Kabuki make-up syndrome (KMS), also called Niikawa-Kuroki syndrome reported in 1981, is a rare congenital disorder of unknown aetiology. It is know to occur in many other ethnic groups, though initially described in Japan. We report a 24-year-old girl of Asian origin diagnosed with Kabuki syndrome based on characteristic clinical features. It is characterized by distinctive facial features (eversion of the lower lateral eyelid, arched eyebrows with the lateral one-third dispersed or sparse, depressed nasal tip, and prominent ears), skeletal anomalies, Dermatoglyphic abnormalities, short stature. As per our knowledge there is no literature which gives information about the importance of electromyographic study in the diagnosis and treatment of the KMS. Hence, this report emphasizes on the role of the same.
Case Report
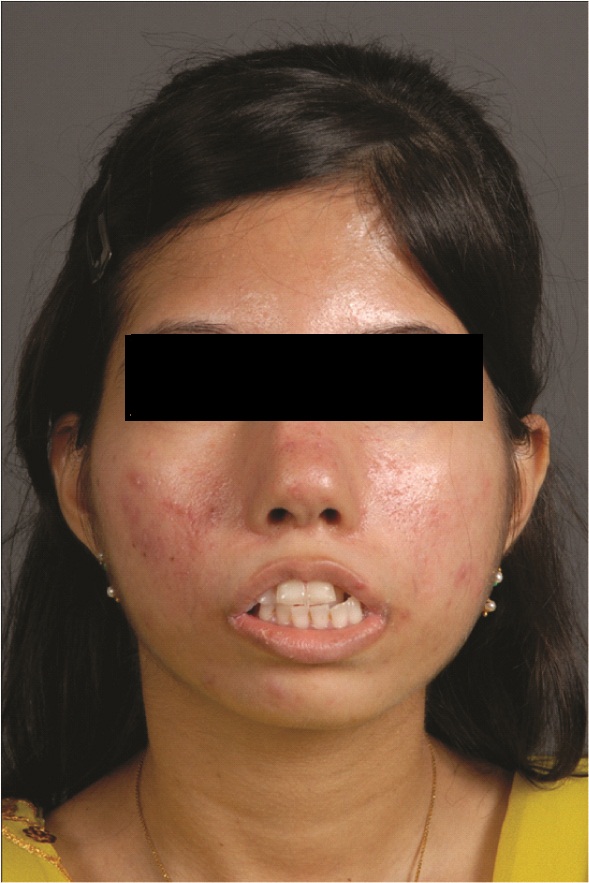
A 24-year-old female patient reported to the Department of Oral Medicine with a compliant of incomplete closure of the lips, difficulty in speech and forwardly placed teeth since birth. She is the first child born after 36 wk of gestation to a healthy mother and no history of consanguineous marriage in the family. She had history of recurrent infections in childhood, feeding difficulties, post natal growth retardation with no mental retardation. Patient exhibited many clinical features [Table/Fig-1,2,3] as summarised in [Table/Fig-4].
Patient was moderately built and nourished with short stature, neurological examination revealed weakness of small muscle of hand, grade IV power in right upper limb, paresis of III, IV and VI nerves causing external ophthalmoplegia. It was noted that patient had articulation errors and abnormal oral resonance, which appeared to be due to poor oral-motor coordination and hypotonia.
Intra oral examination revealed short upper lip (bow shaped), incompetent lips, shallow sulcus depth, bimaxillary protrusion, end on molar relation, cross-bite (lower left anterior), high arched palate and speech abnormality. A distinct feature of wasting of muscle of tongue on right side [Table/Fig-5] was observed which has not been reported previously in the literature of KMS. Routine dental and skeletal radiographs were unremarkable.
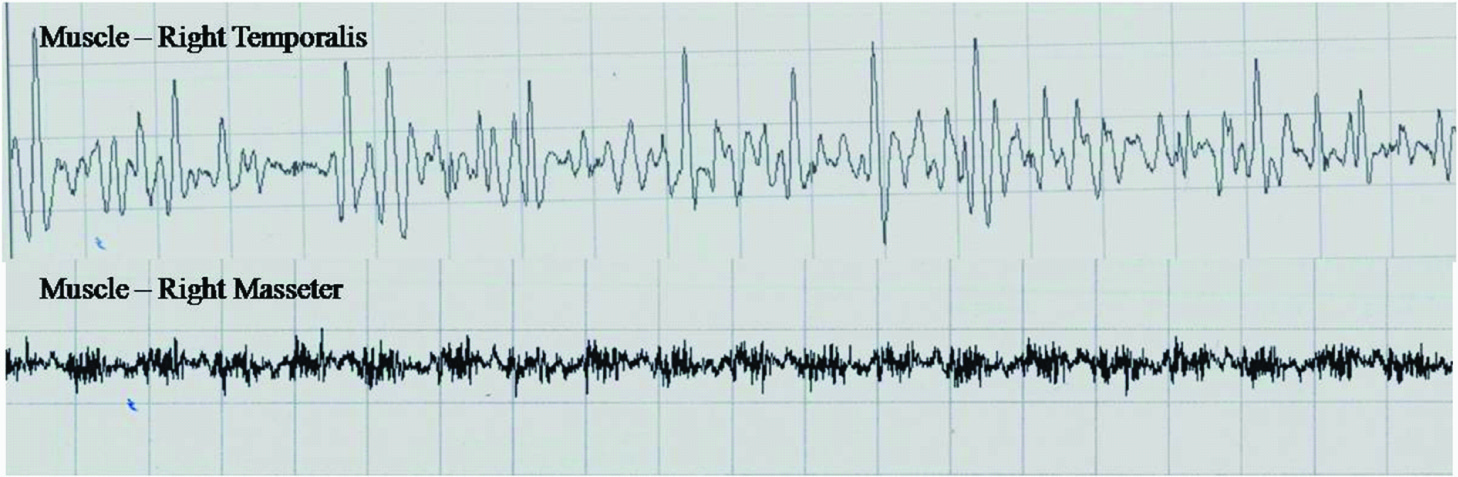
Further, the patient was subjected for the electromyographic study of the facial muscles and the muscles of mastication. Needling of the masseter, orbicularis oculi, frontalis, buccinator, orbicularis oris, temporalis and zygomaticus muscles was done. No resting muscular activity was observed in any of muscles studied. No activity was observed in frontalis, orbicularis oris, orbicularis oculi, and buccinator [Table/Fig-6] however, activity in Temporalis and masseter [Table/Fig-7] was observed. The compound muscle action potentials (CAMPs) from right facial nerve showed reduced amplitude as compared to left [Table/Fig-8] . Patient is undergoing physiotherapy for the hypotonia and is referred to speech therapist.
Discussion
Kabuki Make-Up Syndrome (KMS) was first described in Japanese children by Kuroki et al and Niikawa et al., in 1981[1,2]. Because the facial features of the patients resembled the make-up of actors in Kabuki, the traditional Japanese play, hence the term ‘Kabuki make-up syndrome’. KMS is a rare syndrome and the diagnosis of KMS is based on a series of clinical arguments including five major criteria proposed by Niikawa and Kuroki [2-5]. It is estimated that KMS occurs in about one in 32,000 births [7]. Failure to thrive with confirmed growth hormone deficiency (GHD) in KMS is also noted [6]. The clinical features as tabulated in [Table/Fig-4] . In the present case most of these manifestations were noted and the diagnosis was established based on these clinical findings.
Dental abnormalities have been reported in over 60% of patients with KMS and include most commonly hypodontia (particularly of central/lateral incisors and premolars) associated with interdental spacing and microdontia. KMS patients have a tendency of mid-face hypoplasia possibly predisposing them to the development of a small dental arch and malocclusion (associated arch discrepancy). Abnormal tooth morphology has been seen in this syndrome with teeth being conically-shaped and the upper incisors as ‘flat head’ screwdriver-shaped, which may aid diagnosis [7].
KMS may be an under-diagnosed condition in the cleft lip and palate population. Approximately one-third of KMS patients have cleft lip/palate, and a high arched palate has been seen in almost two-thirds of patients. KMS patients may also exhibit ptosis, an expressionless face and a drooping lower lip [7]. Petzold et al., [5] described dental radiographic features of enlarged pulp cavities of molars with pulp stones, widened pulp chambers of incisors, external root resorption of incisors, incomplete root formation and root division of a normally single-rooted tooth. These radiographic features together with the clinical features assist in diagnosing the condition.
Neurological and endocrinological anomalies that are reported include neonatal hypotonia, feeding problems, seizures, microcephaly, brain atrophy, growth hormone deficiency, precocious puberty, hypoglycemia, delayed sexual development, and diabetes insipidus. Hypoglycemia, is an uncommon feature in KMS and it is very important to be recognized, as early diagnosis and appropriate management will reduce further long-term neurologic morbidity in these patients [8]. Although diagnosis relies on dysmorphic features, neurological symptoms are the most invalidating manifestations in the Kabuki syndrome clinical spectrum, often presenting as the first complaint; nevertheless, Kabuki syndrome is still a rare diagnoses at neurology clinics [2,9]. The condition affects males and females equally and it’s more common in Japanese population however, it is now known to occur in many other ethnic groups [2]. Schrander-Stumpel et al., reported 29 Caucasian patients and reviewed 60 Japanese and 29 non-Japanese patients, noting that non- Japanese patients with this syndrome had more marked neurological symptoms. In over 80% of non-Japanese patients, neurological symptoms were a major clinical problem [10] . The identification of MLL2 gene mutation in 2010 has got a very important role in the diagnosis of KMS patients in recent years. In a study by Yuan S[11] the genetic analysis of KMS was conducted towards pertinent gene mutations. The screening of 110 families with KMS showed MLL2 mutations in 81/110 (74%) of families. KMS may have novel nonsense or frame shift mutations predictive of haploinsufficiency. The clinical characteristics of MLL2 mutation-positive cases did not differ significantly from MLL2 mutation-negative cases with the exception that renal anomalies were more common in MLL2 mutation-positive cases. MLL2 carriers obviously showed more frequently a typical facial gestalt compared with non-carriers [11] .
Burke and Jones reported dysarthria and dyspraxia patients and suggested that it resulted from oral motor problems having a neurological component. In their review, 11/16 patients had significant neurological symptoms aside from mental retardation, including hypotonia and seizures. Wilson et al., similarly reported an increased incidence of neonatal complications, abnormal dentition, hypotonia, and microcephaly in non-Asian KMS patients [12].
Presence of facial muscle hypotonia, feeding difficulties and speech problems were noted in the present case which is in accordance with the literature [2,4,9].
The tendency to have length and angular imbalances in jaw development have significant implications for facial growth, occlusion and for potential orthodontic treatment. A thorough evaluation of the underlying jaw development pattern in advance of initiating any orthodontic treatment has to be carried out. The biting pattern of the teeth is most often a result of the growth pattern of the jaws and not just malpositioning of the teeth. Treatment options must be carefully assessed in order to optimize outcome. Considering the pattern of the neuromuscular environment, children with KMS may not have the same options for orthodontic treatment as typically developing children where sometimes during growth muscle forces can be harnessed to improve the bite and jaw positions [13].
Electromyography which consists of the graphic registration of the myoelectric signal represents an important tool for quantification of muscular activity at rest and during contraction. Thus, electromyographic analysis has been widely used as a diagnostic method for muscular conditions in several situations and in different muscle functions. Electromyographic data representing muscle activity during movements of the mandible (e.g., chewing) are the result of several variables operating simultaneously-i.e., continual variation in muscle length, bite dimension, and temporomandibular joint axis [14].
In the present case, maxillary recession and mid-face hypoplasia predisposed the patient to development of a small dental arch and malocclusion which included forwardly placed teeth with incompetent lips, anterior cross bite with angles class II molar relation. This was further complicated by the presence of hypotonia of the facial muscles and wasting of the muscles of tongue on right side. Thus, it was required to know the tonicity of facial and masticatory muscles and also the conduction of the nerve impulses for both diagnostic and therapeutic purposes. The electromyographic studies in cases of KMS can prove to be an essential diagnostic tool and can help us predict the prognosis of the therapy [15].
As per our literature review, we have come across many electromyographic studies performed for malocclusion [16,15]. But there are no studies or cases reporting the application of the EMG studies in patients with KMS for the assessment of the facial muscle activity. In this case report the EMG study showed no resting muscle activity in the facial muscles. However, there was activity noted in the Masseter and Temporalis muscles. The compound muscle action potential on right side was decreased when compared to the left. Thus, it was inferred that there was no muscle activity present in the facial muscles. Physiotherapy along with nerve stimulation may help to increase the muscle tone and therefore aid in the orthodontic treatment outcome in KMS patients. Presently, our patient is undergoing similar therapy before starting with the orthodontic therapy.
Frontal photograph of KMS patient showing expressionless face, high arched eyebrows, drooping lower lip, anterior cross-bite, broad nose with depressed tip
Lateral photograph of the patient with KMS showing short nasal septum and associated flat tip of nose

Shows blue sclera with characteristic long eye lashes

Clinical features of Kabuli make up syndrome seen in present case
| Major features | Patients with KMS (cumulative %) | In the present case |
| Characteristic face | 100 | + |
| Long palpebral fissures | 99 | + |
| Abnormal dermatoglyphics | 96 | + |
| Short nasal septum | 92 | - |
| Persistent fingertip pad | 89 | - |
| Malformed ear | 87 | - |
| Arched eyebrows | 85 | + |
| Long eye lashes | 85 | + |
| IQ<80 | 84 | - |
| Prominent ears | 84 | - |
| Depressed nasal tip | 83 | - |
| Short 5th digit | 79 | - |
| Joint laxity | 74 | + |
| High-arched palate | 72 | + |
| Abnormal dentition | 68 | + |
| Hypotonia | 68 | + |
| Short stature (<2.0 SD) | 55 | + |
| Ptosis | 50 | + |
| Minor features | | |
| Cardiovascular anomaly | 42 | - |
| Cleft lip and/or cleft palate | 35 | - |
| Scoliosis | 32 | - |
| Deformed vertebra/rib | 32 | - |
| Blue sclera | 32 | - |
| Kidney/ urinary tract malformation | 32 | - |
| Premature thelarche | 28 | + |
| Hearing loss | 28 | - |
| Lower lip pits | 27 | - |
| Cryptorchidism | 24 | - |
| Preauricular pits | 22 | - |
| Hip dislocation | 18 | - |
| Seizures | 17 | - |
oral photograph showing wasting of the muscles of tongue on right side

Electromyography of facial muscles showing no resting muscle activity

Electromyography of temporalis and masseter showing muscle activity
Compound muscle action potential (cmaps) showing reduced amplitude of right facial nerve compared to left

Conclusion
The dental features may aid the diagnosis of this rare syndrome and form part of the diagnostic criteria. It is important that dental professionals are aware of this syndrome with its variable expressivity. EMG study is proved to be a very important diagnostic and prognostic tool and should be used by the dentist since it gives a clue to solve many malocclusion problems in children with KMS. These studies also provide great help in speech therapy for these patients. Hence, dental management is important for the overall care of KS patients, as well as the early involvement of a multidisciplinary team.
[1]. CJ McMahon, W Reardon, The spectrum of congenital cardiac malformations encountered in six children with Kabuki syndromeCardiol Young 2006 16:30-33. [Google Scholar]
[2]. MP Adam, L Hudgins, Kabuki syndrome: a reviewClin Genet 2004 67:209-19. [Google Scholar]
[3]. N Niikawa, Y Kuroki, T Kajii, Kabuki make-up (Niikawa–Kuroki) syndrome: a study of 62 patientsAm J Med Genet 1988 31:565-89. [Google Scholar]
[4]. D Genevie`ve, Atypical Findings in Kabuki Syndrome: Report of 8 Patients in a Series of 20 and Review of the LiteratureAmerican Journal of Medical Genetics 2004 129A:64-68. [Google Scholar]
[5]. D Petzold, E Kratzsch, S Optiz, S Tinschert, The Kabuki Syndrome: four patients with oral abnormalitiesEuropean Journal of Orthodontics 2003 25:13-19. [Google Scholar]
[6]. J Hou, Variable Expressivity in a Family with Kabuki Make-up (Niikawa-Kuroki) SyndromeChang Gung Med J 2004 27:307-11. [Google Scholar]
[7]. ZHS Lung, A Rennie, Kabuki syndrome: a case reportJournal of Orthodontics 2006 33:242-45. [Google Scholar]
[8]. A Subbarayan, K Hussain, Hypoglycemia in Kabuki syndromeAm J Med Genet A 2014 33(2):467-71. [Google Scholar]
[9]. CJ McMahon, W Reardon, The spectrum of congenital cardiac malformations encountered in six children with Kabuki syndromeCardiol Young 2006 16:30-33. [Google Scholar]
[10]. J Hou, Variable Expressivity in a Family with Kabuki Make-up (Niikawa-Kuroki) SyndromeChang Gung Med J 2004 27:307-11. [Google Scholar]
[11]. S Yuan, Congenital heart defects in Kabuki syndromeCardiology Journal 2013 20(2):121-24. [Google Scholar]
[12]. A Sert, ME Atabek, O Pirgon, Two new kabuki cases of kabuki make-up syndromeMarmara Medical Journal 2006 19(2):85-89. [Google Scholar]
[13]. N Niikawa, Y Kuroki, T Kajii, Kabuki make-up (Niikawa–Kuroki) syndrome: a study of 62 patients Am J Med Genet 1988 31:565-89. [Google Scholar]
[14]. D Genevie`ve, A typical Findings in Kabuki Syndrome: Report of 8 Patients in a Series of 20 and Review of the LiteratureAmerican Journal of Medical Genetics 2004 129A:64-68. [Google Scholar]
[15]. Williams Bryan J, Important Dental and Orthodontic Issues for Children with Kabuki Syndromehttp://www.google.com [Google Scholar]
[16]. SA Temtamy, EHA Aboul-Ezz, HH Afifi, AK Abdel-Aleem, AK Kamel, Phenotypic overlap between Kabuki Make-up Syndrome and the Prader-willi like phenotype of fragile-X syndromeCairo Dental journal 1996 12(1):69-75. [Google Scholar]