Evaluation and Comparison of Anticonvulsant Activity of Telmisartan and Olmesartan in Experimentally Induced Animal Models of Epilepsy
Pushpa V H1, Padmaja Shetty K2, Suresha R N3, Jayanthi M K4, Ashwini V5, Vaibhavi P S6
1 Associate Professor, Department of Pharmacology, JSS Medical College, Mysore, India.
2 PG Student, Department of Pharmacology, JSS Medical College, Mysore, India.
3 Professor, Department of Pharmacology, JSS Medical College, Mysore, India.
4 Professor, Department of Pharmacology, JSS Medical College, Mysore, India.
5 PG Student, Department of Pharmacology, JSS Medical College, Mysore, India.
6 PG Student, Department of Pharmacology, JSS Medical College, Mysore, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Padmaja Shetty K, No.527, 5th Main, 4th Cross, Vijaya Bank Colony, Bilekahalli, Bannerghatta Road, Bangalore – 560076, India. Phone : 9448862850, E-mail : padmajaalva@gmail.com
Background: Epilepsy is one common neurological disorder requiring newer targets and newer drugs for its efficient management. In the recent days brain renin angiotensin system has gained immense importance because of its involvement in seizure regulation.
Objective: To evaluate and compare antiepileptic activity of different doses olmesartan and telmisartan on MES and PTZ induced seizure models.
Materials and Methods: Swiss albino mice weighing around 25-30g of either sex were divided into 6 groups: Control ( Distilled Water- 10ml/kg), Standard – Sodium valproate (40mg/kg), O1 – Olmesartan (2.5mg/kg), O2 – Olmesartan (5mg/kg), T1 - Telmisartan (5mg/kg), T2 – Telmisartan (10mg/kg). After 1hour of administration of control , test and standard drugs (orally), convulsions were induced by administering PTZ (70mg/kg – i.p.) in PTZ model. Seizure latency was the parameter recorded. In MES model, suppression of tonic hind limb extension was taken as measure of efficacy.
Result: The results were analysed by one-way-ANOVA followed by Bonferroni’s multiple comparison test. In MES test, dose dependently olmesartan and telmisartan significantly reduced the duration of tonic hindlimb extension in comparison to control (p<0.05). T2 – 9 + 0.89secs significantly reduced the tonic hind limb extension compared to other test groups (p<0.05). The percentage inhibition of seizure was T2-44.3%, O2-28.2%, T1-17.5%, O1- 12.3% respectively. In PTZ test, dose dependently olmesartan and telmisartan produced significant increase in seizure latency (p<0.05). T2 - 206.6+9.83secs significantly increased seizure latency compared to other test groups (p<0.05). Percentage protection from seizure is T2-52.6%, O2- 45.13%, T1- 37.5%, O1- 38.4% respectively.
Conclusion: AT1 receptor antagonist, telmisartan and olmesartan in a dose dependent manner showed increase in antiepileptic activity. Temisartan at higher dose produced significant antiepileptic activity in comparison to olmesartan.
Antiepileptic activity, AT1 Receptor, MES model, Olmesartan, PTZ Model, Telmisartan
Introduction
Epilepsies are frequently devastating disorders characterised by paroxysmal, abnormal, excessive or synchronous neuronal activity in the brain with 5-10% of the population manifesting atleast one seizure with the highest incidence occurring in early childhood and late adulthood [1]. Though there are many antiepileptic agents available for treatment of epilepsy, there is still need of more efficacious drugs with target based approach and with lesser side effects.
Epilepsy may be associated with other comorbid conditions like hypertension, diabetes, renal disorders etc. Many ongoing researches have shown that drugs such as ACE inhibitors, calcium channel blockers, AT II receptor antagonist etc used for these disorders may be involved in seizure prevention. Angiotensin II receptor subtypes have been the recent target molecules studied in various experimentation on neuropsychiatric disorders.
Brain has its own intrinsic renin angiotensin system. Brain RAS has been implicated in functions including regulation of cerebral blood flow, cerebroprotection, stress, depression, seizure, nociception, alcohol consumption, memory consolidation with possible roles in the aetiology of alzheimer’s disease, parkinson’s disease and diabetes [2]. Angiotensin II has neurotransmitter role in CNS as well as it regulates other neurotransmitters such as GABA, NA, 5 HT, Ach release etc [3]. Angiotensin II inhibits GABAergic synaptic transmission in dorsolateral periaqueductal gray neurons through activation of presynaptic AT1 receptors [4]. Hence, ACE inhibitors and AT1 receptor antagonist can facilitate GABAergic transmission which is useful in seizure prevention.
Angiontensin receptor antagonists like telmisartan and losartan were found to enhance the anticonvulsant action of valproate [5], lamotrigine [6] and topiramate [6] in the mouse models of maximal electroshock [5]. AT1 receptor antagonist losartan showed anticonvulsant activity in pentylenetetrazole seizure test [7].
In another study it was shown that losartan significantly increased the seizure threshold for gabapentin [8]. Telmisartan elicited significant depression like effects in forced swim test probably by unopposed AT2 receptor stimulation because of complete blockade of AT1 receptor even at low doses of telmisartan [9]. This mechanism can also contribute to the anticonvulsant activity of these drugs.
In a rat model of epilepsy it was found that components of RAS namely ACE and AT1 receptor were upregulated in the brain following repetitive seizures. Epileptic animals treated with clinically used doses of losartan and enalapril decreased seizure severities significantly [7]. Treatment with the AT1 receptor blocker, telmisartan had neuroprotective effect by reduction of local angiotensin II expression, blockade of AT1 receptor and relative upregulation of AT2 receptor function.
With all the above studies suggesting involvement of AT1 receptors in seizure regulation, present study was undertaken to study and compare the antiepileptic activity of two commonly used antihypertensive drugs telmisartan and olmesartan in clinically used doses in animal models of epilepsy.
Materials and Methods
Albino mice of either sex of average weight 25-30gm aged 3-4 mnth were bred in central animal house. They were housed in groups of three in clean polypropylene cages with 12 h light/dark cycle at 25±2°C and 65±5% humidity. They had access to food (standard pellet diet, Hindustan Lever Ltd) and water. All experiments were carried out between 11 AM and 3 PM. The ethical clearance was obtained from the Institutional Animals Ethical Committee and all the experiments have been carried according to CPCSEA guidelines.
Test drugs Olmesartan (2.5mg/kg and 5mg/kg), Telmisartan (10mg/kg and 5mg/kg) and standard drug Valproic acid (40mg/kg) were used. Distilled water (10ml/kg) was used as vehicle. The vehicle, standard drug and test drugs were administered orally.
Mice were randomly divided into six groups with six animals in each group. These six groups were used for MES test. After a wash period of 2 days the same six groups were used for PTZ test. Test drugs, vehicle and standard drug were administered orally 1 h prior to conducting MES and PTZ tests.
Evaluation of Antiepileptic Activity
Maximal electroshock induced seizures
Electrical stimulation is applied via ear electrodes with a current strength of 50 mA for 0.2 sec .The resultant seizure passes through various phases; phase of tonic limb flexion (1.5 sec duration), phase of tonic limb extension (10 s duration), finally followed by variable short clonic interval which may lead to asphyxial death in some animals. Twenty four hoor before testing of anticonvulsants (to avoid any possible kindling effect) the animals are pre-screened for their ability to develop full tonic extension in the maximal electroshock test. Suppression of tonic hind limb extension is taken as measure of efficacy in this test.
Pentylenetetrazole (PTZ) Induced Convulsion
One hour after test drugs and standard drug administration, 70 mg/kg pentylenetetrazole is injected intraperitonially. Each animal is placed into an individual plastic cage for observation lasting 30 min. Within 30 min they develop a sequence of excitement, myoclonic jerks, clonic seizures, one or more maximal tonic seizures followed by recovery or some animals may succumb to death. Seizure latency and abolition of clonic seizures with loss of righting reflex will be taken as index of protection.
Statistical Analysis
The effect of olmesartan and telmisartan in two different doses on MES and PTZ models of seizure induction were expressed as mean ± SD. Percentage inhibition of seizure was calculated respectively. Data was analysed using one-way-ANOVA followed by Bonferroni’s multiple comparison tests. p-values <0.05 were considered significant.
Results
Maximum electroshock induced seizures
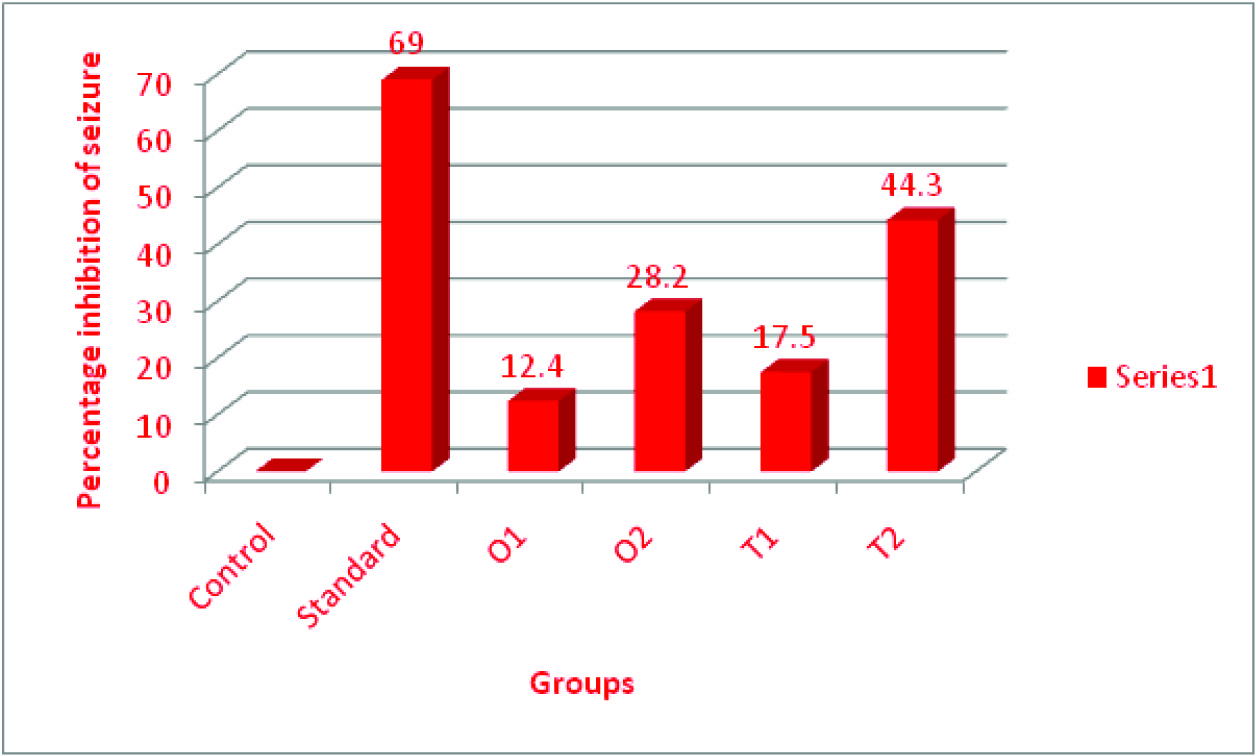
The standard drug sodium valproate significantly suppressed the tonic hind limb extension phase 5+ 0.63 secs with no clonus in comparison to control group. Olmesartan (O1 & O2) and telmisartan (T1 & T2) in a dose depedent manner significantly reduced the duration of hindlimb extensor phase [Table/Fig-1] in comparison to control. T2 significantly decreased the duration of tonic hind limb extension in comparison to T1, O1 and O2. The percentage inhibition of seizure by T2 is 44.3%. Results of MES test on T1, T2, O1 and O2 is shown in [Table/Fig-1,2].
Effect of telmisartan and olmesartan on duration of tonic hind limb extension on MES model
| Groups | Duration of tonic hind limb extension(secs) |
|---|
| Control | 16.16 ± 2.5 |
| Standard | 5 ± 0.63 |
| O1 | 14.16± 0.75 |
| O2 | 11.6 ± 0.51 |
| T1 | 13.33 ± 1.36 |
| T2 | 9 ± 0.89 |
Values are expressed as mean + SD. Statistical analysis of data was carried out by one way ANOVA followed by post hoc Bonferroni’ s multiple comparison tests., *p-value < 0.05 - significant., Percentage inhibition of seizure is measured in comparison to control
Percentage of inhibition of seizure by telmisartan and olmesartan on MES model
PTZ induced seizures
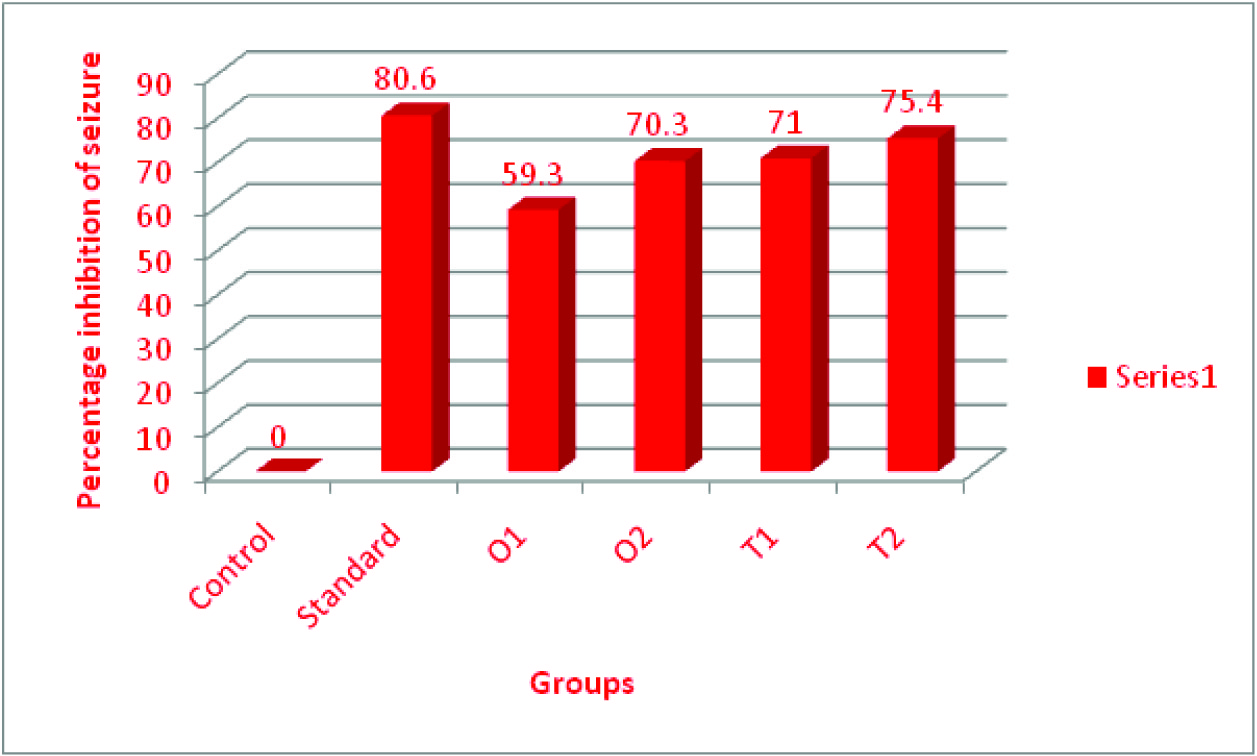
In PTZ model, seizure latency by two different doses of Olmesartan and telmisartan is significantly increased in comparison to control group as shown in [Table/Fig-3]. T2 significantly increased seizure latency to 206.6 + 9.83 when compared to T1, O1 and O2. Percentage protection from seizure by T2 is 52.6% in comparison to standard drug valproic acid. Results of PTZ test on T1,T2, O1 and O2 is shown in [Table/Fig-3,4].
Effect of telmisartan and olmesartan on seizure latency and duration of seizure on PTZ model
| Groups | Seizure latency(secs) | Duration of seizure(secs) |
|---|
| Control | 119 ± 9.59 | 15.5 ± 0.8 |
| Standard | 392.5 ± 26.78 | 3 ± 1.09 |
| O1 | 150.83 ± 9.17 | 6.3 ± 2.05 |
| O2 | 177.16 ± 10.4 | 4.6 ± 1.67 |
| T1 | 147.33 ± 7.44 | 4.5 ± 0.95 |
| T2 | 206.6 ± 9.83 | 3.8 ± 1.39 |
Percentage inhibition of seizure is measured in comparison to control.
Values are expressed as mean + SD. Statistical analysis of data was carried out by one way ANOVA followed by post hoc Bonferroni’ s multiple comparison tests.
*p-value < 0.05 - significant
Percentage inhibition of seizure by telmisartan and olmesartan on PTZ model
Discussion
Epilepsy is a common health problem throughout the world. Compliance with medication is a major problem because of the need for long-term therapy together with unwanted effects of many drugs. In the above study, both telmisartan and olmesartan dose dependently suppress the duration of hind limb extension in MES model. Telmisartan at dose of 10mg/kg significantly reduces this parameter in comparison to control, Sodium valproate, T1, O1 and O2. Percentage inhibition of seizure by T2 is 44.3%, O2 - 28.2%, O1- 12.4% and T1 – 17.5% with maximum inhibition of seizure produced by T2 in comparison to control on MES test. In PTZ test, percentage of inhibition of seizure by O1 – 59.3%, O2 – 70.3%, T1 – 71% and T2 – 75.4% in comparison to control. This shows that T2 produces significant inhibition of seizure in comparison to control. In PTZ test, percentage of protection from seizure in comparison to standard drug is T2 - 52.6%, O2 - 45.13%, O1 - 38.4% and T1 - 37.5% with maximum protection from seizure produced by T2 in comparison to standard drug (valproic acid).This study suggests that antiepileptic activity of AT1 receptor antagonists is dose dependent. Telmisartan has better antiepileptic in comparison to other AT1 receptor antagonists.
The brain RAS plays an important role in the regulation of neurogenic hypertension, cerebrovascular fluid homeostasis and sodium intake, strokes, epilepsy, Alzheimer’s disease , Parkinson’s disease , depression and stress disorders. Both GLT-1 protein levels and glutamate uptake were significantly enhanced in the neuron astrocyte co-cultures after treatment with AT1 receptor antagonist [10]. Renin angiotensin system(RAS) might have a crucial role in the regulation of cardiovascular and neurological functions by modulating glutamate/GABA release in the brain. AT1 receptor blockers decreased glutamate and increased GABA levels and facilitated seizure prevention. Telmisartan dissociates very slowly from the receptors once it is bound and it does not reassociate with receptor after dissociation [11]. The AT1 receptor antagonist telmisartan can penetrate the blood-brain barrier in a dose and time-dependent manner to inhibit centrally mediated effects of angiotensin II [12]. Telmisartan is more liphophilic and has greater potency at brain AT1 receptors [13]. Angiotensin II receptor subtypes, called AT1 and AT2 are engaged in action of angiotensin II. Using a rat model of epilepsy, it was found that components of the RAS, namely ACE and the AT1 receptor are up-regulated in the brain following repetitive seizures. AT1 receptors are present within the midbrain periaqueductal gray area (PAG). Stimulation of AT1 inhibits the synaptic GABA release in the PAG at the presynaptic GABAergic terminals and angiotensin II suppresses GABAergic synaptic inputs to the dorsolateral-PAG through stimulation of the presynaptic AT1 receptors [4]. AT1 receptor antagonists have neuroprotective effects at concentrations not affecting blood pressure. Stimulation of AT2 receptors can promote axonal regeneration in vivo after neuronal lesions.
Angiotensin has been shown to act upon a variety of ion channels such as voltage dependent potassium, calcium currents, non-selective cationic currents. The effects of angiotensin on these channels depend mainly on its action at AT1 receptor which is predominantly involved in neuronal excitability and seizure. Angiotensin has been shown to modulate the voltage dependent delayed rectifier potassium current (IK), and IA. Angiotensin increases total calcium current in response to AT1 receptor activation which is in turn responsible for this neuronal excitation [14].
Benzodiazepine receptors appear to be pharmacologically important as the modulator of anxiolytic, anticonvulsant and muscle relaxant activities in the central nervous system [15]. Stress promotes rapid and widespread changes in cortical BZ1 receptor expression and the stress-induced BZ1 receptor expression is under the control of AT1 receptor activity. ARBs may affect cortical GABAA receptors by modulating AT1-GABAA interactions in cortex by regulating hypothalamic paraventricular nucleus sympathetic system [16].
Reports suggest higher incidence of seizures in presence of pre-existing chronic inflammatory disorders. Cytokines so produced have been reported to influence many neurotransmitters like GABA, NA, acetyl choline as well as neuropeptides. Induction of spontaneously recurring seizure involves activation of inflammatory cytokines and related pro and anti-inflammatory gene in hippocampus. Angiotensin II is involved in regulating cytokines. AT1 receptor antagonist may provide protection from seizures invoked by this cytokines [17]. These are the various mechanisms through which AT1 receptor is involved in seizure generation and hence AT1 receptor antagonists can be used in treatment of epilepsy.
Conclusion
Renin angiotensin system forms a newer target in treatment of epilepsy. AT1 receptor antagonist’s telmisartan and olmesartan are commonly prescribed antihypertensive agents with significant antiepileptic activity. Antiepileptic activity of these agents is dose dependent. Telmisartan has better antiepileptic activity when compared to olmesartan. However, further work needs to be done to elucidate the antiepileptic activity of AT1 receptor antagonists.
[1]. Lowenstein Daniel H, Seizures and epilepsy. Dan L.Longo, Anthony S. Fauci,Dennis L Kasper, Stephen L. Hauser, Larry Jameson J, Joseph LoscalzoHarrison’s principles of internal medicine 2012 18th edNew YorkMc Graw Hill Medical:3251-70. [Google Scholar]
[2]. Vijayapandi Pandy, Harishankar Subash, Nancy Jose, Depression like effects of telmisartan in mice forced swim test: Involvement of brain monoaminergic systemJournal of Pharmacology and Toxicology 2012 7(2):87-95. [Google Scholar]
[3]. Hosseini M, Alaei H, Sharifi MR, Shafeia MS, The effects of angiotensin II and captopril on expression of morphine withdrawal signs in ratsIJPR 2007 6(3):185-91. [Google Scholar]
[4]. Jihong Xing, Jian Lu, Jianhua Li, Angiotensin II inhibits GABAergic synaptic transmission in dorsolateral periaqueductal gray neuronsNeurosci Lett 2009 455(1):8-13. [Google Scholar]
[5]. Lukawski K, Janowska A, Jakubus T, Tochman-gawda A, Czuczwar SJ, Angiotensin AT1 receptor antagonists enhance the anticonvulsant activity of valproate in the mouse models of maximal electroshockEur J Pharmacol 2010 640(1-3):172-77. [Google Scholar]
[6]. Lukawski K, Janowska A, Jakubus T, Czuczwar SJ, Interactions between angiotensin AT1 receptor antagonists and second-generation antiepileptic drugs in the test of maximal electroshockFundam Clin Pharmacol 2014 28(3):277-83. [Google Scholar]
[7]. Pechlivanova DM, Stoynev AG, Techekalarova JD, The effects of chronic losartan pretreatment on restraint stress- induced changes in motor activity, nociception and pentylenetetrazole generalised seizures in ratsFolia Med (Plovdic) 2011 53(2):69-73. [Google Scholar]
[8]. Lukawski K, Janowska A, Jakubus T, Raszewski G, Czuczwar SJ, Combined treatment with gabapentin and drugs affecting the renin-angiotensin system against electroconvulsions in miceEur J Pharmacol 2013 706(1-3):92-97. [Google Scholar]
[9]. McNamara James O, Pharmacotherapy of the epilepsies.Laurence L BruntonGoodman & Gilman’s The pharmacological basis of therapeutics 2011 12th edNew YorkMc Graw Hill Medical:583-607. [Google Scholar]
[10]. Wu X, Kihara T, Hongo H, Akaike A, Niidome T, Sugimoto H, Angiotensin receptor type I antagonists protect against neuronal injury induced by oxygen glucose depletionBr J Pharmacol 2010 161(1):33-50. [Google Scholar]
[11]. Kazushi Tsuda, Renin-Angiotensin System and Sympathetic Neurotransmitter Release in the Central Nervous System of HypertensionInternational Journal of Hypertension. Volume 2012 2012 :1-11. [Google Scholar]
[12]. Gohlke P, Weiss S, Jansen A, Wienen W, Stangier J, Rascher W, AT1 receptor antagonist telmisartan administered peripherally inhibits central responses to angiotensin II in conscious ratsJ Pharmacol Exp Ther 2001 298(1):62-70. [Google Scholar]
[13]. Culman J, Blume A, Gohlke P, Unger T, The renin-angiotensin system in the brain:possible therapeutic implications for AT1-receptor blockersJournal of Human Hypertension 2002 16:S64-70. [Google Scholar]
[14]. Kevin Jason Latchford. Electrophysiological effects of angiotensin II on hypothalamic paraventricular nucleus neurons of the rat. http://qspace.library.queensu.ca/bitstream/1974/995/1/Latchford_Kevin_J_200801_PhD.pdf [Google Scholar]
[15]. Mimaki T, Yabuuchi H, Laird H, Yamamura HI, Effects of seizures and antiepileptic drugs on benzodiazepine receptors in rat brainPediatr Pharmacol (New York) 1984 4(4):205-11. [Google Scholar]
[16]. Enrique Sánchez-Lemus, Honda Masaru, Juan M, Saavedra. Angiotensin II AT1 receptor blocker candesartan prevents the fast up-regulation of cerebrocortical benzodiazepine-1 receptors induced by acute inflammatory and restraint stressBehav Brain Res 2012 232(1):84-92. [Google Scholar]
[17]. Rao RS, Prakash A, Medhi B, Role of different cytokines and seizure susceptibility. A new dimension towards epilepsy researchIndian journal of experimental biology 2009 47:625-34. [Google Scholar]