Pilomatrixoma Masquerading as Metastatic Adenocarcinoma. A Diagnostic Pitfall on Cytology
Divya Sharma1, Shipra Agarwal2, L Shyama Jain3, Vinay Kamal4
1 Resident, Department of Pathology, Maulana Azad Medical College and Associated LNJP Hospital, New Delhi, India.
2 Assistant Professor, Department of Pathology, Maulana Azad Medical College and Associated LNJP Hospital, New Delhi, India.
3 Director Professor, Department of Pathology, Maulana Azad Medical College and Associated LNJP Hospital, New Delhi, India.
4 Director Professor, Department of Pathology, Maulana Azad Medical College and Associated LNJP Hospital, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Divya Sharma, Senior Resident, Department of Pathology, Maulana Azad Medical College, Bahadur Shah Zafar Marg, New Delhi-110002, India. Phone : 91-8860998489, E-mail : sharmadivya20@rediffmail.com
Pilomatrixoma (Px) is a relatively uncommon slowly growing, benign skin appendageal tumor with a wide morphological spectrum, and can pose diagnostic difficulties especially in cases with unusual clinical presentation.
We report a case of young male who presented with a nodule over anterior abdominal wall, fine needle aspiration cytology (FNAC) revealed predominantly small cells in focal acinar pattern suggestive of metastatic carcinoma; however, histopathological diagnosis was Px. The case highlights the diagnostic pitfalls on cytology due to limited morphology.
Adnexal tumor, Fine needle aspiration cytology, Pilomatrixoma
Case Report
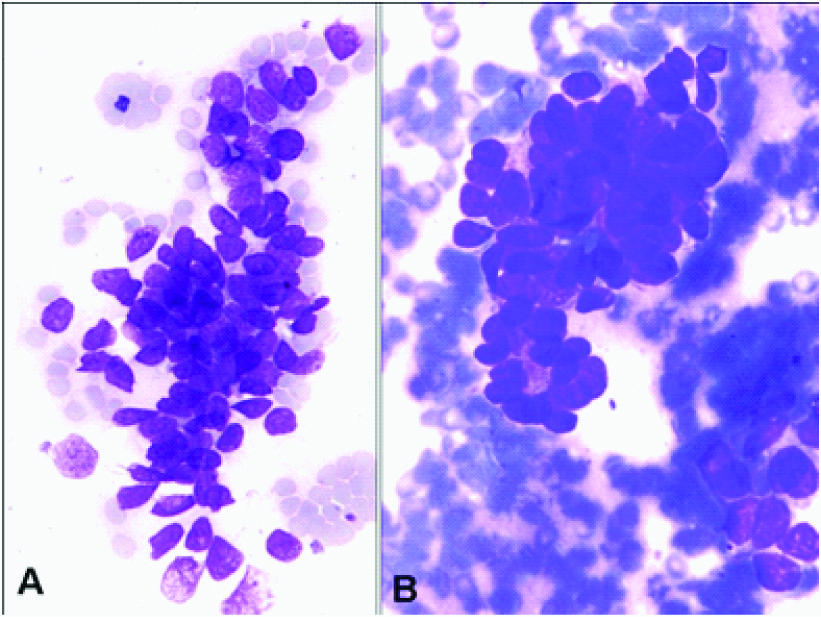
A 31-year-old male presented with a painless swelling in the anterior abdominal wall since eight months. On examination, the nodule was hard, freely mobile and measured 0.5x0.5 cms in size. FNAC was performed as per the standard technique using 23 gauze needle The Giemsa stained smears were moderately cellular, showed tissue fragments, small clusters, focal glandular arrangement and few singly dispersed small cells in a hemorrhagic background. The cells were round to ovoid with high nuclear cytoplasmic (N:C) ratio, scant basophilic cytoplasm and finely dispersed chromatin and small inconspicuous nucleoli [Table/Fig-1]. There was no mitosis or necrosis. Based on these features, a possibility of metastatic adenocarcinoma (MC) was suggested.
FNA smear showing groups of small cells with scant cytoplasm and focal acinar pattern. Giemsa stain X 400
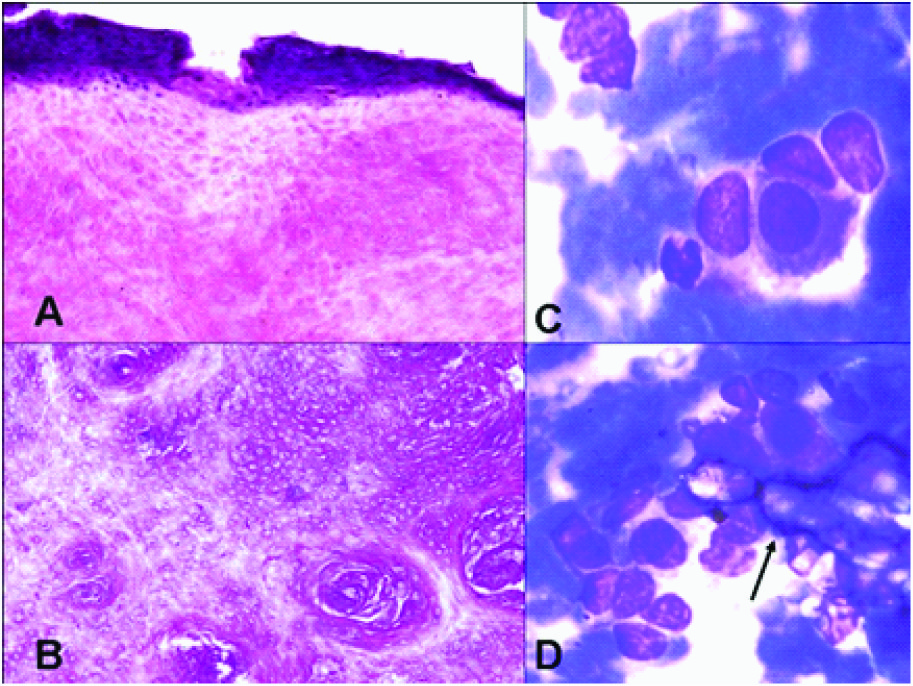
Patient was investigated further, however no evidence of primary elsewhere was found. Wide local excision of the nodule was performed, a skin covered mass measuring 2x1x0.8cm was received. Histological sections revealed sheets of ghost cells with many foreign body giant cells (FBGC). At the periphery of these, few small basaloid cells were noted [Table/Fig-2a,b]. Histological features were diagnostic of a pilomatrixoma. FNA smears were reviewed after histological diagnosis; the small cells in clusters and acinar pattern in smears were the basaloid cells seen in sections and were misinterpreted as MC. Moreover, interestingly; only one of the multiple smears showed occasional mature squamous cell and focal calcification, suggestive of squamous differentiation compatible with pilomatrixoma [Table/Fig-2c,d].
Biopsy of nodule showing small basaloid cells at the periphery with underlying ghost cells and whorling (A,B). (H&E X 400). Review of the FNA smears showing occasional squamous cell (C) and focal calcification shown by arrow (D). Giemsa stain X 400
Discussion
Pilomatrixoma most commonly occurs in head and neck region and rarely at other sites (upper extremity, trunk and lower extremities)[1–3]. In a recent study on 25 cases of pilomatrixoma, most cases were in head and neck region and none in the abdominal wall [4]. Clinically, it is asymptomatic, deep seated, firm, subcutaneous mass adherent to the skin, range 0.5- 3 cms in size and rarely as large as five cms [5].
The clinical differential diagnosis of pilomatrixomas usually includes sebaceous cyst, ossifying haematoma, giant cell tumour, dermoid cyst, chondroma, degenerating fibroxanthoma, foreign body reaction, and osteoma cutis.
Histological features of pilomatrixoma show two types of epithelial cells: small basaloid cells and eosinophilic shadow or ghost cells without nuclei [3]. Early lesions show predominantly basaloid cells in islands. As the lesions mature, the basophilic cells acquire more cytoplasm and lose their nuclei to become ghost cells which may calcify subsequently.
The cytological diagnosis does not pose any difficulty in presence of characteristic morphology as in histopathology (basaloid cells, ghost cells, FBGC and calcification) [6,7]. But all these features may not be present in smears always, and may lead to diagnostic dilemma. It is often misdiagnosed on cytology. In the series by Ieni et al, less than 50% of cases were diagnosed correctly on cytology; remaining being misdiagnosed as round cell tumour, epidermal inclusion cyst and squamous epithelial tumour [Table/Fig-3] [4]. Smears showing predominantly basaloid cells have been often misdiagnosed as malignancy, because of their high N:C ratio, hyperchromatic nucleus and prominent nucleolus. On the other hand the lesions with predominance of squamous cells, ghost cells, and FBGC can be misdiagnosed as squamous cell carcinoma (SCC). Also the background of cell debris may be misinterpreted as tumour diatheses. Such cases have been in the past mistaken for SCC, basal cell carcinoma, MC, mucoepidermoid carcinoma or malignant appendagal tumour [6–10] [Table/Fig-3]. Ghost-cell rich smears mimic epidermal inclusion cyst or giant cell lesions [3,4].
Cases of pilomatrixoma misdiagnosed on cytology
| Year | Author Ref | No. of cases | Site | Cytological diagnosis |
|---|
| 2001 Lemos MM et al., [7] | 1 | Neck | Poorly differentiated malignant tumor, ?Squamous cell carcinoma |
| 1 | Face | Carcinoma, possibly small cell type |
| 1 | Face | Basal cell carcinoma vs pilomatrixoma |
| 2 | Face, neck | Atypical epithelial proliferation; suspicious for malignancy |
| 2 | Neck, Arm | Benign Epithelial tumor/cyst possibly skin adnexal tumor |
| 2007 | Preethi TR et al., [8] | 1 | Posterior neck | Metastatic adenocarcinoma |
| 2007 | Sivakumar S [9] | 1 | Neck | Mucoepidermoid carcinoma of submandibular gland |
| 2010 | Pant I et al., [3] | 2 | Back, ear lobe | Dermoid cyst |
| 2010 | Agrawal L et al., [6] | 1 | Neck | Round cell tumor |
| 2012 | Gupta V et al., [10] | 1 | Neck | Malignancy |
| 2012 Ieni A et al., [4] | 2 | Cheek; foot | Small cell tumour |
| 4 | Chest, scalp, thigh | Epidermal cyst |
| 1 | Upper brow | Atypical epithelial proliferation |
| 1 | Upper brow | Trichoepithelioma |
| 1 | Parietal | Basal epithelial tumor |
| 1 | Scalp | Squamous epithelial tumor |
| 1 | Thigh | Sebaceous cyst |
| 4 | Cheek, temporal, upper brow, arm | Not determine |
| 2013 | Current case | 1 | Abdominal wall | Adenocarcinoma metastasis |
In the present case, there was a gap of about one month between the FNAC and excisional biopsy. This may be the reason for the discordance between the cytological and histopathological features, as pilomatrixoma is known to mature over time. In addition, sampling error with limited morphology may have caused the misinterpretation. However, despite the site being atypical, the long history of eight months and the young age should have been considered against the diagnosis of MC on FNAC.
Treatment is surgical resection with wide margins of 1–2cm to minimize the risk of local recurrence. Recurrences after surgery are rare, with an incidence of 0% to 3% [11]. Pilomatrixoma being a benign lesion has a good prognosis.
Conclusion
To conclude, the cytopathologist should be aware of this benign epithelial lesion commonly misinterpreted as malignant. Possibility of pilomatrixoma should always be considered while reporting cytological smears from any subcutaneous swelling so as to avoid misdiagnosis and undue stress to the patient. A meticulous screening for mature squamous cells can help in clinching the diagnosis. Definitive diagnosis on FNAC is crucial and prevents unnecessary investigations and radical surgery.
[1]. Kumaran N, Azmy A, Carachi R, Pilomatricoma-accuracy of clinical diagnosisJ Pediatr Surg 2006 41:1755-58. [Google Scholar]
[2]. Yencha MW, Head and neck pilomatricoma in the pediatric age group: a retrospective study and literature reviewInt J Pediar Otorhinolaryngol 2001 57:123-28. [Google Scholar]
[3]. Pant I, Joshi SC, Kaur G, Kumar G, Pilomatricoma as diagnostic pitfall in clinical practice: report of two cases and review of literatureInd J Dermatol 2010 55:390-92. [Google Scholar]
[4]. Ieni A, Todaro P, Bonanno AM, Limits of fine needle aspiration cytology in diagnosing pilomatrixoma: a series of 25 cases with clinico- pathologic correlationInd J Dermatol 2012 57:152-55. [Google Scholar]
[5]. Klein W, Chan E, Seykora JT, Tumours of the epidermal appendages. In: Elder DE, Elenitsas R, Johnson BL, Murphy GF, editorsLever’s histolpathology of the skin 2005 9th edPhiladelphiaLippincott, Williams and Wilkins:879 [Google Scholar]
[6]. Agrawal L, Kaur P, Singh J, Singh N, Pilomatrixoma misdiagnosed as round cell tumour on fine-needle aspiration cytologyInd J Cancer 2010 47:483-85. [Google Scholar]
[7]. Lemos MM, Kindblom LG, Meis-Kindblom JM, Ryd W, Willén H, Fine needle aspiration features of pilomatrixomaCancer 2001 93:252-56. [Google Scholar]
[8]. Preethi TR, Jayasree K, Abraham EK, A case of pilomatrixoma misdiagnosed as metastatic carcinoma on fine needle aspiration cytologyJ Cytol 2007 24:207-08. [Google Scholar]
[9]. Sivakumar S, Pilomatrixoma as a diagnostic pitfall in fine needle aspiration cytology: A case reportActa Cytol 2007 51:583-85. [Google Scholar]
[10]. Gupta V, Marwah N, Jain P, Diagnostic pitfalls of pilomatricoma on fine needle aspiration cytologyIranian J Dermat 2012 15:59-61. [Google Scholar]
[11]. Chuang CC, Lin HC, Pilomatrixoma of the head and neckJ Chin Med Assoc 2004 67(12):633-36. [Google Scholar]