher in patients on ventilator.
Antimicrobials are widely prescribed empirically in both groups. Resistance to penicillin, cephalosporins, amikacin is observed and antimicrobial resistance to Pseudomonas and Kleibsella is seen in higher number of patients in group A as compared to group B. Although antimicrobial policy of the Hosptial is available but some of the restricted antimicrobial agents are used significantly in higher number of patients. Hence, to improve rational use of antimicrobial agents following suggestions are:
Education of prescriber by seminar, medical workshop etc.
Availability of antimicrobial policy in every unit, ward including ICU, operation theatre and to every prescriber
Strict monitoring of antimicrobial policy and procurement by policy makers
Limitation of our study that we did not study the use of antimicrobial agents according diagnosis and site of infection and did not include pediatric and pregnant female patients.
Conclusion
Antimicrobial agents are widely prescribed in ICU. Although restricted antimicrobial agents in antimicrobial policy in our set up, they are significantly prescribed in patients on ventilator. This study will helpful for education to prescribers, rational prescription of antimicrobials and better management of patients.
*p<0.05 (Z test ) significantly different as compared to group A; ** p<0.05 (x2 test) significantly different as compared to brand name; #p<0.05 (Z test ) significantly different as compared to other route(s) of administration; ## p<0.05 (x2 test) significantly different as compared to group B