Klestadt’s cyst is commonly known as Nasolabial cyst, is a rare non-odontogenic, soft-tissue, developmental cyst. It accounts for around 0.7% of cysts of the jaws and 2.5% of the nonodontogenic cysts. Following its first description in 1882 by Zukuerkandl, very few cases have been documented in the literature. The cyst usually occurs in the nasolabial region, as a slowly enlarging asymptomatic swelling. As it is a soft tissue cyst, it doesn’t show any radiographic changes. Thus contrast medium can be used to visualize the definite extensions. This paper documents a case of nasolabial cyst which was successfully treated in which a radiographic contrast medium was used in order to define the actual extensions of the lesion.
Contrasts media, Klestadt’s cyst, Nasolabial cyst, Soft tissue cyst
Case Report
A 45-year-old female patient reported with the chief complaint of swelling on left side of the upper lip and nose since five years. The swelling was gradual in onset, which was initially smaller in size and gradually increased to attain the present size. There was no associated symptom like pain, paresthesia or any discharge from the swelling. The patient related that the first treatment for the swelling was endodontic therapy of the upper left central and lateral incisor, but it was not successful in reducing the swelling. The patient also mentioned difficulty in breathing through the left nostril. She was otherwise in good health and her medical history was not contributory.
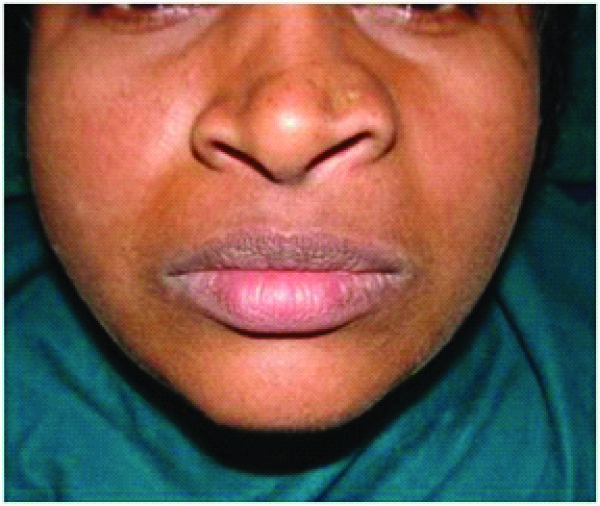
On extra-oral examination a diffuse swelling measuring about 2x3 cm was seen in the region of left nasolabial fold and a slight elevation of the nasal alae with obliteration of naso-labial sulcus [Table/Fig-1]. The floor of left nostril was raised, causing obliteration and thus difficulty in breathing. The overlying skin was stretched with no secondary changes. On palpation the swelling was soft to firm in consistency, slightly tender, fluctuant and freely mobile over the underlying bone.
Raised left ala of nose, obliterated naso-labial sulcus.
Intra-orally a solitary diffuse swelling is seen, obliterating the left labial vestibule in relation to 21, 22 region. The overlying mucosa was normal and the teeth in vicinity of the swelling, revealed access canal opening and restoration [Table/Fig-2].
Discolored left central incisor; swelling in the left side of labial sulcus with obliteration of labial sulcus.

Aspiration biopsy was done through intra-oral route which yielded around 3ml of creamish-white fluid. After aspiration an equal amount of radiopaque contrast dye (Urografin 76%) was infused into the swelling and OPG & Lateral cephalogram radiographs were taken in order to visualize the relation of swelling to the underlying bone [Table/Fig-3,4].
Lateral cephalograph showing the extra-osseous nature of swelling and its antero-posterior extent.

OPG showing mesio-lateral extent of the swelling
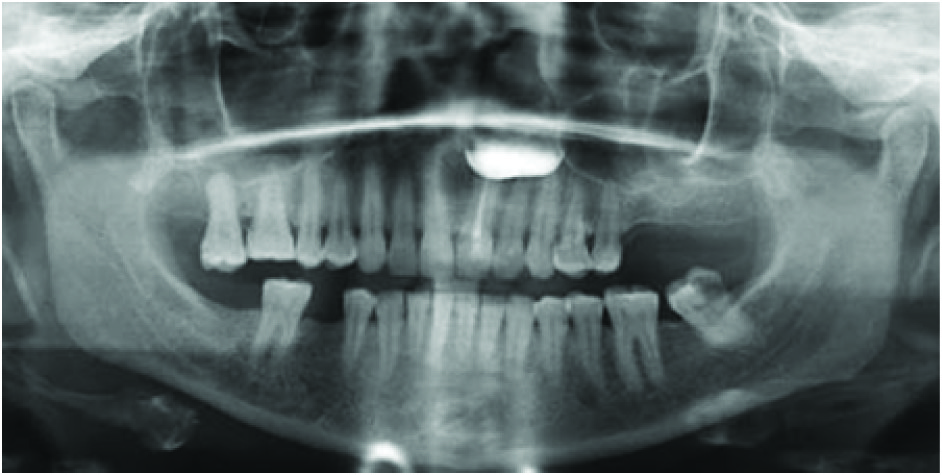
The radiographs with contrast medium revealed an oval shaped radiopaque shadow in the nasoalveolar region of the maxilla, suggestive of the extraosseous nature of the swelling and assisted in differential diagnosis from intra-osseous lesions. The radiographs provided the real extension of the lesion and helped with surgical planning.
The cyst was excised by intra-oral surgical method under general anesthesia in total without any damage to cystic wall and nasal mucosa [Table/Fig-5]. Histopathology revealed cystic wall composed of fibrous tissue and pseudostratified cylindrical epithelium along with few goblet cells, suggestive of nasolabial cyst [Table/Fig-6]. The patient was followed-up postoperatively for one year. There were no postoperative symptoms, and the lesion did not recur within this period.

Histopathological picture

Discussion
Nasolabial cyst is a rare non-odontogenic cyst arising in the nasoalveolar region of the face. The first case of nasolabial cyst was reported by McBride in 1892. In 1953, Klestadt investigated nasolabial cysts in detail, after which the lesion became named Klestadt’s Cyst in his honor [1].
Several theories regarding the etiology of this lesion are put forth, of which the original theory was the one reported by Klestadt in 1953. According to him, the cyst is derived from epithelium trapped in the line of fusion between the lateral nasal and maxillary processes. It is thought that its pathogenesis is related to a period between the 4th and 8th weeks of intra-uterine life; at this time the maxillary process of the second brachial arch forms the base of the nose and the nasal alae. Midline fusion between each maxillary lateral palatine process and the base of the septum forms the hard palate, at the same time initiating formation of the nasal fossa. Aberrant changes at any of these fusion points may give rise to a cyst [2]. However, the more widely supported theory suggests that the cyst arises from nasolacrimal duct epithelium. The cyst develops from cell remains derived from the lower opening of the nasolacrimal duct. Pseudostratified columnar epithelium lines this duct, and is similar to that often found on the walls of nasolabial cysts [2].
The clinical features of nasolabial cyst are fairly typical. Patients usually complain of a swelling adjacent to the nose. The cyst is asymptomatic unless nasal obstruction occurs or it becomes infected. The infection can spread locally and cause tenderness, swelling of the lip and cheek, and facial deformity [3]. The cyst is most commonly seen in adults, with peak prevalence in the 4th & 5th decades of life. There is a significant predilection for women, with a female to male ratio of 3:1. In our case all the features were in agreement with the observations in the literature.
The differential diagnosis includes Nasopalatine duct cyst, periapical abscess, periapical granulomas, periapical cyst, odontogenic cysts and tumors, epidermal inclusion cyst, frunculosis of base of the nose and neoplasms of base of the nose. Schwannoma and hemangioma, which are benign soft tissue masses, should also be considered in the differential diagnosis of masses in the nasoalveolar region [4].
Odontogenic cysts and tumors are intra-osseous and are usually more expansile. The radiographs with contrast medium demonstrated extraosseous nature of lesion and thus helped in differentiate from odontogenic lesions.
Conventional diagnostic radiographs are indispensable to demonstrate the extent, internal characteristics and correlation with the surroundings of the lesion. Because nasolabial cyst is a soft tissue lesion, there may not be any evidence of its presence in conventional radiographs. However, owing to its expansile nature, it can cause bone erosion of the adjacent maxilla, resulting in radiographic identification in some conventional radiographs. Occasionally, erosion of the anterior maxillary labial cortex is seen, probably as a result of longstanding cyst pressure [1,5].
The visualization of cyst by injecting radiographic contrast medium is a safe, low cost, simple and rapid method [6]. This procedure is precise for visualizing the definite extensions of the lesion, mainly in those cases when plain radiographs may not show any detectable changes and where advanced radiographic techniques (CT, MRI etc) cannot be accessed and patient cannot afford for expensive investigations.
The radiographs with contrast medium, preferably two different views perpendicular to each other may provide information on height, width and depth of the cyst.
The procedure is safe as the radiographic contrast medium may not cause allergy for the patients. Whilst the injection of radiographic contrast medium could rupture the borders confining the cyst and then cause dissemination of bacteria into other facial planes, it can only happen when a different volume of radiographic contrast medium from the fluid aspirated is injected. Hence the technique must be made at the same appointment as the surgery [5,6].
Injection of sclerotic substances, marsupialization and surgical removal may be considered for treatment. Thus far, surgical excision through intraoral approach has been the most popular and well-established procedure for the management of nasolabial cysts. Su et al., described the use of trans-nasal endoscopic marsupialization as an option in managing nasolabial cysts [1]. However, unlike some of the large intra-osseous cysts, this soft-tissue lesion does not respond to marsupialization and surgical excision is the treatment of choice. Because this cyst is usually closely related to the floor of the nose, perforation of the nasal mucosa may be expected during surgery. Whilst very small perforations are caused, they can be left untreated; however, larger ones must be sutured [3]. In the present case, there was no perforation of nasal mucosa and the lesion healed without any complications and there was no recurrence of the lesion postoperatively in one year.
Conclusion
As the nasolabial cyst is a soft tissue cyst, contrast radiography is an option of imaging in defining the borders and extent. It further helps in accurate diagnosis and surgical planning. In this case report radiographic contrast medium was successfully used in evaluating the extent of nasolabial cyst and for differentiating it from other Intra-osseous lesions. It is practical to make use of this procedure whenever advanced radiographic techniques are not affordable.
[1]. Wei-Chieh Chao, Chi-Che Huang, Po-Hong Chang, Management of Nasolabial Cysts by Transnasal Endoscopic MarsupializationArch Otolaryngol Head Neck Surg 2009 135(9):932-35. [Google Scholar]
[2]. Raphael NA, Vitor JB, Reinaldo J, Nasolabial cyst: presentation of a clinical case with CT and MR imagesRev Bras Otorhinolaryngology 2008 74(3):467-71. [Google Scholar]
[3]. Jae Yong Lee, Byoung Joon Baek, Jang Yul Byun, Comparison of Conventional Excision via a Sublabial Approach and Transnasal Marsupialization for the Treatment of Nasolabial Cysts: A Prospective Randomized StudyClin Exp Otorhinolaryngol 2009 2(2):85-89. [Google Scholar]
[4]. Nixdorf Donald R, Peters Edmund, Lung Kevin E, Clinical Presentation and Differential Diagnosis of Nasolabial CystJ Can Dent Assoc 2003 69(3):146-49. [Google Scholar]
[5]. Tanimoto K, Kakimoto N, Nishiyama H, MRI of nasoalveolar cyst: Case reportOral Surg Oral Med Oral Pathol Oral Radiol Endod 2005 99:221-24. [Google Scholar]
[6]. Amaral MP, Silva Fonseca LM, Mesquita RA, Nasolabial cyst with radiographic contrast medium: Report of two casesDentomaxillofacial Radiology 2005 34:256-58. [Google Scholar]