Malignant Conversion of Oral Submucous Fibrosis in Surgically Treated Case
Rajendra Arora1, Dwarkadas Adwani2, Milind Naphade3, Bhushan Bhagat4, Abdul Qahar Qureshi5
1 Director of Amravati Cancer Hospital, Amravati, India.
2 Professor & HOD, Department of Oral And Maxillofacial Surgery, V.Y.W.S. Dental College and Hospital, Amravati, India.
3 Professor, Department of Oral And Maxillofacial Surgery, V.Y.W.S. Dental College and Hospital, Amravati, India.
4 Post Graduate Student, Department of Oral And Maxillofacial Surgery V.Y.W.S. Dental College and Hospital, Amravati, India.
5 Post Graduate Student, Department of Oral And Maxillofacial Surgery V.Y.W.S. Dental College and Hospital, Amravati, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr Bhushan R Bhagat, C/o Devidas Kadane Bhagyshri colony Camp Area, Amravati-444602, India.
Phone: +919975630997,
E-mail: bhagatbhushan10@gmail.com
Oral submucous fibrosis (OSMF) is an insidious chronic disease affecting any part of the oral cavity and sometimes the pharynx with epithelial atrophy leading to stiffness of the oral mucosa, causing trismus and inability to eat. However a more serious complication of this disease is the risk of the development of oral carcinoma.
We reported the histopathologically proven case of OSMF with initial interincisal mouth opening 2mm which was treated surgically with nasolabial flap technique but failed to follow up and could not do active mouth opening exercises. Malignant conversion of OSMF was seen in this case. This is required to assess the progress and evaluate any malignant transformation at the earliest. So, the importance of active co-operation and frequent follow up cannot be overemphasized. The purpose of this study is to emphasize the importance of regular follow up and frequent biopsies to facilitate oral examination and to check any malignant conversion after the surgery.
Follow-up, Mouth opening exercise, Malignant transformation, Nasolabial flap, Oral submucous fibrosis
Case Report
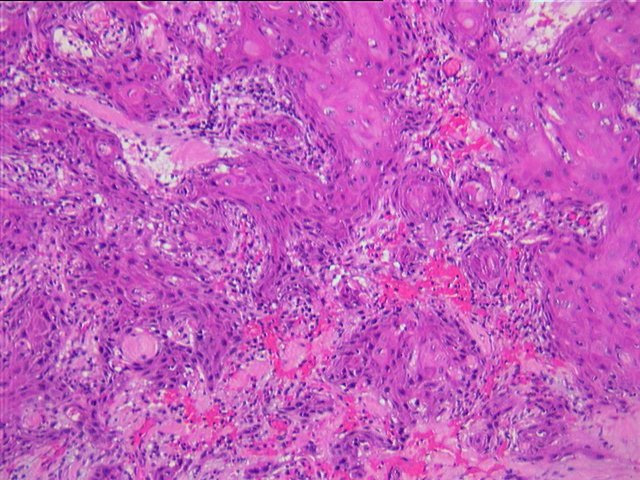
A 60-year-old female patient from India reported with a complaint of increasing difficulty of mouth opening and mastication for the previous 3 yrs. The patient had a habit of chewing betel nuts four times a day for 7 to 9 years. She would keep the betel nut in the mouth, against the cheeks for approximately 30min each time, chew, and finally spit it out. The patient stopped this habit completely after she was informed to stop. No medical history of any systemic diseases like hypertension, Diabetes mellitus, asthma etc. Socioeconomic status of patient was poor. After histopathologically confirming [Table/Fig-1] the diagnosis of OSMF, we planned this patient for surgical intervention. Complete pre-anaesthetic evaluation was done. Informed consent was procured. Initial interincisal mouth opening recorded was 2mm [Table/Fig-2]. Under aseptic precautions, a fibreoptic bronchoscope was used for intubation of the patient for administration of general anaesthesia. Bilateral fibrotomy and coronoidectomy was carried out. The maxillary and mandibular third molars were extracted to prevent the injury to healing flaps in the immediate postoperative phase. In most of cases third molar are buccal erupted, there was no need to extract second and first molars, and reconstruction of buccal defects is done with bilateral nasolabial flaps. The extra oral defect was closed primarily in layers. Temporomandibular joint trainer was placed in the oral cavity for 7 day postoperatively to prevent occlusal trauma induced dehiscence of the flaps. The oral physiotherapy was started after 48h with the help of ice cream sticks for 10 days followed by a Histers jaw exerciser to prevent contracture and relapse. The patient was instructed and motivated to do physiotherapy herself for up to 6 months and advised for regular follow up to observe the progress and note any changes in oral cavity. Immediate postoperative mouth opening was 38mm. But this patient could not follow the recommended mouth opening exercise schedule and lost to follow-up. After 3 month she came with complaint of growth in right buccal mucosa [Table/Fig-3] with reduced mouth opening which was 8mm and on histopathology examination revealed to be well differentiated squamous cell carcinoma [Table/Fig-4].
Histopathology slide of oral submucous fibrosis.

Pre operative mouth opening which was 2 mm.

Malignant conversion showing the lesion in right buccal mucosa region after 3 months.

Histopathology slide of well differentiated squamous cell carcinoma
Discussion
OSMF is an insidious chronic disease affecting any part of the oral cavity and sometimes the pharynx. Although, occasionally preceded by and or associated with vesicle formation, it is always associated with juxtra-epithelial inflammatory reaction followed by a fibroelastic change of the lamina propria, with epithelial atrophy leading to stiffness of the oral mucosa, causing trismus and inability to eat [1]. OSMF has a high rate of morbidity because it causes progressive inability to open the mouth, resulting in inability to eat and consequent nutritional deficiencies [2]. Mortality rate is significant because of high probability of malignant transformation into oral cancer, particularly squamous cell carcinoma at a rate of 7-30 % [2]. It is poorly understood unsatisfactorily treated disease.
Management includes cessation of habit and surgical release of fibrous bands followed by forceful opening of the mouth by fibrotomy and coverage of surgical defects with nasolabial flap and postoperative active jaw physiotherapy for atleast 6 month [3]. Other management modalities include buccal pad fat flap, Tongue flap, Palatal flap, Radial forearm flap used to reconstruct the defects created after fibrotomy. Surgery may induce scar tissue which reduces mouth opening due to scar contraction in mouth closing muscles [4]. Relapse is a common complication that occurs after surgical release of the oral trismus caused by OSMF. A variety of jaw opening devices have been used to treat trismus. The patient’s cooperation is the primary requirement for success in the treatment of OSMF.
Nasolabial technique flap has versatility and a distinct edge in maintaining the mouth opening. Exercises are frequently proposed to prevent or treat trismus, including active range of motion exercises combined with passive range of motion exercises. However a more serious complication of this disease is the risk of development of oral squamous cell carcinoma in one-third of OSMF patients [5]. In patients with oral submucous fibrosis, the oral epithelium becomes atrophic and thereby becomes more vulnerable to carcinogens [6,7]. Recently, the carcinogenicity of areca nut without tobacco was identified [8].
We did surgical intervention not only to relieve the trismus with long term results but also to facilitate oral examination for early detection [9] and management of malignant transformation. But because of lack of patient co-operation and inadequate follow up we failed to achieve our goals. OSMF is a potentially malignant disease predominantly. Only surgical treatment is not sufficient. Long terms follow-up and patient co-operation are equally important in the management of OSMF.
Conclusion
Only surgical intervention is not sufficient in the management of OSMF. Regular follow-up and frequent biopsies play an important role to check any malignant conversion even after the surgery.
[1]. Pillai R, Balaram P, Pathogenesis of oral submucous fibrosis: relationship to risk factors associated with oral cancerCancer 1992 69:2011-20. [Google Scholar]
[2]. Shevale VV, Kalra RD, Management of Oral Sub-Mucous Fibrosis: A ReviewIndian Journal of Dental Sciences 2012 4(2):107-14. [Google Scholar]
[3]. Borle RM, Nimonkar PV, Extended nasolabial flaps in the management of oral submucous fibrosisBritish Journal of Oral and Maxillofacial Surgery 2009 47:382-85. [Google Scholar]
[4]. Dijkstra PU, Exercise therapy for trismus in head and neck cancerOral Oncology 2007 43:389-94. [Google Scholar]
[5]. Hazarey VK, Erlewad M, Mundhe KA, Ughade SN, Oral submucous fibrosis: study of 1000 cases from central IndiaJ Oral Pathol Med 2007 36:12-7. [Google Scholar]
[6]. Pundir S, Saxena S, Aggrawal P, Oral submucous fibrosis a disease with malignant potential - Report of two CasesJ Clin Exp Dent 2010 2(4):e215-18. [Google Scholar]
[7]. Auluck A, Rosin MP, Zhang L, Sumanth KN, Oral Submucous Fibrosis, a Clinically Benign but Potentially Malignant Disease: Report of 3 Cases and Review of the LiteratureJCDA 2008 74(8):735-40. [Google Scholar]
[8]. Tilakaratne WM, Klinikowski MF, Saku T, Peters TJ, Warnakulasuriya S, Oral submucous fibrosis: review on aetiology and pathogenesisOral Oncol 2006 42(6):561-68. [Google Scholar]
[9]. Naphade MV, Dessertation on major immunoglobulin status and lactate dehydrogenase isozyme profile in oral pre-malignancy and malignancy 1993Nagpur. IndiaGovt. Dental College & Hospital [Google Scholar]