Extra- Adrenal Silent Retroperitoneal Paraganglioma: Report of a Rare Case
Hemalatha A. L.1, Avadhani Geeta K2, Anoosha K3, Ashok K.P.4, M. Rajani Deepa2
1 Professor, Department of Pathology, Affiliated to Rajiv Gandhi University of Health Sciences, Adichunchanagiri Institute of Medical Sciences, B. G. Nagar, Mandya, Karnataka, India.
2 Professor, Department of Surgery, Affiliated to Rajiv Gandhi University of Health Sciences, Adichunchanagiri Institute of Medical Sciences, B. G. Nagar, Mandya, Karnataka, India.
3 Post Graduate, Department of Pathology, Affiliated to Rajiv Gandhi University of Health Sciences, Adichunchanagiri Institute of Medical Sciences, B. G. Nagar, Mandya, Karnataka, India.
4 Post Graduate, Department of Pathology, Affiliated to Rajiv Gandhi University of Health Sciences, Adichunchanagiri Institute of Medical Sciences, B. G. Nagar, Mandya, Karnataka, India.
5 Post Graduate, Department of Pathology, Affiliated to Rajiv Gandhi University of Health Sciences, Adichunchanagiri Institute of Medical Sciences, B. G. Nagar, Mandya, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Hemalatha. A.L No: 156, 12th cross, 2nd main, Jayanagar, Mysore- 570014, India. Phone : 8453399335, E-mail : halingappa@gmail.com
Extra- adrenal retroperitoneal paragangliomas are extremely rare neuroendocrine neoplasms with an incidence of 2-8 per million. They arise from embryonic neural crest cells and are composed mainly of chromaffin cells located in the para- aortic sympathetic chain. They synthesize, store and secrete catecholamines because of which they may present with headache, sweating, palpitation and symptoms of hypertension. On the other hand, they may remain silent and non- functional and present with vague symptoms like pain abdomen due to episodic release of catecholamines.
Histologically and immunohistochemically, non- functional and the functional tumours are no different from each other. Primary methods of pre-operative diagnosis include imaging techniques which also help in surgical planning and pre-operative preparation. Non- functional tumours of ten escape pre-operative detection and create per- operative complications. We present a case of non- functional extra- adrenal retroperitoneal paraganglioma occurring in a 66-year-old female patient presenting with pain and mass per abdomen.
On ultrasonongraphy, a retroperitoneal mass of probable mesenchymal origin was suspected. The patient was posted for surgical resection of the mass. Per-operatively, the patient developed hypertensive crisis and massive bleeding. Post-operatively she developed renal failure and succumbed to it after three days. This report highlights the importance of pre- operative diagnosis which is vital in the management of extra- adrenal retroperitoneal paraganglioma.
Adrenal pheochromocytoma, Neuroendocrine, Retroperitoneal
Case Report
A 66-year-old female patient presented to surgical department with complaints of pain abdomen and myalgia in the left hypochondrium. There was no history of vomiting or altered bowel habits or previous history of similar attacks. The patient was not a known hypertensive and was not on any medication.
Per abdominal examination revealed tenderness and a mass in the left hypochondriac region which did not move with respiration. Bowel sounds and rectal examination were normal. Ultrasonography showed a retroperitoneal mass suspected to be of mesenchymal origin probably arising from the nerve sheath. The hematological and biochemical profiles were normal. Laparotomy was undertaken for exploration by left paramedian incision. Per-operatively, a retroperitoneal mass was found inferior to the renal vein on the left side of aorta occupying 2nd, 3rd and 4th lumbar vertebral levels. The tumour was abutting the aorta encircling about 2/3rds of the aortic circumference. The ureter was pushed anteriorly while the inferior mesenteric vessels were pushed laterally. Many direct arterial connections were seen supplying the mass from the aorta. The mass was found located anterior to the sympathetic and lymphatic chain. While attempting to separate the mass, the short veins draining to the renal vein were avulsed. Further dissection revealed that the mass was arising from the sympathetic chain. The mass was completely resected.
Histopathological Findings
Gross examination: Single, soft well- encapsulated reddish mass measuring 7 x 6 x 5 cms. The cut section was solid, homogeneous, grey- brown to grey- yellow with a few tiny cystic spaces [Table/Fig-1].
Cut section of the mass which is solid, homogeneous, grey- brown to grey- yellow with a few tiny cystic spaces,

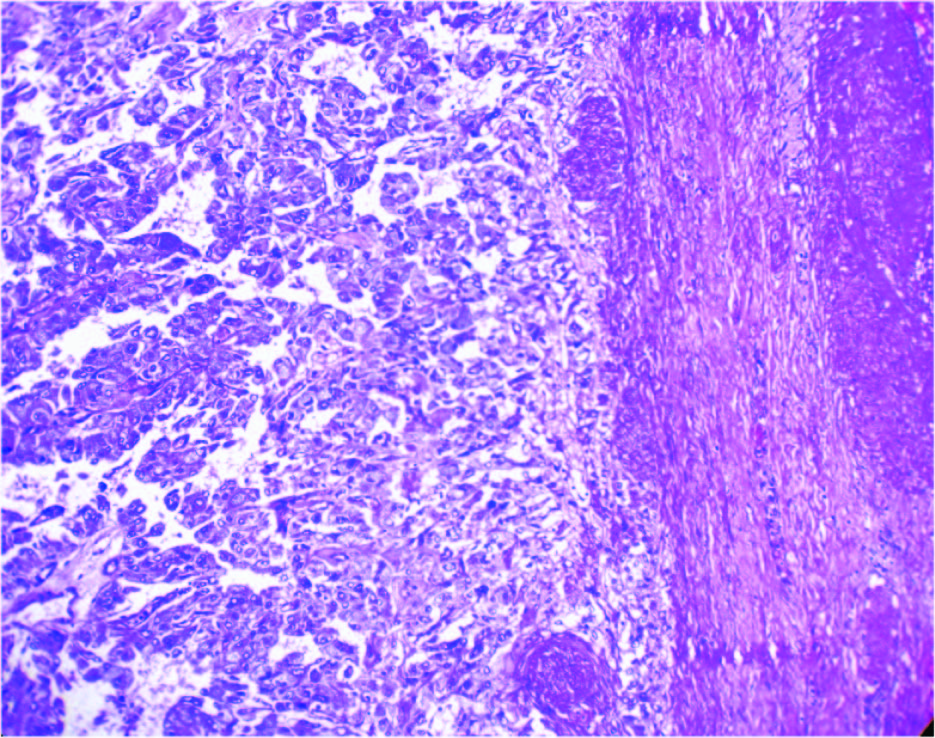
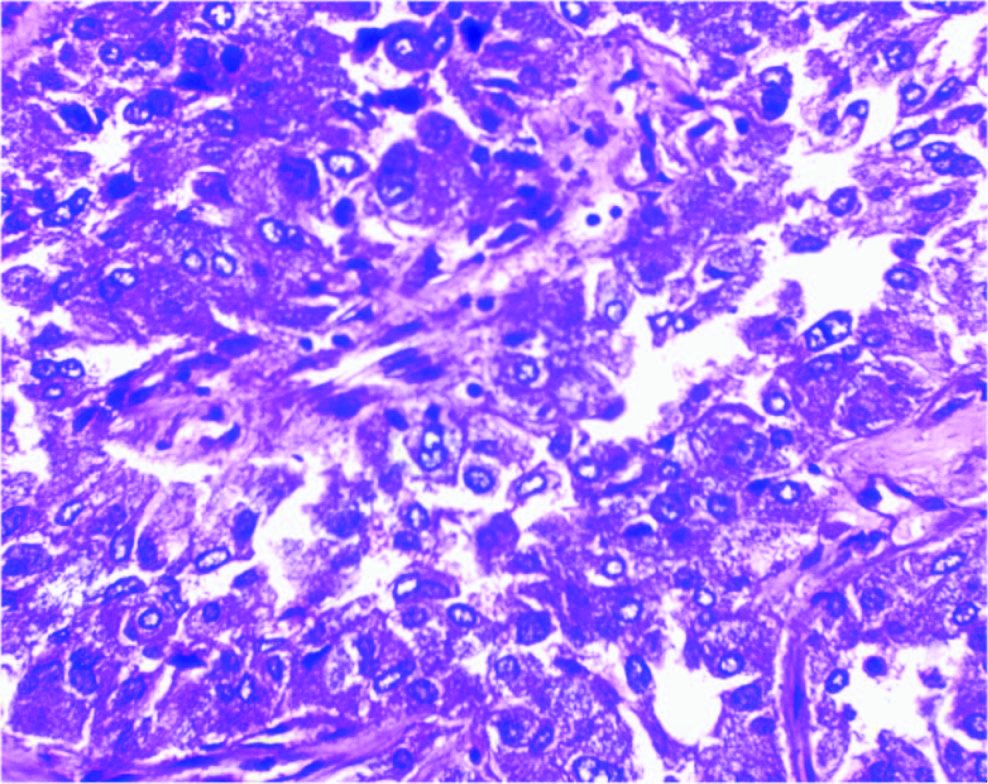
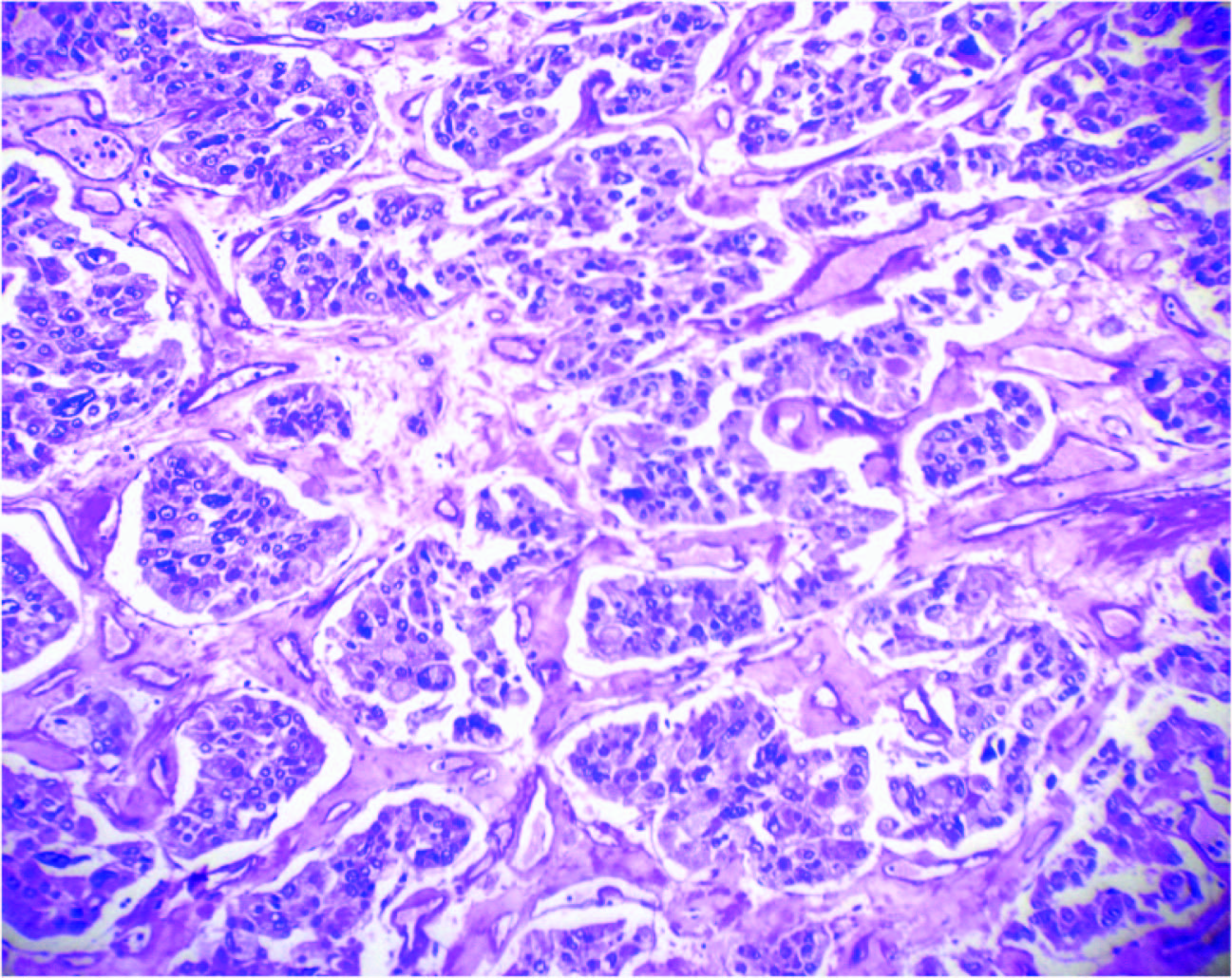
Microscopy:Showed a well- encapsulated tumour [Table/Fig-2] composed of large round to polyhedral cells arranged in cords, trabecular patterns and nests (Zellballen) [Table/Fig-3] with abundant acidophilic cytoplasm and nuclei with salt and pepper type of chromatin [Table/Fig-4].
Cellular tumour with thickened capsule, (H & E, ×100)
Large tumour cells with abundant granular cytoplasm and nuclei with salt pepper type chromatin, (H & E, ×400)
Tumour cells in Zellbalen pattern, (H & E, ×400)
Histopathological diagnosis: Extra- adrenal retroperitoneal paraganglioma.
Immunohistochemistry showed positivity for Chromogranin and S- 100 protein.
Discussion
Paragangliomas are rare neuroendocrine tumours arising from specialized cells referred to as chief cells of paraganglia which are spread over the entire body ranging from the skull to the pelvic floor. Regardless of their location, these are referred to as “paragangliomas”. The only exception to this rule being the paraganglioma arising from the adrenal medulla commonly referred to as “pheochromocytoma”. The term “extra- adrenal paraganglioma” is applicable to paragangliomas situated outside adrenal medulla. Majority of the paragangliomas are known to occur in specific locations like the carotid body, jugular foramen, middle ear, aortico- pulmonary region, posterior mediastinum and abdominal para aortic region including the Zuckerkandl’s body or aortic body [1,2]. The adrenal medulla has the largest collection of receptor cells derived from the neural crest which accounts for the highest rate of occurrence of these tumours in this site. Whereas, extra- adrenal retroperitoneal paragangliomas arise from the symmetrically distributed paraganglia situated in close relation to the aorta and sympathetic chain. These paraganglia which are histologically similar to carotid body and adrenal medullary paraganglia regress after the age of 1 to 1 ½ years [3].
Some of the paragangliomas are known to originate, store and secrete catecholamines and are hence termed “functional paragangliomas”. While these are easily diagnosed, non- functional paragangliomas may create considerable difficulties in pre-operative diagnosis.
Extra- adrenal paragangliomas are rarely encountered in surgical practice. If they are non- functional, they can pose additional diagnostic dilemmas thus causing difficulties in the choice of treatment and management options as in the present case.
Extra- adrenal retroperitoneal paragangliomas exhibit classic histological features which help clinch the diagnosis. But, the true essence of appropriate management lies in the pre-operative diagnosis since pre-operative pharmacological preparation with alpha- adrenergic blockade for 2- 4 weeks to prevent and treat a syndrome of possible intra- operative catecholamine release may be initiated failing which, catecholamine induced complications like hypertensive crisis, cardiac arrhythmias, pulmonary edema and cardiac ischemia due to manipulation of the tumour may ensue. Even a hypotensive crisis may arise after tumour removal. Pre-operative diagnostic modalities include radio- imaging techniques including USG, CT, MRI, I 131, MIBG and octreotide along with endocrine secretion evaluations [3]. These pre-operative diagnostic modalities were unaffordable to our patient. Hence, the tumour was diagnosed post-operatively based on its classic histologic features.
A multitude of factors contribute to the difficulties encountered in the management of extra- adrenal paragangliomas as in our case. They include the rarity of extra- adrenal paragangliomas which account for just 2-8 per million incidence, the paucity of information available regarding their natural history and outcome and the non- availability of a definitive pre- operative diagnosis especially in a non- functional tumour [3].
Extra- adrenal paragangliomas can be uni or multicentric with a tendency for local invasion and therefore,a thorough evaluation needs to be undertaken to rule out multicentricity. Periodic follow- ups will have to be scheduled to rule out recurrence. 24- 50 % of extra- adrenal paragangliomas are malignant in contrast to malignant pheochromocytomas which have an incidence of 10% [3].The tumour in the present case was benign, unicentric and lacked local invasion.
Wendelin et al., observed that benign and malignant lesions could not be distinguished based on histopathological findings alone. They opined that distant metastases and local invasion of adjacent organs were the only reliable indicators of malignancy [4]. The tumour in the present case was interpreted as benign based on the histopathological findings and absence of local invasion.
Sclafani et al., concluded that patients in whom a complete surgical dissection was possible had a better overall survival than patients in whom it was not [5]. Though a complete surgical resection was possible in the present case, the patient succumbed to the complications of hypertensive crisis.
Malignant extra- adrenal paragangliomas are known to metastasize to bone, liver, peritoneum, pelvis, ovaries, cervical lymph nodes and lung [5]. No evidence of distant metastases was detected in the present case.
The pre-operative differential diagnosis considered in the present case were retroperitoneal malignant mesenchymal tumour and mixed germ cell tumour.
Conclusion
Extra- adrenal retroperitoneal paragangliomas are rare neoplasms which may cause difficulty in diagnosis and treatment. Yet, a pre-operative diagnosis is imperative for pre-operative preparation and proper planning of management.Therefore, we wish to highlight the importance of pre- operative diagnosis in these tumours due to our own bad experience of a non- functional tumour which escaped a definitive pre- operative diagnosis resulting in unforeseen development of per operative hypertensive crisis leading onto massive bleeding, shock, renal failure and finally a fatal outcome.
[1]. Feng N, Zhang WY, Wu XT, Clinicopathological analysis of paraganglioma with literature reviewWorld J Gastroenterol 2009 15:3003-08. [Google Scholar]
[2]. Bismar HA, Murshid KR, Extra adrenal retroperitoneal paragangliomaSaudi Med J 2003 24:778-80. [Google Scholar]
[3]. Wen J, Li HZ, Ji ZG, Mao QZ, Shi BB, A decade of clinical experience with extra- adrenal paragangliomas of retroperitoneum: Report of 67 cases and a literature reviewUrol Ann 2010 2:12-16. [Google Scholar]
[4]. Hayes WS, Davidson AJ, Grimley PM, Hartman DS, Extra- adrenal retroperitoneal paraganglioma: clinical, pathologic and CT findingsAm J Rad 1990 155:1247-50. [Google Scholar]
[5]. Sclafani LM, Woodruff JM, Murray FB, Extraadrenal retroperitoneal paragangliomas- from the departments of Surgery and Pathology, Memorial Sloan- Kettering Cancer center, New YorkSurgery 1990 108:1124-30. [Google Scholar]