Senior – Loken syndrome is a rare combination of juvenile nephronophthisis and tapeto – retinal degeneration. The author describes two patients who presented with varying degrees of retinal dystrophy and renal insufficiency in their second decade of life. Both the patients presented with severe renal failure requiring hemodialysis. The first patient had early onset progressive retinal degeneration leading to childhood blindness whereas the second patient had asymptomatic retinitis pigmentosa. These cases are presented to highlight the spectrum of eye manifestations of Senior – Loken syndrome. This report also stresses the need for fundus evaluation in patients with chronic kidney disease presenting in second decade of life even if asymptomatic.
Familial juvenile nephronophthisis, Hereditary renal - retinal dystrophy, Retinitis pigmentosa, Renal – retinal syndrome
Case History 1
A 12-year-old female patient was referred to our hospital with history of vomiting, oliguria and facial puffiness of five days duration. Patient had one episode of generalized tonic-clonic seizures of two minutes duration just before the arrival to our hospital. Past history was significant for polyuria of four years duration
She was born to 2nd degree consanguinous marriage and had normal developmental milestones. She had normal eye to eye contact till nine months of age after which she was found to have lack of fixation of eyes. At four years of age she was unable to see the board at her school. Her neurological evaluation then was otherwise normal and neuroimaging was unremarkable. She was enrolled in a blind school at six years of age. Family history was not contributory.
On examination, her height and weight were 121 cm and 18 kg (both < 3rd percentile for her age and sex). She was pale with blood pressure of 80/60 mm of Hg (normal for her age) and pulse rate of 104 per minute. She had knock knees with widening of both the wrists. Her limbs were hypotonic and she walked with broad based gait. She had bilateral horizontal nystagmus, and her visual acuity was reduced to perception of hand movements bilaterally. Her fundi examination showed mild pallor.
Her urine examination showed nil proteinuria with no active sediments. Investigations showed hemoglobin 6.1gms/dl, urea 196 mg/dl, creatinine 8.6 mg/dl, sodium 145meq/L, potassium 5.4meq/L, albumin 3.5g/dl, alkaline phosphatase 232 IU/L, corrected calcium 7.6 mg/dl, Phosphorus 5.8 mg/dl, and iPTH – 582 pg/ml. Ultrasound abdomen showed bilateral small kidneys with increased echogenecity and few small cysts in both the kidneys. Electroretinogram (ERG) revealed bilateral unrecordable rod and cone response suggestive of retinal dystrophy.
Case History 2
A 16-year-old male was admitted to our hospital with complaints of anorexia, vomiting, pedal edema, oliguria of 10 d duration. He was born to 2nd degree consanguineous marriage and his developmental milestones were normal. His past history was significant for polyuria and polydipsia of seven years duration.
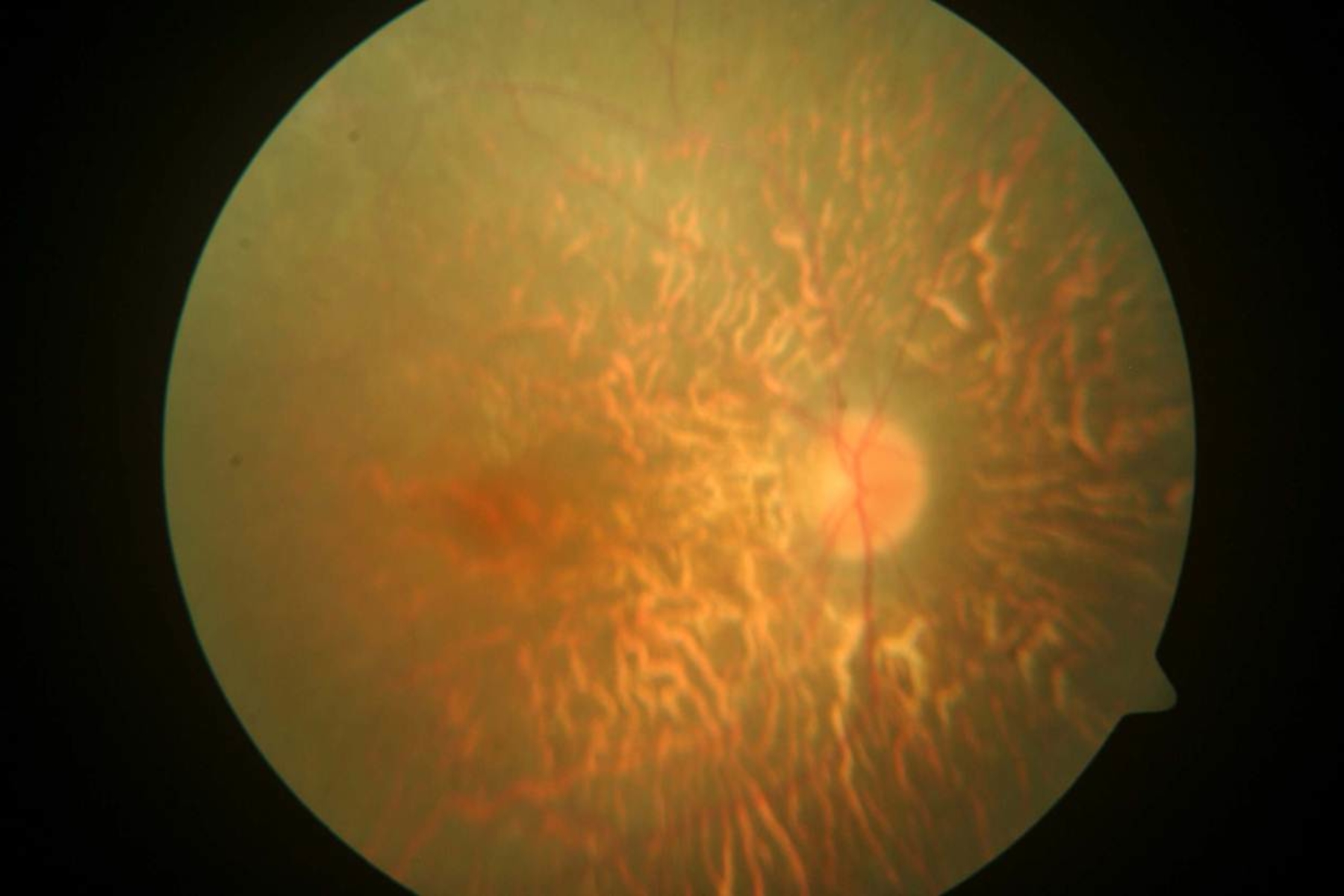
On examination, he was pale with bilateral pedal edema. His height and weight were 138 cm and 26.5 kg (both < 3rd percentile for her age and sex). His blood pressure was 120/80 mm of Hg in his both upper limbs. Physical examination revealed absent secondary R1sexual characters with knock knees and widened wrists bilaterally. Ophthalmic examination showed squint with no nystagmus. Fundi examination was conspicuous for pigmentary clumps suggestive of retinitis pigmentosa [Table/Fig-1]. Rest of the nervous system examination was normal.
Urinalysis showed proteinuria with no active sediments. His blood investigations showed hemoglobin 7.5g/dl, urea 298 mg/dl, creatinine 9.0 mg/dl, corrected calcium 7.6 mg/dl, phosphorus 4.0 mg/dl, and alkaline phosphatase 734 U/L. Ultrasound abdomen revealed bilaterally echogeinc kidneys with loss of corticomedullary differentiation.
Both the patients presented with features suggestive of chronic interstitial nephritis and retinopathy in their second decade of life. The retinopathy was of early onset and severe in the first patient whereas late onset and mild in second patient. Based on the clinical picture of combination of retinopathy and nephronophthisis, the two patients were diagnosed as having Senior-Loken syndrome. They were started on haemodialysis and their parents refused renal transplantation due to financial reasons.
Discussion
Senior-Loken syndrome is a rare syndrome of retinopathy and nephronophthisis which usually presents in the first two decades of life. It was first described in 1961 by Senior et al., and Loken et al., separately, who reported a combination of nephronophthisis and tapetoretinal degeneration in children [1,2]. Senior-Loken syndrome, an autosomal recessive disorder that is also referred to as hereditary renal-retinal syndrome, juvenile nephronophthisis with Leber amaurosis, and renal dysplasia and retinal aplasia. Senior-Loken syndrome has been recently included in the broad category of “ciliopathies”, a class of genetic diseases that occur due to primary ciliary dysfunction.
The retinal lesions in the Senior-Loken syndrome are variable, ranging from severe Leber’s amaurosis to a more typical retinitis pigmentosa [3]. Leber’s congenital amaurosis is a severe form of retinal dystrophy which leads to blindness in infancy, nystagmus and a diffuse atypical retinal pigmentation and pallor of the optic disc, with an early and complete extinction of the electroretinogram (ERG). Retinitis pigmentosa is characterized by bone spicule pigmentation of the retina and presents initially with night blindness which slowly progress to daytime blindness. Other ocular findings that have reported in this syndrome include cataract, Coat’s disease and keratoconus [4].
The renal manifestations of this syndrome are identical to those of isolated nephronophthisis. Polyuria, polydipsia and impaired concentrating ability are the earliest signs. It is usually insidious in onset and progresses inexorably to end-stage kidney disease before the age of 20 y. The main histological findings are tubular atrophy, interstitial fibrosis, thickening and lamellation of the tubular basement membrane [5].
The diagnosis is based on typical clinical presentation of a combination of chronic interstitial nephritis and retinopathy in second decade. There is no specific treatment for nephronophthisis. Renal transplantation is the preferred treatment for these patients.
There are very few case reports of Senior Loken syndrome from India probably due to lack of awareness of this rare condition [6-9]. Singh NP et al., reported two siblings in the same family with Senior Loken syndrome and unusual manifestations such as short status, kyphoscoliosis, short metacarpals and cutis laxa [6] . HK Aggarwal et al., reported a 19-year-old male with severe renal failure, retinitis pigmentosa, madarosis and small hands [7] . Giridhar S et al., described 11-year-old female twins with renal failure, retinitis pigmentosa and dysmorphic features of face and hands [8] . Though various other abnormalities have been described, our patients didn’t have any other unusual features.
The ophthalmic findings in our patients were important clues that led to the diagnosis of Senior-Loken syndrome. The first patient had early onset severe retinal dystrophy leading on to childhood blindness. Awareness about this syndrome could have led to early diagnosis of renal disease. Diagnosis could have been missed easily but for the ophthalmic evaluation in the second patient who was not having any ocular symptoms. The cases presented here, other than the typical combination of renal failure and retinal degeneration is notable for several reasons, including presentation with endstage renal disease, and extreme ophthalmic manifestations of the syndrome.
Conclusion
The author presented two patients who had extremes of eye manifestations of Senior Loken syndrome. Senior – Loken syndrome must be considered in patients who present with visual impairment and renal failure in the first two decades of life. Hence, ophthalmic examination should be done in all young patients with renal failure even if they are apparently normal. Patients with nephronophthisis should undergo detailed ophthalmic evaluation periodically. Similarly, children with retinal dystrophy should have regular assessments of blood pressure, urinary concentrating ability, renal parameters, and renal ultrasound scan.
[1]. B Senior, AI Friedmann, JL Braudo, Juvenile familial nephropathy with tapetoretinal degeneration. A new oculorenal dystrophyAm J Ophthalmol 1961 52:625-33. [Google Scholar]
[2]. AC Loken, O Hanssen, S Halvorsen, NJ Jolster, Hereditary renal dys¬plasia and blindnessActa Paediatr 1961 50:177-84. [Google Scholar]
[3]. D Satran, ME Pierpont, WB Dobyns, Cerebello-oculo-renal syndromes including Arima, Senior-Loken and COACH syndromes: More than just variants of Joubert syndromeAm J Med Genet A 1999 86:459-69. [Google Scholar]
[4]. JG Gleeson, LC Keeler, MA Parisi, SE Marsh, PF Chance, IA Glass, Molar tooth sign of the midbrain-hindbrain junction: Occurrence in multiple distinct syndromesAm J Med Genet A 2004 125:125-34. [Google Scholar]
[5]. V Godel, A Iaina, P Nemet, M Lazar, Retinal manifestations in familial juvenile nephronophthisisClin Genet 1979 16:277-81. [Google Scholar]
[6]. NP Singh, S Anuradha, S Gupta, SN Rizvi, R Arora, Senior-Loken syndrome with unusual manifestationsJ Assoc Physicians India 1998 46(8):740-42. [Google Scholar]
[7]. Aggarwal HK, Jain A, Yadav S, Kaverappa V, Gupta A, Senior-Loken Syndrome with Rare Manifestations: A Case ReportEurasian J Med 2013 45:128-31. [Google Scholar]
[8]. S Giridhar, R Padmaraj, P Senguttuvan, Twins with Senior-Loken syndromeIndian J Pediatr 2006 73(11):1041-43. [Google Scholar]
[9]. R Janardhanan, S Krishnakumar, Senior-Loken syndromeJ Assoc Physicians India 1997 45(11):889-90. [Google Scholar]