Background: Examination of bone marrow plays a pivotal role in the practice of haematology. It can be evaluated by three ways–bone marrow aspiration (BMA), bone marrow touch imprints (BMI) and bone marrow biopsy (BMBx).
Aim and Objective: To study the efficacy and reliability of BMI smears in comparison to BMA smears, in making a diagnosis of diseases involving bone marrow.
Setting and Designs: This study was carried out in the Department of Pathology, Institute of Medical Sciences, Varanasi over a period of 26 months.
Materials and Methods: A total number of 182 cases, with their BMA, BMI and BMBx samples (from each and every case), were evaluated and their findings even compared.
Statistical Analysis: All the observations were evaluated using simple and basic statistical tool, i.e. percentage.
Results: The cellularity or cell density on BMI correlated with the cellularity of BMBx in 78.6% cases, which was higher than the value observed with BMA smears (71.4%). The spreading quality was better and cytological details were better appreciated in BMI as compared to BMA. Also, the presence of lymphoglandular bodies and particles on BMI were additive diagnostic clues. All of those findings were reflected in the higher diagnostic accuracy of BMI than BMA.
Conclusion: BMI should be a standard practice and be considered as an early and reliable diagnostic tool for evaluating bone marrow pathologies
Introduction
The role of evaluation of bone marrow cannot be underestimated in the practice of Medicine. It serves as a very useful diagnostic tool in many haematological disorders originating and/or infiltrating the marrow, as well as many non-haematological disorders documented to have bone marrow involvement. Bone marrow can be evaluated by three ways – Bone marrow aspirate (BMA) smears, Imprints or touch preparations(BMI) of bone marrow core biopsies, and histological sections of core biopsies (BMBx). Evaluation of BMA and BMI smears requires much less time compared to BMBx, as the latter has to undergo various time-consuming processes including fixation, decalcification, dehydration, block-preparation and soon. There is a wide range of medical conditions where evaluation of mere BMA smears alone does not turn out to be fruitful, because of dry tap, bloody tap, poor spreading etc. In such situations, evaluation of BMI smears may be very useful in diagnosing the underlying disease process. Therefore, it may help in initiating a prompt treatment in critically ill patients without waiting for the histopathological report of core biopsy.
Materials and Methods
Samples of bone marrow aspiration, imprints and biopsy were collected from medical department and paediatric department of Sir Sunderlal Hospital, Banaras Hindu University, Varanasi, India. The period of sampling was from August 2011 to October 2013.
The standard technique [1] was employed for obtaining the aspirate samples using Salah’s needle from posterior superior iliac spine. The trephine biopsy [2] was performed using the Jamshidi’s needle with the length of the biopsy core between 2.5-3.5 cm. Touch imprint smears were prepared by using the procedure of gentle touch and rolling of biopsy core on the slide. The biopsy core was then fixed, decalcified and finally 2-3 thin sections were made.
All the patients were checked for having any major coagulation disorder before undergoing any procedure.
The slides of BMA and BMI smears were stained with Leishman and Wright-Giemsa methods, while the BMBx slides were stained by hematoxylin-eosin and reticulin methods.
Evaluation of slides
The following parameters were documented in both BMA and BMI smears:
1. Cellularity or cell density
2. Spreading quality of smears
3. Quality of cytomorphological details of the cells
The cellularity of BMA smears were assessed in the particles and their trails considering the proportion of hematopoietic cells and adipocytes in the particles and subjectively estimated as the percentage of area of the particles occupied by the hematopoietic cellular elements. The normal cellularity varies with age, and evaluation of cellularity must always be made in the context of the patient’s age [3], i.e. newborn (80-100%), child < 10 y (60-95%), adult (25-75%) and ≥ 70 y (10-50%).
Considering the age-related cellularity of BMA particles, the smears were labelled as normocellular if the cellularity falls in the normal range and as hypocellular and hypercellular if the cellularity crosses the lower and upper limits of cellularity respectively.
As the cellularity of BMI smears has not been described in details in any previous study, we proposed a grading system to assess the cellularity or cell density of the touch preparations as shown in [Table/Fig-1].
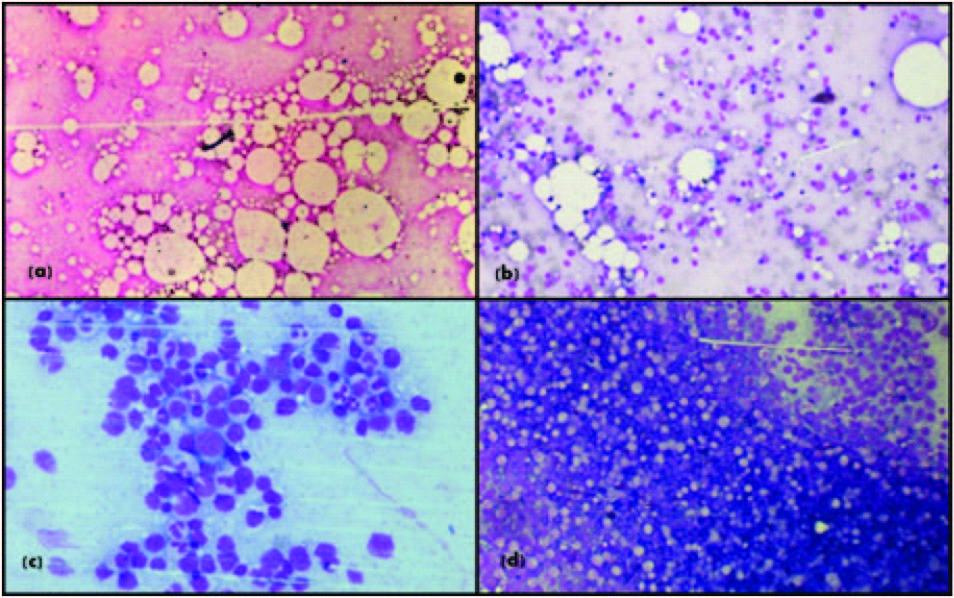
For example a “Grade 3” is termed as “good” cell density and corresponds to a “hypercellular” BMI smears [Table/Fig-2].
Spreading quality of both BMA and BMI smears are again graded as shown in [Table/Fig-3].
Quality of cytomorphological details is graded depending on ease of appreciability of cellular details as shown in [Table/Fig-4].
Results
A total number of 182 cases, both from neoplastic and non-neoplastic diseases, were studied with their BMA, BMI and BMBx, in each and every case.
Out of the 46 cases, where repeated attempts of BMA were met with dry tap, in only 18 cases BMI were acellular. In the rest 28 cases (60.8%), BMI were informative, yielding 11 hypocellular touch imprint smears from aplastic anaemia, 3 normocellular (two from aplastic anaemia and one from metastatic adenocarcinoma) smears and 14 hypercellular (including 7 acute leukaemias, 3 multiple myelomas, 2 myelodysplastic syndromes and 2 chronic myeloid leukaemias) smears
Out of 37 hypocellular BMA, there was concordance with BMI in 94.6% (n=35) cases, while among 75 hypercellular BMA smears, only 53 (70.6%) showed hypercellular BMI. In total, there was concordance in the cellularity of BMA and BMI smears in 130 cases (71.4%).
Bone marrow of core biopsy sections were considered as the gold standard for assessment of marrow cellularity [2], and the cellularity of BMA and BMI were compared with the cellularity of corresponding biopsy sections.
Among the hypercellular BMBx (n=84) sections, 79.8% (n=67) BMI were hypercellular, and the rests were normocellular, probably due to better distribution of cells. In cases of hypocellularity (n=58), the findings of BMI and BMBx were comparable in 75.9% cases. In total, the cellularity of BMI and BMBx were in concordance in 78.5%(n=143) cases. This value is much higher than the concordance of cellularity of BMA smears and BMBx sections (71.4%).
Spreading quality was “good” (grade III) in 63 BMI smears as compared to 52 BMA smears. Also the number of “fair” (grade II) quality spread smears were higher in BMI (n=63) than BMA (n=53). In total, 21(11.5%) more numbers of BMI smears were spread better than BMA smears.
In 102 BMI smears and 89 BMA smears, the cytomorphological details of individual cellular elements were excellent. There was very little difference in the number of BMI (n=70) and BMA (n=67) smears displaying appreciable cytological details. The occurrence of poor quality BMI smears (n=13) was lower as compared to BMA (n=23) smears.
The diagnostic accuracy of BMA and BMI were comparable in cases of nutritional deficiency anemias, CML, lymphomas, TB, CLL and metastatic adenocarcinoma. Both the procedures were non-diagnostic for all the cases of myelofibrosis and polycythemia vera-spent phase. In cases like aplastic anaemia, acute leukemia, multiple myeloma and myelodysplastic syndromes, BMI were more helpful than BMA in making diagnoses. On the whole, the diagnostic accuracy of BMI for bone marrow pathologies was significantly higher than BMA [Table/Fig-5].
Discussion
WHO has focused on the utility of BMBx as an essential aid in the diagnostic and prognostic evaluation of haematological diseases, while little work has been done on BMI. Only a few studies, over past decade, have tried to study BMI in details.
In our study, we evaluated the importance of BMI smears as a reliable diagnostic tool, especially in cases where BMA smears turned out to be non-diagnostic or uninformative.
There was concordance in the cellularity of BMI with cellularity of BMA smears in 61.5% cases, which was quite comparable with the observation of study by X Gong et al., [4] [Table/Fig-6].
The occurrence of dry tap in 22 marrows from aplastic anaemias and bone marrow from hypocellular MDS was a major cause of discordance of BMA and BMI cellularity. Dry tap was also encountered in two CML and 7 acute leukaemia cases, probably due to packed marrow. Four cases of multiple myeloma, on aspiration, yielded only blood. Inability to aspirate marrow elements resulting from clot formation at the site of needle-puncture in hypercoagulable state of myeloma might be the cause of blood tap. In majority of above mentioned cases, BMI smears were more helpful, as they were prepared by gentle touch and rolling of core biopsy over glass-slides so that impression of the cells were made by almost all aspects of the core biopsy. This procedure will enhance the detection of focal involvement of marrow also.
Considering BMBx as the gold standard for assessment of bone marrow cellularity, 78.5% BMI smears had cellularity comparable with that of BMBx. The value was much higher as compared to the concordance of BMBx and BMA cellularity (71.4%).
The spreading quality of BMI was found to be better than BMA. Simple exfoliation of loose cells from the surface of core biopsies, while preparing smears might be the reason for better spreading of BMI, while spreading of BMA was dependant on multiple factors, like delay in spreading and uneven edge of the spreader.
Even the cytological details of individual cellular element were better appreciable in BMI smears than BMA. Mutilation of the cells with aspiration and spreading of BMA smears may be the cause, while BMI were prepared be gentle rolling
Asessment of cellularity on BMA is undertaken by assessing the percentage of the particles occupied by haematopoietic cells, whereas, assessment of cellularity on BMI is based primarily on cell density. Presence of marrow particles on BMI further enhances the diagnostic accuracy of assessing cellularity as BMI. In addition, assessment of marrow iron stores becomes feasible.
The previous studies have documented diagnostic accuracy of BMI between 83.7% and 99.4%[7,8]. Our observation was well within this range (87.3%). We observed a higher diagnostic accuracy of BMI in comparison to BMA. This finding is supported by all the previous studies [Table/Fig-7].
Assessment of cell density on bone marrow touch imprint smears
| Grade | Cell Density | Cellularity | Description |
|---|
| 3 | Good | Hypercellular | • Marked clumping and overlapping of cells |
| • No definite morphology can be identified in the clump |
| • Need to go at the periphery of the smears to comment on morphology |
| 2 | Fair | Normocellular | • Few small clumps to none |
| • Well distributed cells |
| • Morphology can be easily identified in any area |
| 1 | Poor | Hypocellular | • Occasional clumps to few cells(3-5) to no clump |
| • Cells wide apart, need to examine many fields to count 100 cells |
| 0 | Acellular | Acellular | • No hematopoietic cell in any field, and/or |
| • Marked adipocytosis, and/or only blood |
Grading of cellularity of bone marrow imprint smears (a) Acellular, (b) Poor cellularity (Grade I), (c) Fair cellularity (Grade II) and (d) Good cellularity (Grade III)
Assessment of spreading quality of bone marrow aspiarte and imprint smears
| Spreading Quality | Description |
|---|
| Good (Grade III) | Richly cellular smear with no verlapping, cell identification and differentiation is easy |
| Fair Grade II) | Fair cellularity with no or minimal overlapping, cellular differentiating features appreciable |
| Poor(Grade I) | Sparsely cellular smear with difficulty in counting of cells, or, Heavily cellular smear with frequent overlapping of cells obscuring their cytological details, regardless of their staining quality |
Assessment of cytomorphological details of bone marrow aspirate and imprint smears
| Cytomorphological Details | Description |
|---|
| Good(Grade III) | Good stainining making finer nuclear and cytoplasmic details clear |
| Fair(Grade II) | Cell identification and differentiation possible, but finer nuclear and cytoplasmic details are difficult to appreciate |
| Poor(Grade I) | Cell identification is very difficult due to overstainining, or, understainining and/or presence of artefacts or stain deposits |
Diagnostic accuracy of aspiration and imprint smears
| Diagnosis(Numbers of cases) | Diagnostic Accuracy |
|---|
| Aspiration Smears | Imprint Smears |
|---|
| Aplastic anemia(57) | 35(61.4%) | 46(80.7%) |
| Nutritional deficiency anaemia(36) | 36(100%) | 36(100%) |
| Acute leukemia(34) | 30(88.2%) | 34(100%) |
| Chronic Myeloid Leukemia(15) | 15(100%) | 15(100%) |
| Multiple myeloma(12) | 7(58.3%) | 11(91.6%) |
| Myelodysplastic syndromes(10) | 7(70%) | 9(90%) |
| Myelofibrosis(7) | 0(0%) | 0(0%) |
| Lymphoma(4) | 4(100%) | 4(100%) |
| Tuberculosis(3) | 1(33.3%) | 1(33.3%) |
| Metastatic adenocarcinoma(2) | 2(100%) | 2(100%) |
| Polycythemia vera – spent phase(1) | 0(0%) | 0(0%) |
| Chronic lymphocytic leukemia(1) | 1(100%) | 1(100%) |
| TOTAL(n=182) | 138(75.8%) | 159(87.3%) |
Concordance in cellularity between aspirate and imprint smears among different studies.
| Study | Numbers Of Cases Studied | Concordance |
|---|
| X. Gong et al., [4] | 3781 | 2369(62.6%) |
| D. Pasquale et al., [5] | 20 | 18 (90%) |
| Present study | 182 | 112(61.5%) |
Diagnostic accuracy of aspiration and imprint smears
| Study | Numbers of Cases | Diagnostic Accuracy |
|---|
| Aspiration Smears | Imprint Smears |
|---|
| X.Gong et al., [4] | 1025 | 921 (89.8%) | 969(94.5%) |
| N. Verma et al., [6] | 535 | 342 (63.9%) | 479 (89.5%) |
| D. Pasquale et al., [5] | 108 | 95 (87.9%) | 101 (93.5%) |
| S. Chandra et al., [7] | 565 | 438(77.5%) | 473(83.7%) |
| R. Aboul- Nasr et al., [8] | 173 | 146(84.4%) | 172(99.4%) |
| Present study | 182 | 138(75.8%) | 159(87.3%) |
Conclusion
The study concludes that BMI are unquestionably important for investigation of bone marrow pathologies. It provides better information regarding marrow cellularity in comparison to BMA. Differential count is easier on BMI due to better spreading of cells. Owing to less mutilation, cellular cytological details are better appreciated in BMI. Even it provides some important diagnostic clues (e.g. marked adipocytosis). All these are ultimately reflected in better diagnostic accuracy of BMI as compared to BMA. It also avoidsthe unnecessary delay caused by decalcification and processing of BMBx sections in routine histopathology laboratories.
BMI should, therefore, be standard practice and be considered as an early and reliable diagnostic tool for evaluating any marrow pathology.
[1]. BJ Bain, Bone marrow aspirationJ Clin Pathol 2001 54:657-63. [Google Scholar]
[2]. BJ Bain, Bone marrow trephine biopsyJ Clin Pathol 2001 54:737-42. [Google Scholar]
[3]. RJ Hartstock, EB Smith, CS Petty, Normal variations with ageing of the amount of hematopoietic tissue in bone marrow from anterior iliac crestAmerican Journal of Clinical Pathology 1965 43:326-31. [Google Scholar]
[4]. X Gong, X Lu, X Wu, Role of bone marrow imprints in hematological diagnosis: A detailed study of 3781 casesCytopathology 2012 23:86-95. [Google Scholar]
[5]. D Pasquale, G Chikkappa, Comparative evaluation of bone marrow aspirate particle smears, biopsy imprints and biopsy sectionsAm J Hematol 1986 22:381-89. [Google Scholar]
[6]. N Verma, S Dash, R Sarode, N Marwaha, Relative efficacy of bone marrow trephine biopsy sections as compared to trephine imprints and aspiration smears in routine hematological practiceIndian J Pathol Microbiol 1993 36:215-26. [Google Scholar]
[7]. S Chandra, H Chandra, Comparison of bone marrow aspirate cytology, touch imprint cytology and trephine biopsy for bone marrow evaluationHematology Reports 2011 3:22 [Google Scholar]
[8]. R Aboul-Nasr, EH Estey, HM Kantarjan, Comparison of touch imprints with aspirate smears for evaluating bone marrow specimensAm J Clin Pathol 1999 111:753-58. [Google Scholar]