Case Report
A 32-year-old male patient was referred to the dental clinic by neurophysician for oral examination and treatment needs. Patient’s complains were halitosis, loss of teeth since 2 y due to caries and poor periodontal status. Patient had difficulty in mastication due to absence of complete set of dentition, hence wanted to replace the missing teeth. Patient gives history of smoking 5-7 cigarettes per day since 8 year. Medical examination revealed history of epilepsy since 5 year and hypertension since 7 year for which the patient was under medication. BP recorded was 140/90mmHg, which was slightly elevated prior to dental examination. Family history reveals no consanguineous marriage of his parents. His father gives history of hypertension, thyroid disease and psychiatric illness. Mother was healthy and normal. The younger sibling of the patient was normal.
General physical examination revealed short stature, round face, short neck, sparse hair on scalp, low set ears, depressed nasal bridge, widely separated inter acanthus distance [Table/Fig-1], bulky lower lip with serrations present on its surface. Patient was obese with Body Mass Index (BMI) calculated as 36.7 for a height of 5 feet weighing 188 pounds.
Face showing dysmorphic facial features like round face, short neck and flat nasal bridge

The other prominent feature presented in the case was evident brachydactyly of right ring finger with bulky broad nail bed [Table/Fig-2]. Patient also showed positive chvostek sign.
Picture showing brachydactyly of fourth digit

Intra-oral examination reveals anterior hypoplastic teeth [Table/Fig-3] with missing permanent mandibular right 2nd premolar, 2nd and 3rd molars with no history of extraction in the past, and teeth present are mal-aligned, high arched palate with angles class I malocclusion with deep bite. Deep caries in relation to permanent mandibular right 2nd premolar and 1st molar. Xerostomia and generalized gingival inflammation was seen.
Figure shows anterior hypoplastic teeth and serrated lower lip

Laboratory investigation revealed Serum Calcium=5.6 mg% (Normal: 9-11 mg%), Serum Phosphate level=5.0 mg/dl (Normal: 2.4-5mg/dl)and PTH=67.1 pg/ml (15-72pg/ml) Vit D=40ng/ml(30-74ng/ml). Thyroid function test resulted normal functioning of thyroid gland with, T4=11.55(5.1-14ug/dl), T3=129ng/dl (50-200ng/dl) and TSH=1.88(0.27-4.2 mIU/L). Alkaline phosphatase: 200U/L (Normal: 50-160U/L)
OPG reveals hypoplastic anterior teeth, impacted 3rd molars, horizontally impacted left mandibular 2nd premolar and most of the teeth show loss of lamina dura with associated root resorption. Pulpal calcification is evident in left mandibular impacted 3rd molar tooth [Table/Fig-4].
OPG reveals impacted third molars and left second molar,pulpal calcification in relation to impacted left mandibular 3rd molar

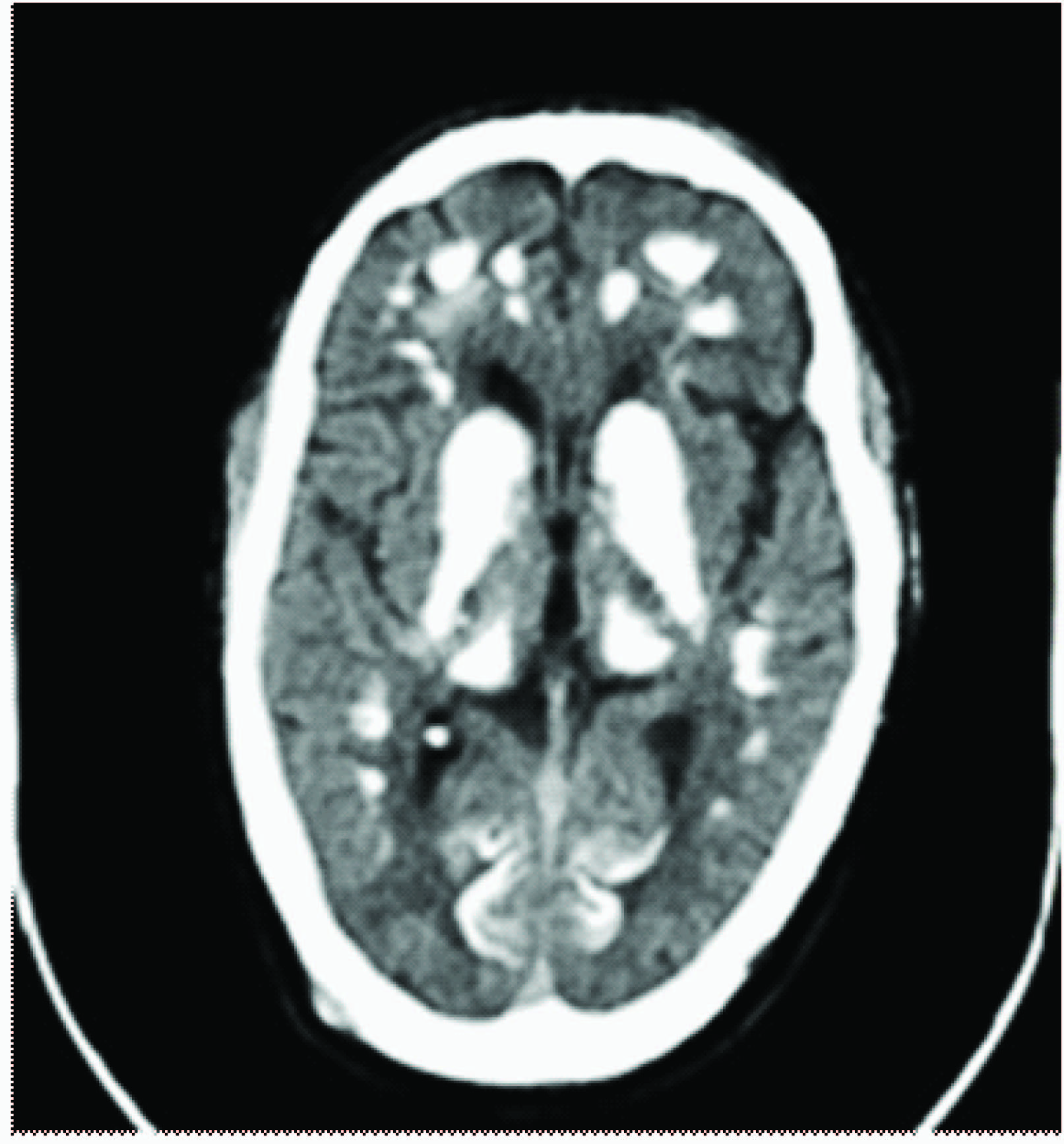
Computed tomography reveals calcification involving basal ganglia, periventricular region and cerebellar hemispheres [Table/Fig-5].
CT showing extensive bilateral symmetrical calcifications in the basal ganglia, thalamus and cerebellum
Neurophysicians had diagnosed the case with epilepsy and hypertension and had kept him under medication for the same. Before further investigations were carried out, we were approached to restore his oro-functional habits. Detailed history and examination revealed us in identifying the key features which includes history of seizures, short stature, obesity, brachydactyly of 4th digit and positive chvostek sign. Initial hematological examination reported showed decreased serum calcium levels. Depending on the history and initial blood investigation a provisional diagnosis of PHP and AHO was given. To rule out PHP, parathormone and thyroid function test were carried out. Parathormone level was within the normal range and thyroid function test which includes T3, T4 and TSH also were within the normal range. Computed tomography showed basal ganglia calcification and calcification of periventricular region and cerebellar hemispheres. Hence, a final diagnosis of AHO was established and treatment was planned accordingly.
Treatment plan included medication with Phenobarbitone 60mg orally once daily, 3gms of Calcium supplements orally, 60mcg vitamin D3 daily was started as initial phase of treatment. Patient was recalled after three weeks wherein hematological investigations were carried out. There was a considerable increase in serum calcium level to 7.8mg%, serum phosphate recorded was 3.7mg% which was reduced compared to initial values and PTH levels were 32.5pg/ml which showed considerable reduction from the aforementioned values.
Dental treatment plan included oral prophylaxis, removable partial denture to replace the missing teeth and restoration of decayed teeth in relation to permanent mandibular right 2nd premolar and 1st molar. Fixed partial denture was avoided in the present case due to history of epilepsy which could be the cause of frequent fracture of the replaced tooth. Patient is on regular follow up.
Discussion
Parathormone is the principal hormone that maintains serum calcium and phosphorous levels in the body. Parathormone functions mainly includes, enhanced distal tubular resorption of calcium, promotion of bone resorption, increased synthesis of 1,25 hydroxy vitamin D, therefore, leading to enhanced intestinal calcium absorption [1–4].
AHO is a hereditary metabolic disorder usually presented with constellation of characteristic physical features like obese build, short stature and brachydactyly. AHO when associated with end organ resistance to hormones like parathormone, gonadotrophins and Thyroid Stimulating Hormone (TSH), is called Pseudohypoparathyroidism (PHP) [1–5].
Genetic studies done to know the aetiology of AHO has revealed mutation of GNAS1 gene located on 20q13-11 as the culprit gene [2].
In literature, AHO has been reported with characteristic features like short stature, round face, flat, wide and low nasal bridge, obesity, short neck, flat occiput, mental retardation, brachydactyly of 4th and 5th digits, knuckle dimples in the clenched fists, short broad nails, osteoporosis, cataract, dementia, epileptic seizures, ankylosis of TMJ, rheumatoid arthritis of hand and foot joints, cone shaped epiphysis, thickened calvaria, basal ganglia calcification and subcutaneous ossification [3,4,6,7].
The present case does not give a familial history of AHO which is in agreement to studies done by Monica Gomes et al., but is contrary to series of erratic cases reported in literature [3,8].
Cases documented previously show preponderance of AHO in female individuals, stating that AHO occurs twice frequently in females than males. But the present case contradicts and presents itself in a male patient. In accord with female preponderance are studies done by Davies and Hughes, Fitch N et al., Sunder and Singh, and Esel Ertugrul et al., [5,6,9,10].
The characteristics typical of AHO piled in literature are round faces, short stature, brachydactyly of 4th and 5th digit, hypocalcemia and mental deficiency, also described in the present case, in concurrence with string of reports on AHO by Monica Gomes et al., Esel Ertugrul et al., kottler ML et al., Ambika L & Vaishali K, Wilson L & Richard and Seema Kapoor et al., [3,4,6–8,11].
TMJ ankylosis has been reported in case reports by Ambika L & Vaishali K and Goldberg et al., but the presenting case shows no ankylosis of TMJ [3,12].
Basal ganglia calcification seen in Computed Tomography (CT) has also been reported by Ambika L & Vaishali K, Wilson L & Richard and Seema Kapoor et al., and Livia et al., [2–4,11]. The reason for the focal accumulation of calcium in basal ganglia can be due to local factors and disturbance of calcium metabolism. Dementia, siezures and Parkinsonism are seen associated with basal ganglia calcification [6,13].
Oral manifestations in AHO patients include aplasia, thin enamel with enlarged pulp chamber, hypoplasia, hypodontia, pulp calcification, multiple carious teeth, multiple unerupted teeth, crowded anterior teeth, anterior open bite, gingival hyperplasia, gingivitis with spontaneous bleeding and pain [3,4].
Conclusion
Albright hereditary osteodystrophy is a longstanding disorder which needs careful examination and symptomatic treatment. As dentist, careful examination of physical characteristics and thorough evaluation of tooth eruption in accordance with chronological age of the patient can help in early diagnosis of patients with AHO. Careful correlation of other dental anomalies, enamel hypoplasia, blunted roots, mal-aligned teeth, malformed tooth can also aid in diagnosis. Multidisciplinary approach can help in accurate diagnosis and on providing prompt treatment to the patient.
[1]. Prentice R, Pseudohypoparathyroidism: a case reportThe Journal of Clinical Endocrinology & Metabolism 1954 14(9):1069-73. [Google Scholar]
[2]. Garavelli L, Pedori S, Zanacca C, Caselli G, Loiodice A, Mantovani G, Albright’s hereditary osteodystrophy (pseudohypoparathyroidism type Ia): clinical case with a novel mutation of GNASActa Biomed 2005 76(1):45-48. [Google Scholar]
[3]. Keluskar LA, Albright V, Herediatary Osteodystrophy: A constellation of Clinical FeaturesJournal of Indian Academy Of Oral medicine & Radiology 2010 22(4):215-17. [Google Scholar]
[4]. Kapoor S, Gogia S, Paul R, Banerjee S, Albright’s hereditary osteodystrophyThe Indian Journal of Pediatrics 2006 73(2):153-56. [Google Scholar]
[5]. Sunder R, Singh M, Pseudohypoparathyroidism: a series of three cases and an unusual presentation of ocular tetanyAnaesthesia 2006 61(4):394-98. [Google Scholar]
[6]. Ecsel E, Dűndar M, Bayram F, Catakouglu Candemir Z, Kilicc C, Albright’s Hereditary Osteodystrophy and Dementia: A Case ReportBull Clin Psychopharmacol 2001 11:183-86. [Google Scholar]
[7]. Kotter M, Linglart A, Carel J, Albright hereditary osteodystrophyOrphanet Encyclopedia 2004 [Google Scholar]
[8]. Gomes M, Camargo A, Sampaio T, Graziozi M, Armond M, Oral manifestations of Albright hereditary osteodystrophy: a case reportRevista do Hospital das Cl'inicas 2002 57(4):161-66. [Google Scholar]
[9]. Davies S, Hughes H, Imprinting in Albright's hereditary osteodystrophyJournal of medical genetics 1993 30(2):101-03. [Google Scholar]
[10]. Fitch N, Opitz J, Herrmann J, Albright's hereditary osteodystrophy: a reviewAmerican journal of medical genetics 1982 11(1):11-29. [Google Scholar]
[11]. Wilson L, Trembath R, Albright's hereditary osteodystrophyJournal of medical genetics 1994 31(10):779-84. [Google Scholar]
[12]. Goldberg MH, Slaughter TW, Harrigan WF, Pseudohypoparathyroidism with temporo-mandibular ankylosis: report of caseJ Oral Surg 1967 25(2):175-81.PubMed PMID: 5226355 [Google Scholar]
[13]. Evans B, Donley D, Pseudohypoparathyroidism, parkinsonism syndrome, with no basal ganglia calcificationJournal of Neurology, Neurosurgery\& Psychiatry 1988 51(5):709-13. [Google Scholar]