Biologic Restoration: A Treatment Option for Reconstruction of Anterior Teeth
Prashant Babaji1, Priyanka Khanna2, Shankar S3, Vishwajit Rampratap Chaurasia4, Vinaykumar S Masamatti5
1 Professor, Department of Pedodontics, Sharavathi Dental College, Shimoga, Karnataka, India.
2 Assistant Professor, Department of Conservative Dentistry & Endodontics, Qaseem Private Colleges, Ministry of Higher Education, Kingdom of Saudi Arabia.
3 Senior Lecturer ,Department of Conservative Dentistry & Endodontics, MR Ambedkar Dental College & Hospital, Banglore, Karnataka, India.
4 PG Student, Department of Conservative dentistry & Endodontics, KLE dental College, Belguam, Karnataka, India.
5 PG Student, Department of Conservative dentistry & Endodontics, KLE dental College, Belguam, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Prashant Babaji, Professor, Department of Pedodontics, Sharavathi Dental College, Shimoga, Karnataka, India. E-mail : babajipedo@rediffmail.com
Several procedures are advised to manage fractured anterior tooth structure using acrylic resin, composite restoration, ceramic or metal crown with ceramic facing. Biologic restoration is a procedure to restore fractured tooth structure with natural tooth material. In this in vitro case we have made an attempt for aesthetic rehabilitation of maxillary central incisor with similar biologic crown taken form extracted maxillary central incisor. It was observed that biologic restoration is an aesthetic, economical, fast and functional procedure which can be used as an alternative method to restore fractured primary or permanent anteriors.
Aesthetic, Anterior, Biologic restoration
Case Report
In this in vitro procedure, two identical freshly extracted maxillary central incisors with colour and dimensions, without any associated fractures or cracks were selected as experimental samples. Samples were placed in 3% aqueous buffers solution of formaldehydes. Thereafter, samples were thoroughly scaled, polished and freed from periodontal ligaments and then stored in distilled water. One sample tooth was then mounted on wax block. The crown preparation was done on mounted tooth with a chamfered cervical finish line to receive biologic crown [1]. Sharp angles were rounded and retentive undercuts were eliminated.
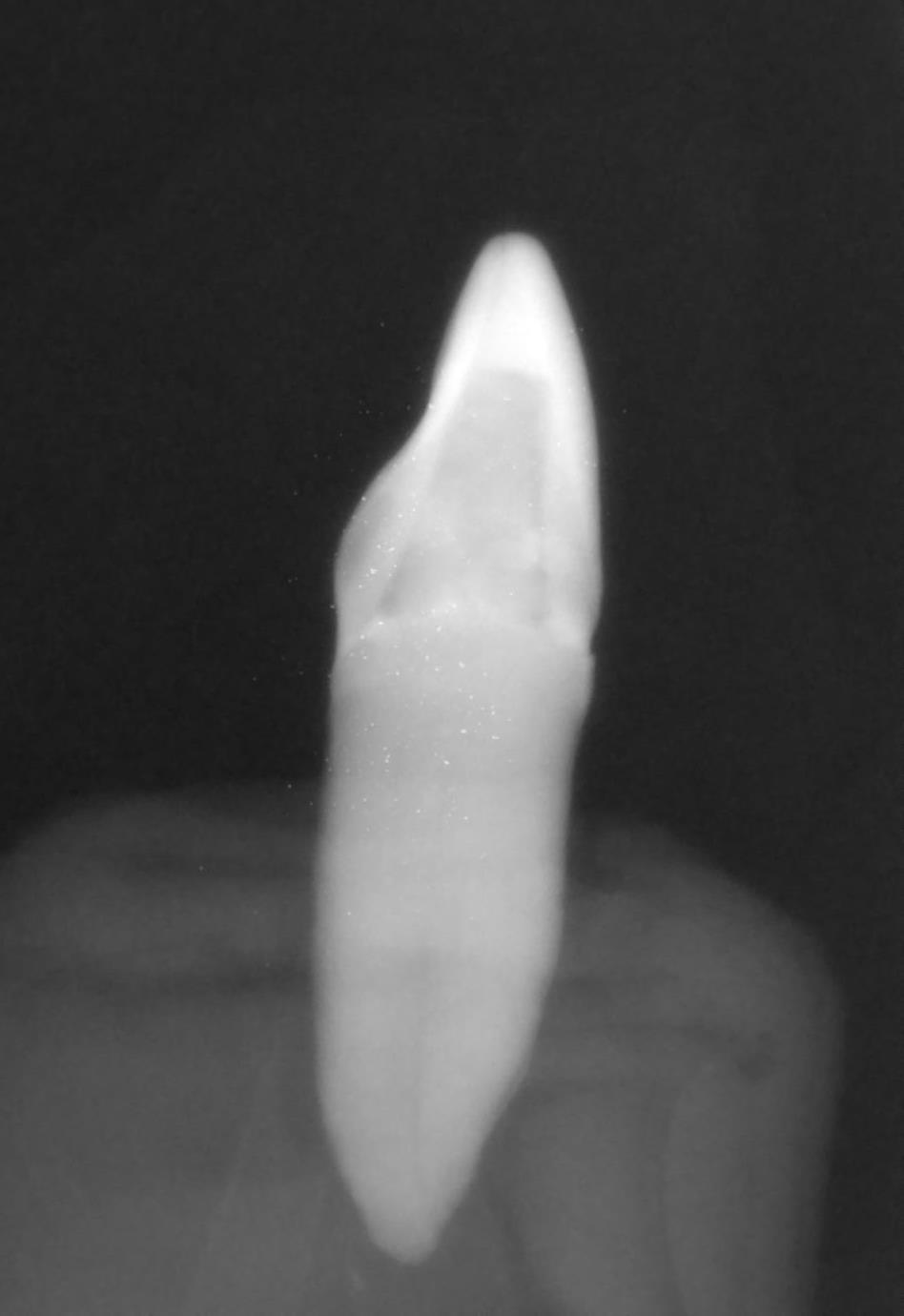
Other central incisor tooth used to make biologic crown was autoclaved at 1210C for 15 min. Then biological crown was prepared by cutting coronal portion of sterilized tooth at the level of proximal CEJ using ceramic disk and thin tapered bur [Table/Fig-1]. Pulp tissue was removed and crown portion was prepared by hallowing both internally as well as on the cervical portion of extracted sterilized crown, leaving approximately 1 mm dentine with the enamel, using various round and chamfered diamond points under cooling [Table/Fig-2a,b]. Proper fitting of prepared biologic crown was checked using articulating paper for any high points. Inner portion of crown was reduced until passive (snugly) fit occurs, which was confirmed clinically (for fitting, absence of rocking and probing around margin for marginal adaptation) and radiographically.
Crown reduction to receive biologic crown

Image showing preparation of crown from donor tooth

Image showing prepared biologic crown

The coronal portion of prepared tooth and inner portion of prepared biological crown were conditioned with 37% phosphoric acid for 15 sec and washed thoroughly followed by drying and application of adhesive system and light curing. The crown was filled with the self-curing resin cement, positioned and maintained under digital pressure until polymerization was completed. Excess extruded cement was removed. Any surface defects were corrected using flowable composite and light curing it. Finishing and polishing was done to give a final aesthetic result. Adaptation of biologic crown was finally checked clinically [Table/Fig-3a,b] and radiographically [Table/Fig-4a,b].
Labial view of biologic crown in position after cementation

Proximal view of biologic crown in position after cementation

Radiograph showing labial aspect of biologic crown after cementation
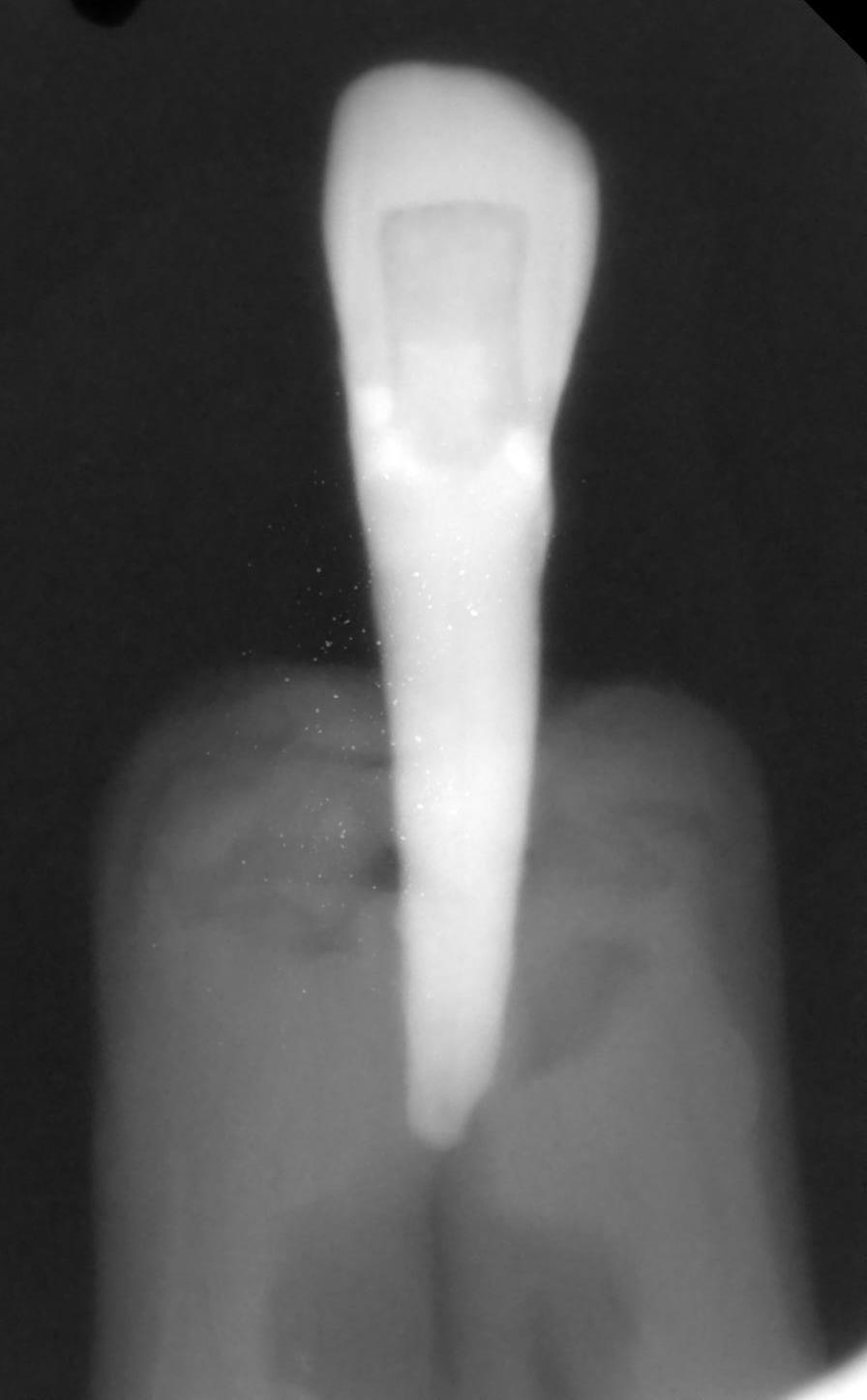
Radiograph showing proximal aspect of biologic crown after cementation
Discussion
Fractured anteriors with loss of tooth fragments results into lack of aesthetic, function and creates psychologic problems. Hence fractured teeth should be restored to improve aesthetic and self esteem of patient. Prevalence of anterior tooth fracture as a result of traumatic injuries occurs 8.1 in 1000. In the past fractured teeth were restored with acrylic resin, ceramic restorations or metal crowns. Chosack and Eildeman in 1964 published the first case report on reattachment of a fractured incisor fragment [1]. Recently with the advancement in the materials and bonding techniques has resulted into development of new method of retaining fractured natural tooth segment i,e. biologic restoration, which is gaining popularity. The term “biologic restoration” was introduced by Santos and Bianchi in 1991for restoration using sterile parts of extracted human teeth [2–4].
Various treatment modalities has been advised to manage severely damaged primary or permanent anterior teeth due to caries or fracture such as prefabricated crown, biological restoration, resin composite restoration, post and core techniques. Post and core technique is advised to build up tooth structure when there is not enough tooth structure is available either due to decay or fracture. Post and core can be done using metal, fiber or biologic post following endodontic treatment [5]. Prefabricated posts are fast; cheaper and easy to use whereas biologic posts are made from natural elements [6]. Biologic posts can resorb naturally and are cost effective [7]. Restoration of crown structure of primary or permanent anteriors can be done by various methods such as, composite build up, metal crown, ceramic crown or biologic crown. Biologic tooth can be used as post, crown or as only to restore prepared cavity [4]. To receive biologic crown or only, the prepared tooth structured should have no retentive areas, convergent walls; protect the cavity floor with calcium hydroxide for vital pulp for natural only or inlays.
Biologic restoration procedure
Biologic crowns are obtained either from donor/tooth bank or from same patient (endogenous/autogenous) [3]. Before storage of donor tooth in tooth bank it can be thoroughly cleaned and any soft tissue or periodontal remnants are removed. The pulps should be removed from root canal and kept in ultra sonic tank in 6% H2O2 for 5 cycles then stored in Hank’s balanced salt solution (HBSS) with donor identification.
Select the biologic crown for restoration by measuring the tooth to be restored using compass and selecting colour in day light. Crown adaptation can be done by direct or indirect method. For indirect method cast should be poured from maxillary or mandibular impression with irreversible hydrocolloid material. On stone cast decoronated biologic crown is tried and adjusted with high speed bur until passive fitting occurs. Occlusion can be checked and adjusted. Crown adaptation is checked clinically and radiographically. Prepared fragment is autoclaved and conditioned followed by restoration of fragment with either dual cure resin cement or luting GIC cement. Any marginal defects can be restored with flowable composite. Later the surface is finished and polished [4].
Grewal and Sethi(2008) from their comparative clinical study for period of 3,6, 9 and 12 months follow up study on biologic restoration with composite restoration found no statistical significant difference in colour matching, marginal discolouration, surface roughness, fractured restorations and clinical caries among groups [2]. In order to avoid fracture of selected donor tooth during crown preparation, it should be hydrated throughout the procedure [3]. Mandroli has observed clinically succefull results with use of natural crown and root [8]. Goenka et al., from their clinical study observed that biologic restoration is successful with use of internal beveling the fractured fragments [9]. Successful biologic restorations were also reported by various authors [2–4,7,10,11].
From the in vitro case we found that performance of biologic crown restoration was compatible with respect to shade match, marginal adaptation, discolouration, surface finish and retention.
The use of natural tooth fragments is an excellent biologic approach for restoring fractured anterior when fractured fragment is available. Biologic restoration using autogenous tooth fragments is aesthetic, cost effective, conservative procedure and faster than composite restoration [12]. Several other advantages of biologic restoration are; regaining colour, anotomy and size of the original tooth, physiologic wear similar to adjacent tooth, compatible adaptation with adjacent teeth, provides excellent surface smoothness, eliminates laboratory procedure, and has psychologic benefits [1,4–6,8,10,11].
Limitations of biologic restorations are; [
3,
10]
Need of tooth bank
Not acceptable by patients
Possibility of fracture of selected extracted tooth during its sectioning to obtain crown.
Difficulty in matching the original colour
Difficulty in obtaining teeth with the needed characteristics such as colour, anatomic size and shape and absence of cracks.
Need of sterilization of donor tooth
More time required for crown adaptation
Not much long terms studies are available regarding clinical success of biologic restoration
Conclusion
Biologic restoration is an aesthetic, alternative and economic procedure. It can be used for restoration of fractured primary or permanent anteriors. However, there is need of long term clinical studies to access its aesthetics, longevity and marginal adaptations.
[1]. Wadhwani KK, Hasija M, Meena B, Wadhwa D, Yadav R, Biologic restorations: Option of reincarnation for severely mutilated teethEuropean Journal of Dentistry 2013 2(1):62-66. [Google Scholar]
[2]. Grewal N, Sethi R, Comparative in vivo evaluation of restoring severely mutilated primary anrerior teeth with biologic post and crown preparation and reinforced composite restorationJ Indian Soc Pedod Prev Dent 2008 :141-48. [Google Scholar]
[3]. Das UK, Maiti N, Nature’s own alternative – restoration with biological crownsInternational Journal of Medical Dentistry 2013 3(2):144-49. [Google Scholar]
[4]. Sanches K, Carvalho FK, Nelson-Filho P, Assed S, Silva WGP, Queiroz AM, Biological Restorations as a Treatment Option for Primary Molars with Extensive Coronal Destruction - Report of Two CasesBraz Dent J 2007 18(3):248-52. [Google Scholar]
[5]. Verma L, Passi S, Glass fibre-reinforced composite post and core used in decayed primary anterior teeth: A case reportCase Reports in Dentistry 2011 article ID 864254, 4 pages [Google Scholar]
[6]. Bayrak S, Tunc ES, Tuloglu N, Turkey S, Plyethylene fiber-reinforced composite resin used as a short post in severly decayed primary anterior teeth: A case reportOral Surg Oral Med Oral Pathol Oral Radiol Endod 2009 107:e60-64. [Google Scholar]
[7]. Srivastav M, Singal D, Anshul Arora S, Vatsala V, Yadav V, Biologic restoration of anterior teeth: A case reportJ of Dental Science and Oral Rehabilitation 2013 :39-41. [Google Scholar]
[8]. Mandroli PS, Biologic restoration of primary anterior teeth: A case reportJ Indian Soc Ped Prev Dent 2003 21(3):95-97. [Google Scholar]
[9]. Goenka P, Marwah N, Dutta S, Biological approach for management of anterior tooth trauma: Triple case reportJ Indian Soc Pedod Prev Dent 2010 28(3):223-29. [Google Scholar]
[10]. Busato AL, Loguercio AD, Barbosa AN, Sanseverino Mdo C, Macedo RP, Baldissera RA, Biological restorations using tooth fragmentsAm J Dent 1998 11(1):46-49. [Google Scholar]
[11]. John SA, Anandaraj S, George S, Biologic restoration of a traumatized maxillary central incisor in a toddler: A case reportJ Indian Soc Pedo Prev Dent32(1):79-82. [Google Scholar]
[12]. Kulkarni VK, Bhusari CP, Sharma DS, Bhusari P, Bansal AV, Deshmukh J, Autogenous tooth fragment reattachment: A multidisciplinary management for complicated crown-root fracture with biologic width violationJ Indian Soc Ped Prev Dent 2014 32(2):190-94. [Google Scholar]