Evaluation of Bowel Wall Thickening by Computed Tomography to Differentiate Benign from Malignant Lesions
Chaitanya Tapasvi1, Neeraj Prajapati2, Rajneesh Madhok3, Ashish K. Gupta4, Vichi Taneja5, Abhinav Aggarwal6
1Assistant Professor, Department of Radiology, SRMS Institute of Medical Sciences, Bareilly-Nainital Road, Bareilly (UP), India.
2Assistant Professor, Department of Radiology, SRMS Institute of Medical Sciences, Bareilly-Nainital Road, Bareilly (UP), India.
3Professor and Head, Department of Radiology, SRMS Institute of Medical Sciences, Bareilly-Nainital Road, Bareilly (UP), India.
4Assistant Professor, Department of Radiology, SRMS Institute of Medical Sciences, Bareilly-Nainital Road, Bareilly (UP), India.
5Resident, Department of Radiology, SRMS Institute of Medical Sciences, Bareilly-Nainital Road, Bareilly (UP), India.
6Resident, Department of Radiology, SRMS Institute of Medical Sciences, Bareilly-Nainital Road, Bareilly (UP), India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Chaitanya Tapasvi, C-4, Doctors Residence, SRMS Institute of Medical Sciences Campus, Bareilly-Nainital Road, Bareilly (UP), India. Phone : 7500847855
E-mail: chaitanyatapasvi@yahoo.com
Purpose: Computed tomography(CT) is an excellent non-invasive modality to evaluate bowel wall thickening.The aim of our study was to evaluate CT appearance of bowel wall thickening due to various benign and malignant conditions taking into consideration pattern of attenuation, bowel wall thickness, extent of lesion, symmetry of lesion and other associated CT findings.
Materials and Methods: The prospective study was carried out on 50 patients who underwent computed tomographic evaluation of abdomen for suspicion of bowel pathology based on ultrasonography, barium studies and/or clinical grounds. The studies were conducted on Siemens ART and GE High speed CT scanners. The examination was performed as is done routinely for an abdominal scan with imaging done from diaphragm to pubic symphysis in supine position with the right lateral decubitus scans in selected cases for better characterization of gastric antral and duodenal lesions. Oral, rectal and intravenous (IV) contrast agents were administered. The diagnosis was confirmed by cytology or histopathology of any biopsy or surgical specimen. However, in cases where surgery was not done, diagnosis was confirmed by clinical response to medical treatment.
Results: Based on the various CT characteristics of abnormal bowel wall thickening, sensitivity and specificity of classifying a lesion as benign or malignant were calculated. Majority of the malignant bowel lesions were showing the following characteristics i.e. heterogeneous pattern of enhancement, marked bowel wall thickening, asymmetry of the lesion and focal/segmental bowel involvement. Overall, CT showed a sensitivity of 97% and specificity of 93% in differentiating between benign and malignant etiology of abnormal bowel wall thickening.
Conclusion: Due to its high sensitivity and specificity, CT is an ideal imaging modality for differentiating between benign and malignant etiology of abnormal bowel wall thickening. Radiologists should be aware of the usefulness of specific CT criteria of bowel wall thickening to better differentiate benign lesions from malignant or potentially malignant lesions that warrant further diagnostic evaluation.
Asymmetry of lesion, Focal/segmental bowel involvement, Heterogeneous enhancement, Marked bowel wall thickening
Introduction
Computed tomography (CT) has become a versatile tool in assessing the gastrointestinal (GI) tract. It provides accurate information about the wall of the gut and surrounding structures. The GI tract can be difficult to evaluate because it is actively peristalting [1]. Multidetector CT (MDCT) makes possible the acquisition of isotropic data and affords the capability of performing high resolution multiplanar reconstructions [2]. 3-D interactive workstations and advanced software have considerably improved lesion conspicuity and even provide virtual endoscopy of bowel. Applications that were once routinely performed with barium studies (e.g. evaluation of suspected small bowel obstruction) or angiography (e.g. evaluation of mesenteric ischemia) now have been replaced with CT scans [3]. CT cannot demonstrate subtle superficial mucosal changes revealed on barium studies, but is a highly sensitive method for detection of intramural disease and extramural extension of colonic disease [4]. In particular, CT enterography acquired after luminal distension through the administration of high volumes of neutral contrast material (1,500-2,000ml of water, water-methylcellulose solution, polyethylene glycol electrolyte solution or low-concentration barium) is helpful in displaying the thickness and enhancement of the small bowel wall [2,5] Presently, CT is considered a first-line modality for evaluation of a variety of small bowel diseases [3]. A wide spectrum of intestinal wall morphologic and enhancement abnormalities can be seen with bowel disorders which include normal variants,inflammatory conditions and neoplastic disease. Once an abnormality is detected the radiologist needs a systematic approach for determining the specific cause of the intestinal abnormality. The aim of study was to differentiate benign and malignant conditions of bowel wall thickening taking into consideration pattern of attenuation, bowel wall thickness, extent of lesion (focal, segmental or diffuse involvement), symmetry of lesion and associated perienteric abnormalities.
Materials and Methods
The prospective study was carried out on 50 patients who underwent computed tomographic evaluation of abdomen for suspicion of bowel pathology based on ultrasonography, barium studies and/or clinical grounds. The cases included were those of abnormal bowel wall thickening (>5mm wall thickness when adequately distended), large masses focally involving the bowel wall primarily and cases with segmental or diffuse involvement of the bowel wall. No selection bias was exercised on the basis of age or sex. The studies were conducted on Siemens ART and GE High speed CT scanners. The examination was performed as is done routinely for an abdominal scan (in breathhold) with imaging done from diaphragm to pubic symphysis in supine position with the right lateral decubitus scans in selected cases for better characterization of gastric antral and duodenal lesions. Oral and intravenous (IV) contrast agents were administered in all cases (except in cases of suspected intestinal obstruction where oral contrast was not given). 750ml of positive oral contrast material was administered 45 minutes prior to the examination to opacify the bowel loops. Another 250ml of oral contrast was given to the patient just before the start of examination for adequate distension of stomach. The oral contrast material used was flavoured 76% w/v iodine based contrast, diluted in one litre of water. Many prefer to use negative oral contrasts such as water or Volumen [6]. Patients with allergies to iodine that require positive oral contrast received dilute barium. Patients with suspected bowel obstruction did not require oral contrast because they usually have air and fluid within the bowel to provide negative contrast. Positive contrast agents containing 76% w/v iodine diluted in one litre of water were administered via rectum in cases suspected for colonic pathology or in patients with unopacified bowel loops in pelvis.Non-ionic iodinated contrast materials were preferred for IV administration (typical dose 100ml of Omnipaque 350, children 2-2.5ml/kg of IV contrast medium) [7]. The diagnosis as benign or malignant lesion was confirmed by cytology or histopathology of any biopsy or surgical specimen. However, in cases where surgery was not done, diagnosis was confirmed by clinical response to medical treatment. The imaging characteristics were recorded in all patients and their management and final diagnosis documented.
Results
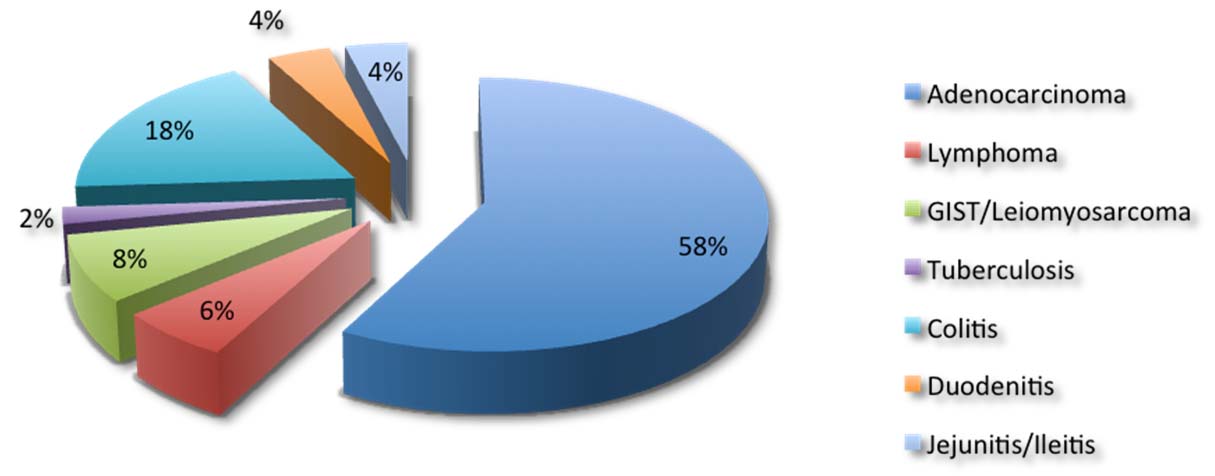
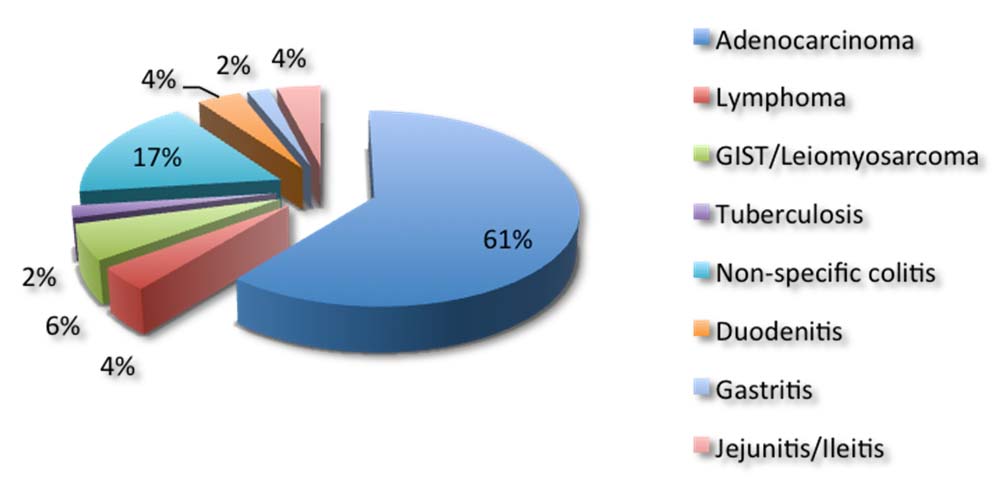
Our study consisted of 50 patients, the youngest being of 7 years and oldest being of 80 years. There were total of 35 malignant bowel wall lesions and 15 benign cases of bowel wall thickening [Table/Fig-1,2]. Benign causes of bowel wall thickening were noted to be commoner in the below 60 years group making 14 (93.3%) out of 15 cases. Malignant causes of bowel wall thickening were noted in much older patients with 23 (65.7%) out of 35 cases seen in patients with more than 40 years of age. No definite sex predilection of benign or malignant lesions was noted. Abdominal pain was the commonest symptom in the benign group (in 13 out of 15 patients) while anorexia/weight loss was the commonest complaint in the malignant group (in 33 out of 35 patients). Of the total 50 cases, 7 cases involved the stomach, in 13 cases there was small bowel involvement while in 30 cases there was involvement of the large intestine. Certain lesions that were extending into the adjacent segment of bowel were classified into the category where the major length of abnormality was seen. Also,lesions involving the terminal ileum and caecum were considered in large bowel distribution. Of all attenuation patterns, white attenuation was seen in three cases of benign bowel wall thickening and none of the malignant lesions showed this type of intense attenuation, thus making it 100% specific for the benign lesions. Fat halo pattern was seen in a single case in benign group. Water Halo pattern was noticed in 5 cases; out of which 4 were in the benign group. A single lesion which showed the water halo attenuation in malignant series was a case of lymphoma in a 23 years old female patient. None of the adenocarcinoma cases showed water halo attenuation pattern. Thus, the specificity and sensitivity of water halo attenuation in predicting the benignity of a lesion was highly specific with a specificity of 96% but, a dismal sensitivity of 27%. Heterogeneous enhancement pattern was seen in total 23 cases; out of which in 20 cases, the cause of bowel wall thickening was malignant, thereby making this attenuation pattern a specific marker for the malignant lesions [Table/Fig-3]. Mild bowel wall thickening was a sensitive marker for picking up a pathology but not that specific; on the other hand, marked thickening of bowel wall(noted in 24 out of 25 malignant cases) was a specific marker for malignant lesion but not as sensitive [Table/Fig-3]. Asymmetrical bowel wall thickening(seen in total 34 cases; out of which in 29 cases, the cause of bowel wall thickening was malignant) was having good sensitivity and specificity for malignancy [Table/Fig-3]. Focal/segmental involvement of bowel wall was highly sensitive for malignancy (in total 26 cases showing focal involvement of bowel, 22 were in malignant group and out of total 17 cases showing segmental involvement of bowel, 12 were in malignant group) [Table/Fig-3]. Gray attenuation pattern was seen in total 18 cases, with 14 cases lying in the malignant group and remaining 4 in the benign group. Thus, gray attenuation was neither a specific nor a sensitive marker for malignancy [Table/Fig-3].Associated CT findings like ulceration, cavitation, necrosis and surrounding fat stranding were also considered. Out of the total 12 cases showing associated ulceration, all cases belonged to the malignant group. All the 5 cases showing associated cavitation belonged to the malignant group. Also, 23 out of total 24 cases showing necrosis were of malignant etiology. Tweleve cases with associated CT finding of fat stranding belonged to the benign group while other 27 cases were having malignant cause. Out of total 50 cases taken in for study, 13 cases showed signs of bowel obstruction with either dilatation of proximal bowel loops, or non passage of contrast beyond the obstructing lesion. Of these 13 cases, 11 cases had malignant etiology as final diagnosis, while other 2 belonged to the benign group. Of the total 50 cases, 4 cases were having free fluid in abdomen. Among these 4 cases, 1 case was in the benign category and other 3 were in the malignant category. Of the 50 cases studied, 35 cases showed lymph node positive status. Amongst malignant group, 25 cases had lymph node size <1cm (short axis diameter) while 6 cases had lymph nodes >1cm in size. In benign group 2 cases each belonged to both the above categories. The sensitivity of lymph node size >1cm in predicting the malignancy status was 17% while specificity was 50%.
Discussion
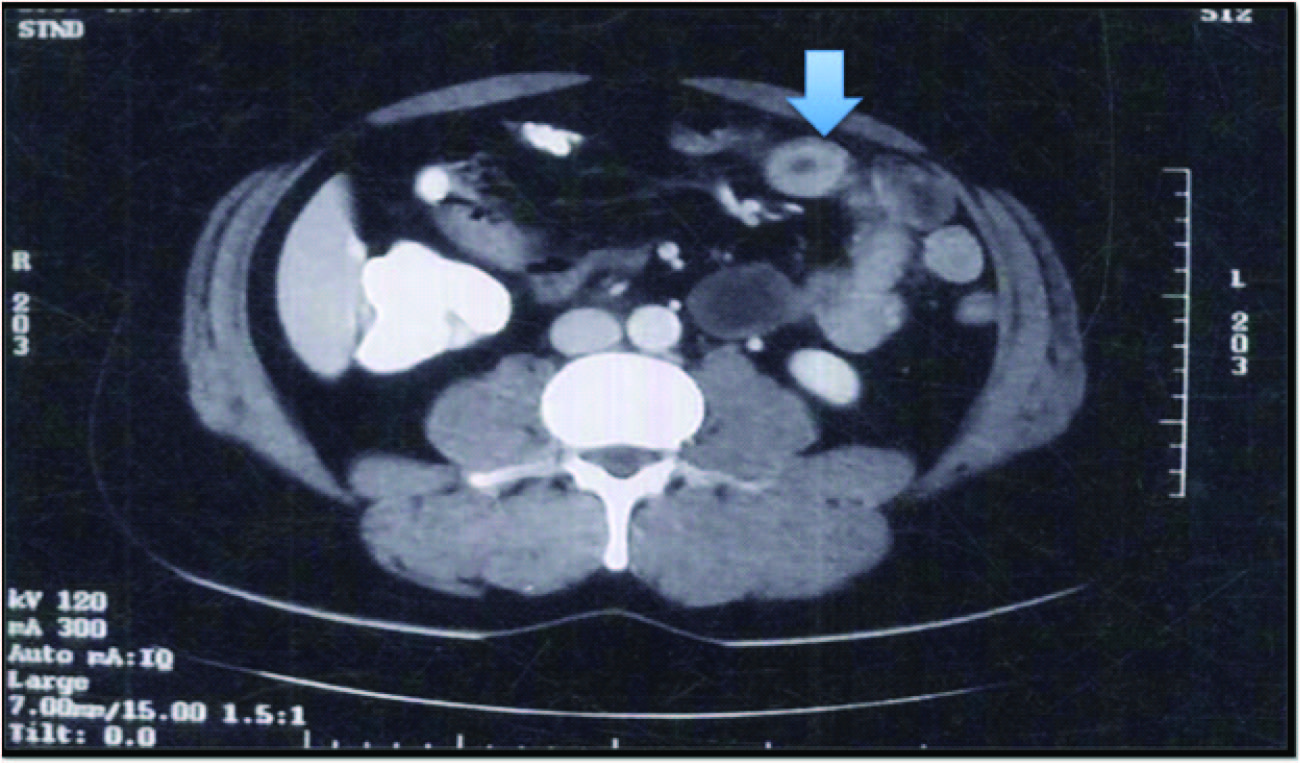
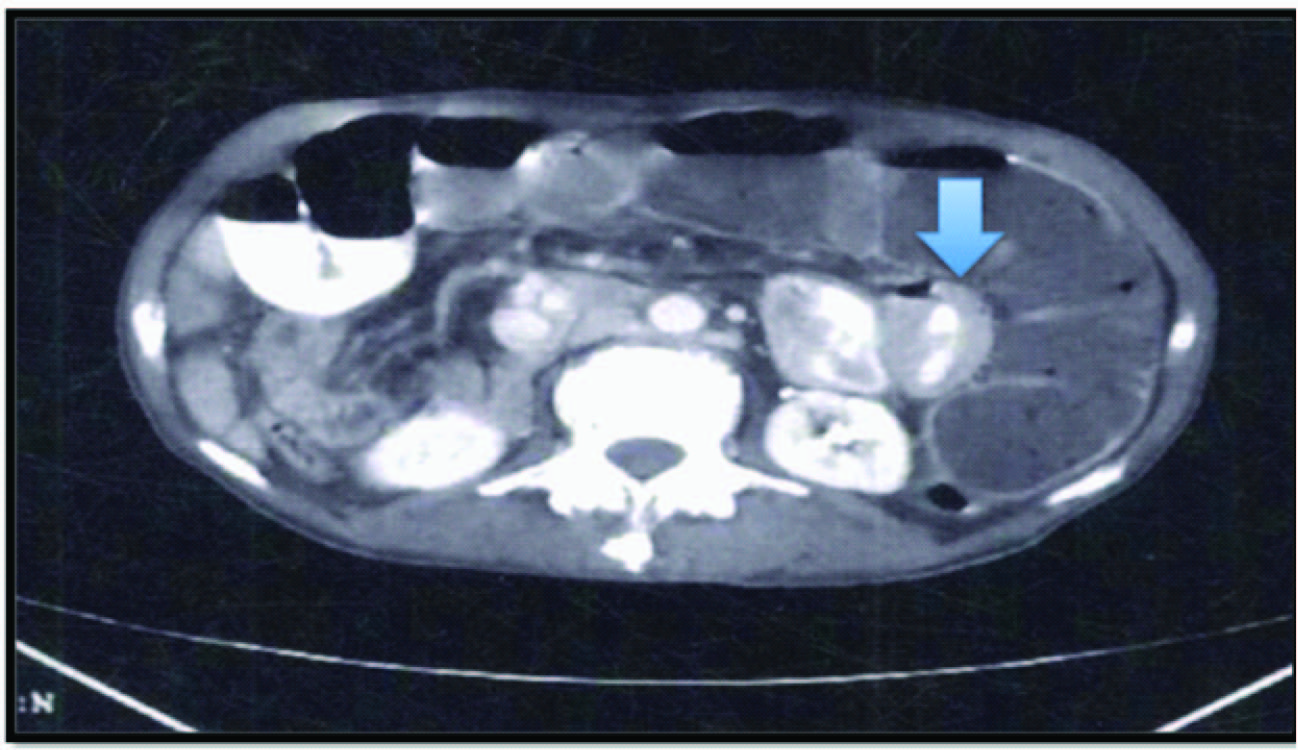
The bowel wall normally enhances after the administration of intravenous contrast material. The mucosa is the most intensely enhancing layer of the bowel wall and when enhanced may appear as a distinct layer. In contrast, the submucosa is less vascularised and is seldom seen as a separate structure on CT scans unless it is oedematous, haemorrhagic or infiltrated by fat [8,2]. If the bowel wall is enhanced to a degree that is equal to or greater than that of venous opacification in the same scan, it should be classified in the white attenuation pattern [9] [Table/Fig-4]. This pattern can be seen mainly in two clinical entities:ischemia and inflammatory bowel disease [2]. The pattern of gray attenuation [Table/Fig-5] is defined as a thickened bowel wall that shows little clear-cut enhancement and whose homogeneous attenuation is comparable with that of enhanced muscle. The pattern of black attenuation is the equivalent of pneumatosis. The common diagnoses in which this attenuation pattern is seen include ischemia, infection and trauma. The water halo sign [Table/Fig-6] is used as a generic term to indicate stratification within a thickened bowel wall that consists of either two or three continuous, symmetrically thickened layers. It is commonly seen in idiopathic inflammatory bowel diseases, vascular disorders, infectious diseases and radiation damage. The pattern of the fat halo sign refers to a three-layered target sign of thickened bowel in which the middle or “submucosal” layer has a fatty attenuation.This sign is commonly seen in crohn’s disease in small intestine and ulcerative colitis or crohn’s disease in the colon . The rare diagnoses in which this pattern occurs include cytoreductive therapy exposure and chronic radiation enteritis [10]. In our study,fat halo sign was seen in a case of duodenitis secondary to pancreatitis [Table/Fig-7]. Bowel wall thickness of 2 cm and less than 2 cm was considered as mild while thickness of more than 2 cm was considered as marked [Table/Fig-8].It was observed that in our study, 14 (93.3%) out of total 15 cases were correctly diagnosed as benign on CT. Also, out of the total 35 malignant cases, 33 (94.3%) cases were correctly diagnosed on CT. Out of these, one case whose probable diagnosis was kept as lymphoma turned out to be adenocarcinoma [Table/Fig-8] and another case of abnormal thickening of pyloric region of stomach, thought to be malignant, turned out to be hypertrophic gastritis. Erik K. Insko et al., [11] in their study of 38 patients of abnormal bowel wall thickening had taken into account 14 malignant and 24 benign cases. Like in our study where bowel wall thickness of more than 2cms had sensitivity and specificity of 69% and 93% respectively; the sensitivity and specificity in the study conducted by Erik K. Insko et al., were 50% and 88% respectively [11]. However, in our study we had divided the lesions into three categories taking into account focal, segmental and diffuse involvement of the bowel wall. It iscentimetres), segmental (10-30 cm), or diffuse (involving most of the small bowel or colon) [8]. If we take the cases segregated under the segmental distribution as focal involvement, the sensitivity and specificity for labelling a lesion as malignant are 97.1% and 40% respectively [Table/Fig-3] which is similar to the distribution shown in the study done by Erik K Insko et al. Similar to the study by Erik K Insko et al., where there were 71% and 29% of the malignant cases showing asymmetrical and symmetrical bowel wall involvement respectively, the congruent figures in our study turned out to be 83% and 17% respectively. For the benign cases, the corresponding figures were 25% and 75% in the study done by Erik K Insko et al., and the percentage involvement in our study were 33% and 67% respectively. In the study conducted by Erik K Insko et al., the authors were very optimistic in the use of CT as the primary modality for the evaluation of bowel wall thickening. The various other parameters apart from marked bowel wall thickening like heterogeneous pattern of enhancement (sensitivity 57%, specificity 80%) [Table/Fig-8,9], asymmetrical bowel wall thickening ( sensitivity 82.8%, specificity 66.7%), and gray attenuation ( sensitivity 40%, specificity 73%) are also useful in characterising a lesion as malignant. Finally, in our study, CT showed a sensitivity of 97% and specificity of 93% in differentiating between a benign and malignant etiology of abnormal bowel wall thickening, which was similar to the conclusion reached by Erik K Insko et al., in their studies.
Sensitivity and specificity of various CT characteristics for labelling a lesion as malignant
| S.No. | CT characteristic | Sensitivity | Specificity |
| 1. | Heterogeneous pattern of enhancement | 57% | 80% |
| 2. | Marked bowel wall thickening (>2cms) | 69% | 93% |
| 3. | Asymmetric bowel wall thickening | 82.8% | 66.7% |
| 4. | Focal/segmental bowel involvement | 97.1% | 40% |
| 5. | Gray attenuation | 40% | 73% |
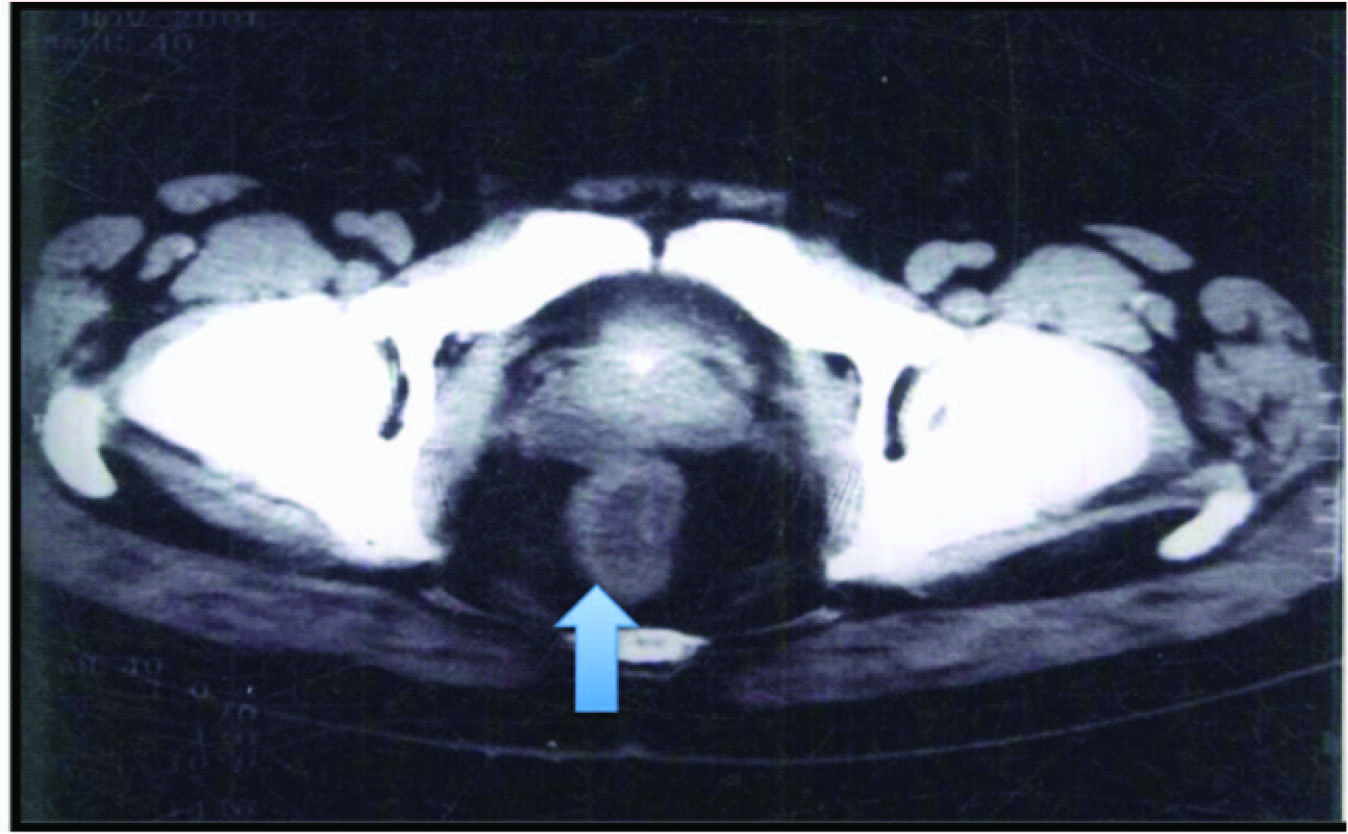
White attenuation - Thickened bowel wall of small intestine showing avid wall enhancement (white attenuation) comparable to the abdominal vessels, in a case of jejunitis
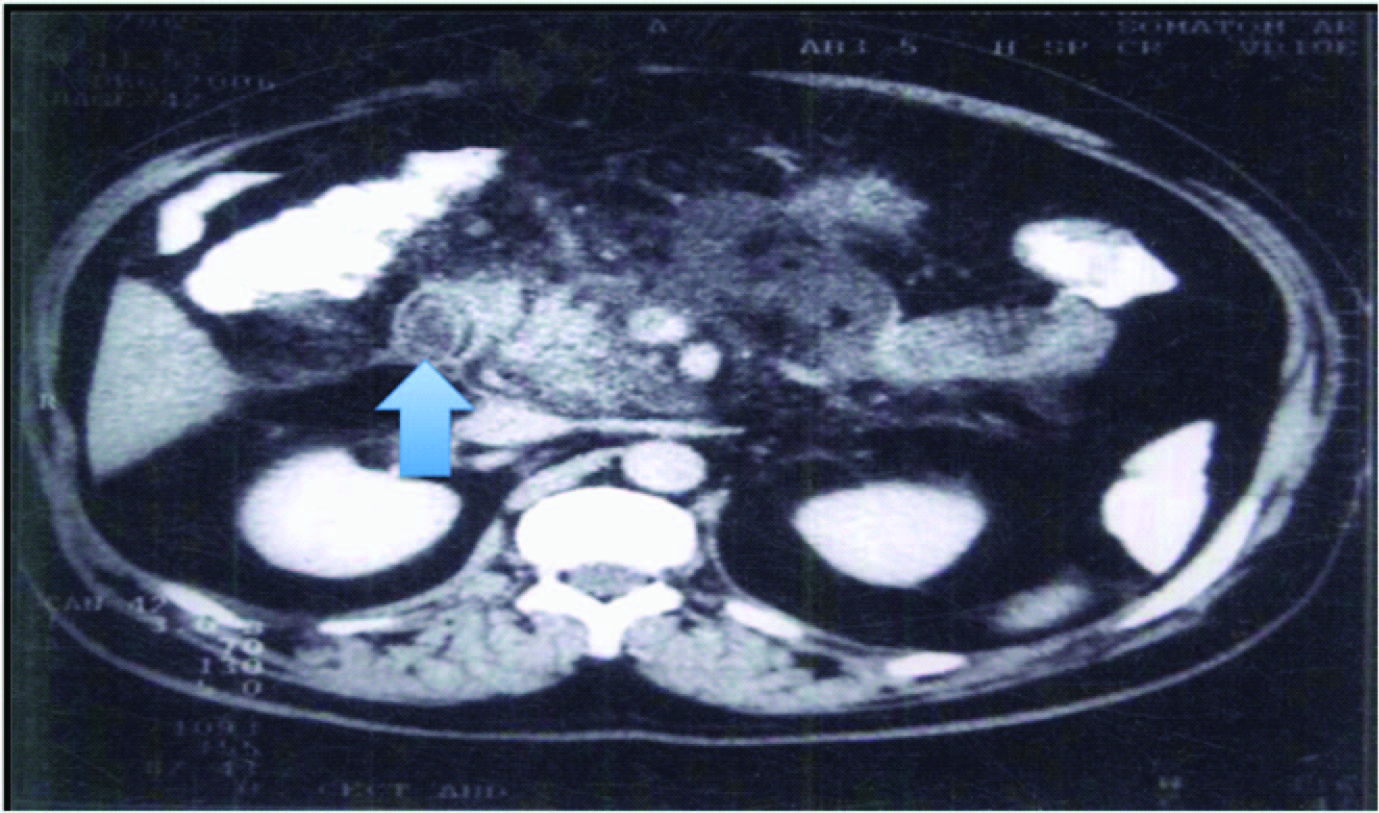
Gray attenuation – Thickened small bowel loops showing homogeneous enhancement comparable to enhanced muscle. There is associated dilatation of colon
Water Halo sign – Rectal wall showing stratified enhancement with higher attenuation of the inner and outer layers compared to low attenuation in the middle layer (submucosa) in a case of proctocolitis with pelvic abscess
Fat halo sign- Mild thickening of the duodenal wall showing negative attenuation in the submucosal layer in a case of inflammation secondary to pancreatitis
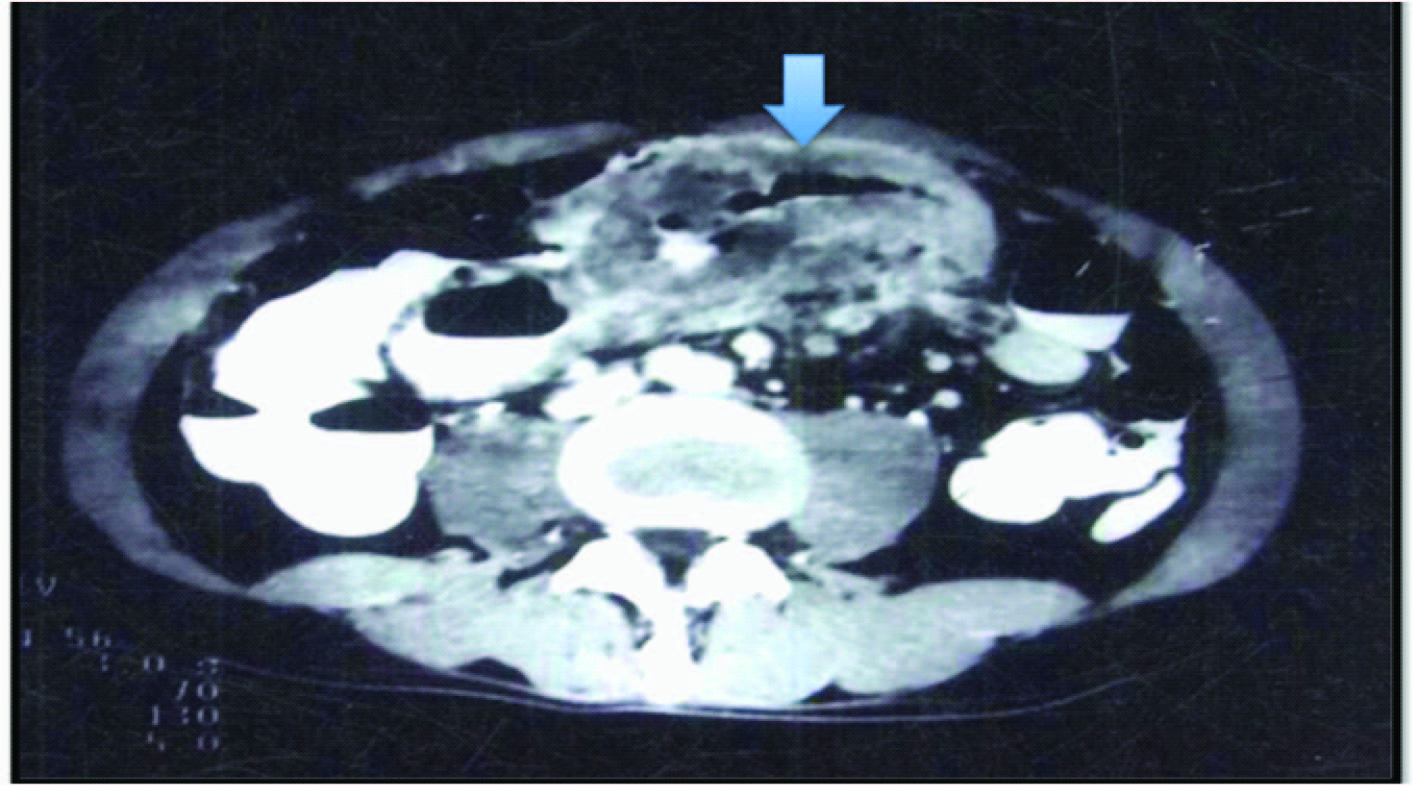
Marked heterogeneous transverse colon wall thickening without luminal narrowing and surrounding lymphadenopathy thought to be lymphoma, was proven to undifferentiated adenocarcinoma on histopathology
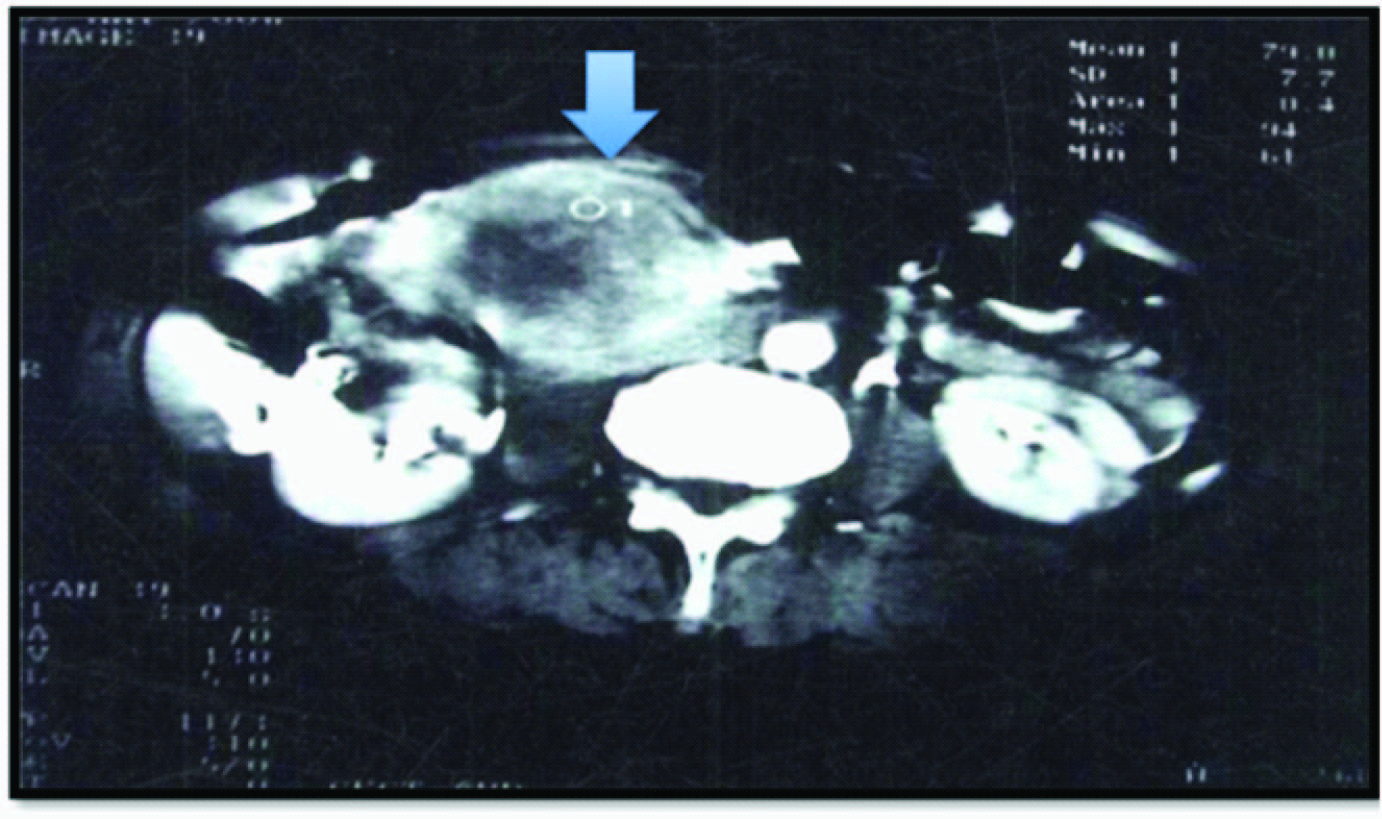
CECT showing eccentric heterogeneously enhancing mass with internal necrotic areas in a case of gastrointestinal stromal tumor
Conclusion
Due to its high sensitivity and specificity, CT is an ideal imaging modality for differentiating between benign and malignant etiology of abnormal bowel wall thickening. The combination of heterogeneous pattern of enhancement, focal/segmental bowel wall involvement, marked bowel wall thickening and asymmetrical lesion leads to very high specificity to label a lesion as malignant. Radiologists should be aware of the usefulness of specific CT criteria of bowel wall thickening for better differentiation of benign lesions from malignant or potentially malignant lesions that warrant further diagnostic evaluation.
[1]. L Canon Cheri, Gastrointestinal tractComputed Body Tomography with MRI Correlation 2006 4:771-828. [Google Scholar]
[2]. T Fernandes, MI Oliveira, R Castro, B Araújo, B Viamonte, R Cunha, Bowel wall thickening at CT: simplifying the diagnosisInsights Imaging 2014 5:195-208. [Google Scholar]
[3]. KM Horton, EK Fishman, The current status of multidetector row CT and threedimensional imaging of small bowelRadiol Clin N Am 2003 41:199-212. [Google Scholar]
[4]. R F Thoeni, J P Cello, CT imaging of colitisRadiology 2006 240:623-28. [Google Scholar]
[5]. SR Paulsen, JE Huprich, JC Fletcher, F Booya, BM Young, JL Fidler, CT enterography as a diagnostic tool in evaluating small bowel disorders: review of clinical experience with over 700 casesRadiographics 2006 26:641-57. [Google Scholar]
[6]. CT Body, CT protocolsDepartment of Radiology,University of California San Diego 2009 :1-26s. [Google Scholar]
[7]. Y Yamashita, AK Komohara, Y Takahashi, M Uchida, N Hayabuchi, T Shimizu, Abdominal Helical CT:evaluation of optimal doses of IV contrast material-a prospective randomized studyRadiology 2000 216(3):718-23. [Google Scholar]
[8]. CK Chou, RH Wu, CW Mak, MP Lin, Clinical significance of poor CT enhancement of the thickened small-bowel wall in patients with acute abdominal painAm J Roentgenol 2006 816(2):491-98. [Google Scholar]
[9]. M Macari, EJ Balthazar, CT of bowel wall thickening : significance and pitfalls of interpretationAm J Roentgenol 2001 176:1105-16. [Google Scholar]
[10]. J Wittenberg, MG Harsinghani, K Jhaveri, Algorithmic Approach to Diagnosis of the abnormal bowel wallRadiographics 2002 22:1093-1107. [Google Scholar]
[11]. EK Insko, MS Levine, BA Birnbaum, JE Jacobs, Benign and Malignant lesions of the stomach: Evaluation of CT criteria for differentiationRadiology 2003 28:166-71. [Google Scholar]