Since the discovery of x-rays by roentgen, the dental radiography has evolved at par with the medical radiology into a valuable asset to diagnosis. With the introduction of digital imaging and the advanced tomography, the diagnoses of oro-facial pathologies are possible with millimetre resolution. At routine clinical use, the intraoral radiographic techniques:, the bisecting angle technique and the paralleling angle techniques are the best option, since it does not require much radiographic exposure and the patient can afford it at a low cost.
However, the drawback of the above said techniques are that it is not feasible to place the film/sensor intraorally in cases of patients with developmental disability, exaggerated gag reflex, paediatric patients, dental phobia, trauma, trismus and neurological deficits [1–3]. Moreover, the above said problem is compounded by the fact that, the oral cavity encases a complex anatomical architecture and the added bulk of sensor in digital radiography makes it more difficult for certain patient populations to accept intraoralfilms/sensors and film holder placement [4,5]. Considering this, Newman and Friedman in the year 2003 proposed the placement of film/sensor extra-orally while directing the x-ray beam at a prescribed angulation [6]. Chia-hui chen in the year 2003 further enhanced this approach by using an extraoral aiming device to avoid partial image (cone-cut) [7]. Saberi et al., suggested a 100 tilt of the head away from the mid-sagittal plane towards the side being imaged [8]. Since then, the extra-oral approach has been used as a supplementary aid in dental radiography, however, its clinical usage has not been validated yet. Thus the aim of the present study was to evaluate the utility of the extra oral aiming device in imaging the periapical regions of the posterior teeth.
Materials and Methods
Twenty volunteer patients of both gender in the 10-35 y age group reported as outpatient to Department of Oral Medicine & Radiology, St. Joseph dental college & hospital, Eluru, India were randomly recruited. The Ethical Review Committee of the Institution approved the study, while written consent was given by the patients/guardian.
The selected samples were further subdivided into four groups according to the area to be imaged, with five patients in each group as follows:
Group A- Maxillary premolars
Group B- Maxillary molars
Group C- Mandibular premolars
Group D- Mandibular molars
From all the selected samples, both extraoral and intraoral (both soft tissue and hard tissue) examination was carried out, past medical and dental histories were recorded. Patients who volunteered and with clinically visible premolar/molar crowns were included for the study. Patients with missing teeth premolars/ molars or with any neuromuscular disorder that hamper the holding of the aiming device were excluded from the study.
Armamentarium
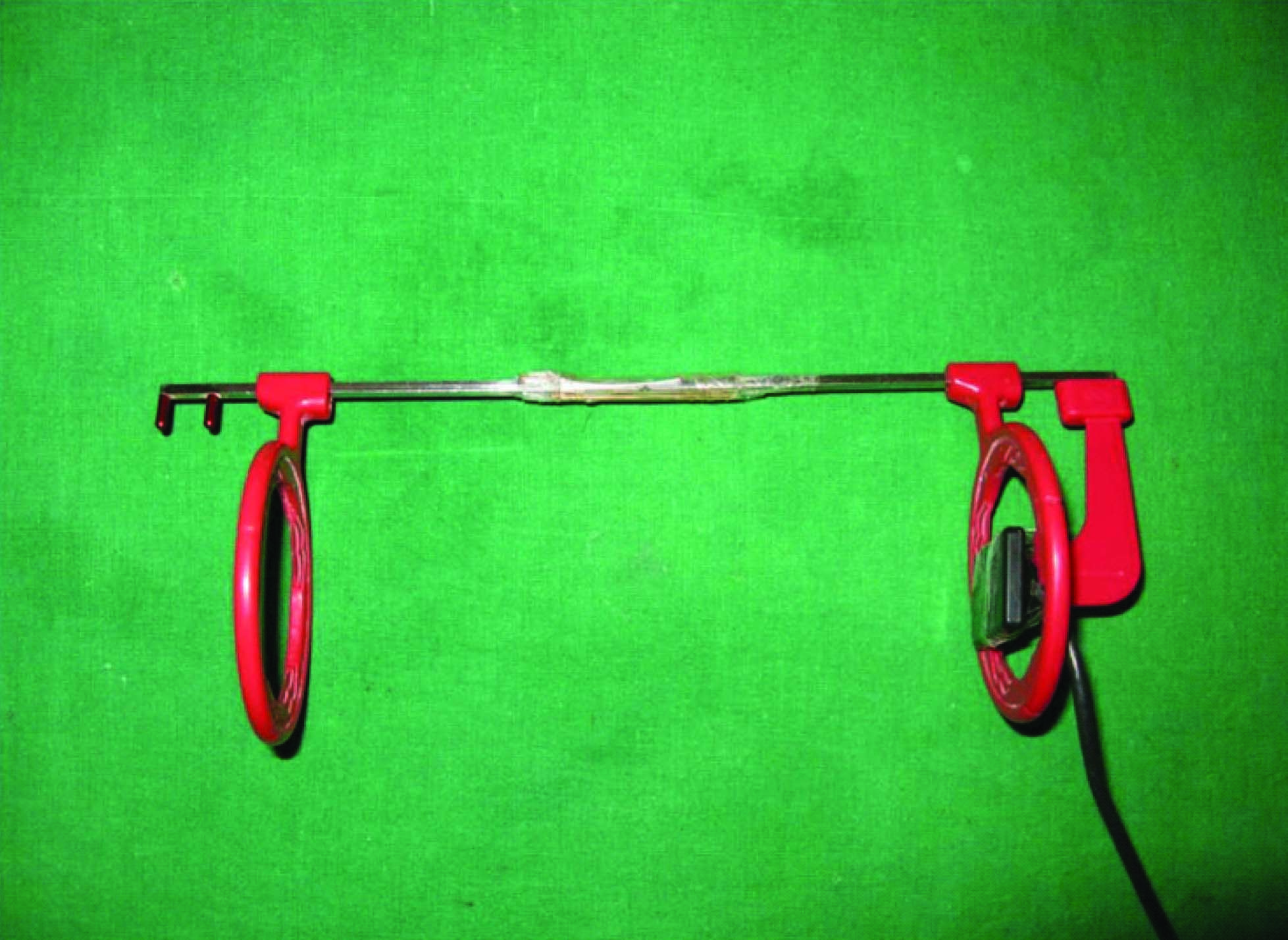
Bite-wing radiography locator rings (Dentsply, York, PA) - 2
Bite-wing radiography straight metal supporting indicator rods- 2
Horizontal bite-wing radiography bite block – 1
Rubber tube of approximately 2 cm in length- 1
Size no.2 sensor- 1
Assembly of the aiming device: The aiming device is assembled as suggested by Chia-hui chen in the following manner: [7]. The two straight supporting metal indicator rods are inserted into two locator rings (one at each end). At one end of the indicator rods, the bite block is attached and the film/sensor is placed firmly into the slot of the bite block. Note that the exposing surface of the sensor must be oriented in the direction of the x-ray cone. Finally, the two indicator rods (with one locator ring each) are connected together using the rubber tube [Table/Fig-1]. The distance between the two locator rings can be adjusted using the linking tube to take into account the facial width of the patient. As per the facial width of the patient, the distance between the two locator rings can be altered by adjusting the ends of the metal indicator rods placed within the linking rubber tube.
Technique
As stated earlier the methodology employed in this study is modified form of extra oral radiographic techniques available in the literature to image the intraoral periapical regions of the posterior teeth [6–8]. The procedure is carried out in the following manner:
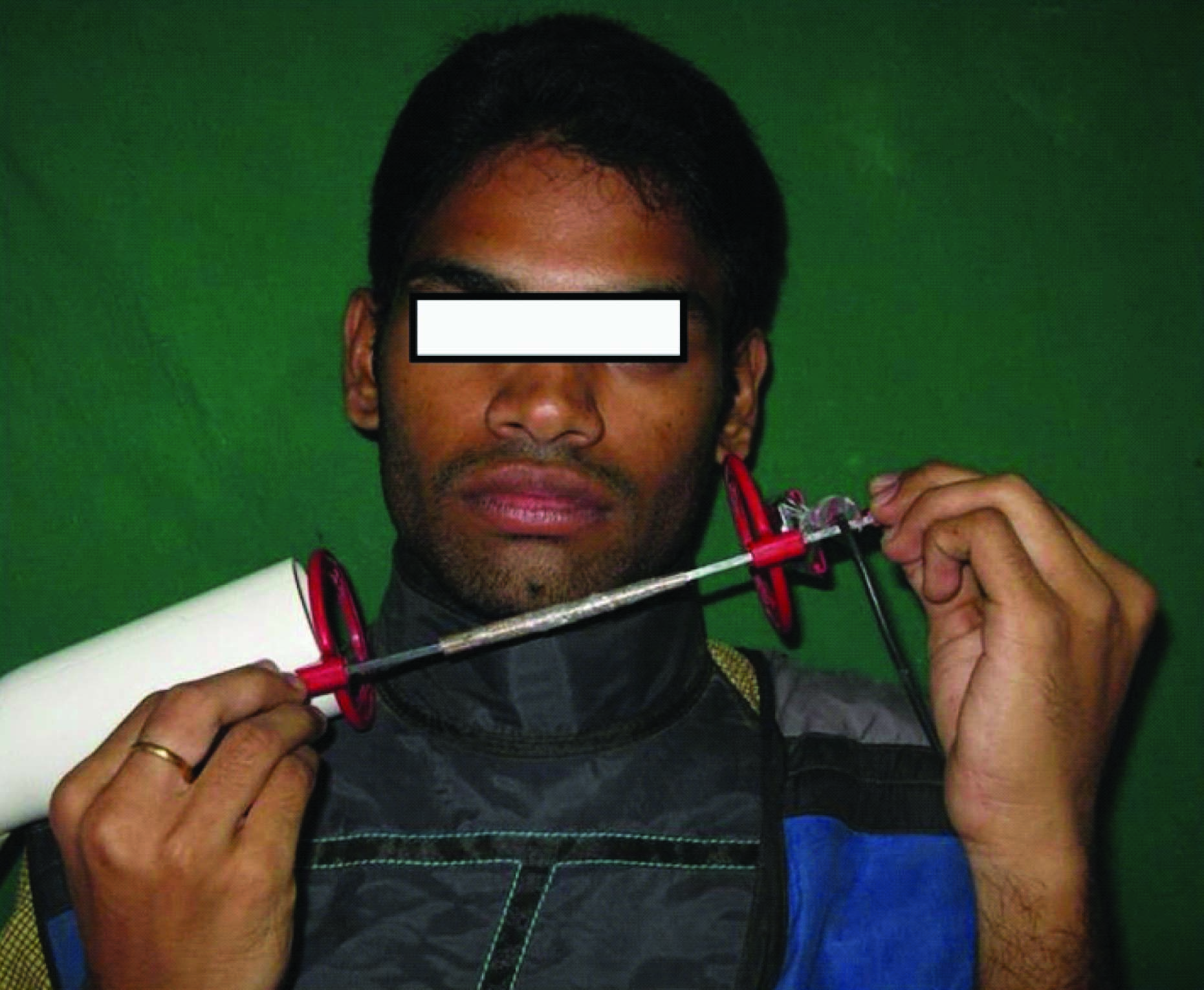
For Maxilla [Table/Fig-2].
[Table/Fig-2]
Patient position for maxillary molar exposure

Step 1: The patient was made to sit upright with Frankfort plane [this plan extends from the upper border of the external auditory canal (anteriorly) to the upper border of the lower orbital rim] horizontal with the floor.
Step 2: The aiming device was placed on the external surface of the cheek, directly buccal to the side of the target tooth to be imaged and the patients were instructed to hold the device firmly with their hand.
Step 3: The patients were instructed to open their mouth wide so that the X-ray beam pass through the aiming device to the sensor unobstructed from the opposite side and to avoid superimposition of the contralateral tissues.
Step 4: The patients head was rotated 100 toward the side being imaged.
Step 5: The Position indicating device (PID) was angled vertically at -200 to -250.
Step 6: The exposure was made.
For Mandible [Table/Fig-3].
[Table/Fig-3]
Patient position for mandibular molar exposure
Repeat steps 1&2 as for maxilla, stated above
Step 3: The patient’s chin was raised, which allows the X-ray beam to pass to the sensor through the aiming device unobstructed, thus avoiding superimposition of the contralateral tissues on the image.
Step 4: The head was tilted approximately 100 towards the side being imaged.
Step 5: The PID was angled approximately vertically at -150 to -200.
Step 6: The exposure was made.
All images were obtained by using sopix imaging RVG system (Satelac Pvt. Ltd INDIA) and intraoral sensors (37 x 24 mm). An Intra Os 70 (Blue X imaging system) DC X-ray source (Assago, Italy) was used at 70 kVP, 7 mA, 0.5 seconds for exposure of mandibular teeth and 1.0 sec for maxillary teeth. After exposure, the radiographs were labelled and stored for interpretation [Table/Fig-4,5,6,7].
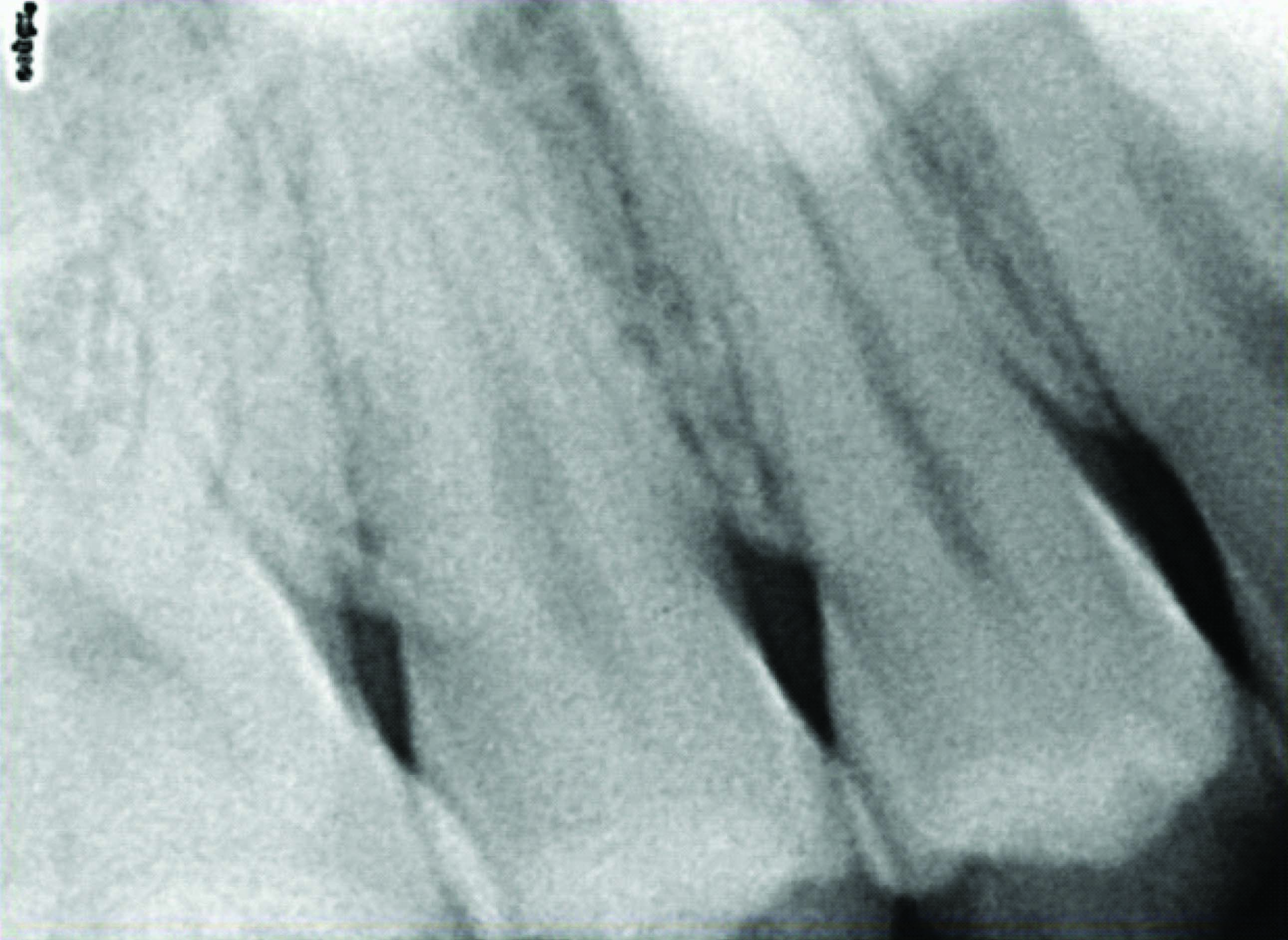
Radiograph of maxillary second premolar region (25)
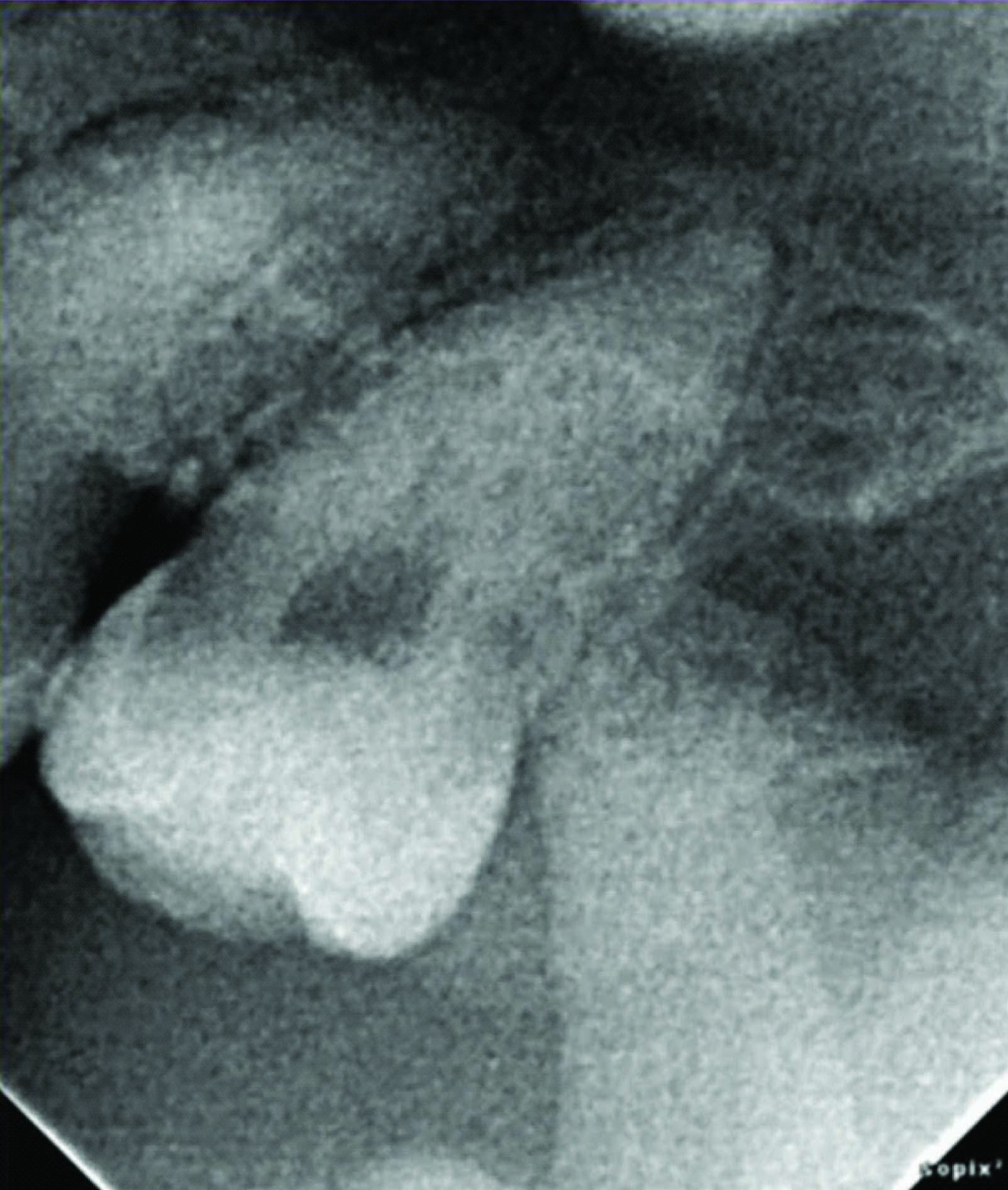
Radiograph of maxillary third molar (28)
Radiograph of mandibular second premolar (36).,

Radiograph of mandibular third molar (48)
The radiographs were evaluated for the complete coverage and visualization of the anatomical structure imaged and this is measured in terms of percentage by a digital grid, a component of radiovisiography software. To evaluate the above said measurement, each radiographic image was drawn into the imaging window of the personal computer and the digital scale option was clicked which places a grid containing 100 equal square boxes [Table/Fig-8]. Then the overall equal magnification of the image was done and interpreted for crown-root and periapical regions. All the findings recorded were entered in a Microsoft excel spread sheet and subjected for statistical analysis. ANOVA (Analysis of variance) test was employed to differentiate the significance, if any among the groups.
Radiographic image with grid placed for measurement

Results
Among the 20 selected samples 13 (65%) were adults and 7 (35%) were children [Table/Fig-9]. Accurate coverage of the imaging area for the child patients ranged from 65-100% and for the adult patients it ranged from 75-95%. There was no much difference in the overall accuracy among children (88%) and adult (92.3%) patients.
Demographic data., * Not significant
| Area imaged | S. No. of radiographs | Type of patient | Percentage of diagnosable image | Reason for non-diagnosable image | Over-all percentage of accuracy | Statistical Findings |
|---|
| Maxillary premolars | 1A | Adult | 80 | Overlapping of the opposite arch | 84 | f-value- 2.152 p-value- 0.134* |
| 2A | Child | 90 | Overlapping of the opposite arch |
| 3A | Adult | 90 | Improper alignment of the sensor- device |
| 4A | Adult | 95 | Inadequate coverage of the sensor |
| 5A | Child | 65 | Patient movement |
| Maxillary molars | 1B | Adult | 100 | ---------------- | 89 |
| 2B | Child | 85 | Overlapping of the opposite arch |
| 3B | Adult | 95 | Horizontal overlapping |
| 4B | Child | 90 | Overlapping of the opposite arch |
| 5B | Adult | 75 | Improper alignment of the sensor- device |
| Mandibular premolars | 1C | Child | 95 | Inadequate coverage of the sensor | 93 |
| 2C | Adult | 95 | Horizontal overlapping |
| 3C | Adult | 90 | Overlapping of the opposite arch |
| 4C | Adult | 85 | Overlapping of the opposite arch |
| 5C | Adult | 100 | ------------- |
| Mandibular molars | 1D | Adult | 100 | -------------- | 97 |
| 2D | Child | 100 | -------------- |
| 3D | Child | 90 | Improper alignment of the sensor- device |
| 4D | Adult | 95 | Inadequate coverage of the sensor |
| 5D | Adult | 100 | ------------- |
The area intended to image was covered more in mandible (95%) than in maxilla (86.5%). Among the mandibular tooth, the molars were better imaged (97%) than the premolars (93%). Similarly the maxillary molars were imaged better (89%) than the maxillary premolars (83%) [Table/Fig-9].
The overall accuracy was 90.75%. Among the reason for reduced accuracy include overlapping of the opposite arch teeth (4%), improper alignment of the sensor-teeth being imaged (2.25%), inadequate coverage of the sensor (0.75%), horizontal overlapping of teeth (0.5%) and patient movement (1.75%) [Table/Fig-9].
Discussion
Dental radiographic technique can be classified as intra-oral or extra-oral based on the location of the placement of the film/sensor. The intraoral techniques include imaging of teeth in a particular arch in its superior-inferior dimension or imaging of the occlusal surface of the teeth (occlusal radiography) in the arch in partial or as a whole [4].
The intra oral film placement allows the imaging surface to be in close contact with the image receptor (film/sensor); this allows the image receptor to be smaller in size and has an added advantage of reduced exposure to the patient. However, sometimes the intraoral film placement can be difficult in many patients due to various reasons [9,10]. As some patients cannot tolerate the image receptor/film holders or both due to compromised anatomy such as shallow/narrow arches or reduced vestibular depth, third molar regions. At times pathologies, trauma and trismus can also hinder the placement of the image receptor. Above all, it is difficult to place intraoral film/sensor in certain patient populations such as paediatric patients, those with exaggerated gag reflex, patient with dental phobia and neurological deficits [1–3].
As early as in 1974, Fisher proposed an extraoral radiographic technique (extraoral film placement) for obtaining the images of third molars using occlusal film [2]. Fischer technique holds good for imaging third molars alone but the remaining posterior teeth are not imaged with this technique.
Later Newman and his colleagues in the year 2003 proposed the placement of film/sensor extra-orally (instead of conventional intraoral placement) to radiograph both maxillary and mandibular posterior teeth [6]. According to Newman and Friedman for imaging maxillary teeth, with the patient sitting upright, the sensor is placed on the external surface of the cheek, directly buccal to tooth to be imaged. A cotton roll can be placed between the sensor and the cheek to parallel the sensor with the buccal surface of the tooth to allow the X-ray beam to pass to the sensor unobstructed from the opposite side. To avoid superimposition of the contralateral tissues, the patient mouth is open as wide as possible and the X-ray cone is angled approximately -550. Additionally, the X-ray cone must be aligned perpendicular to the sensor to provide an accurate image [6]. Similarly, for imaging mandibular teeth, with the patient sitting upright and the chin raised, the sensor is placed on the external surface of the cheek and the X-ray cone is angled at approximately -350 [6].
The drawback of the Newman and Friedman technique is that, the x-ray entry points and exact location of receptor based on anatomic landmarks have not been specified for each tooth. Moreover, there is a chance of cone cut artifact of the resultant images, attributed to incorrect positioning of the x-ray cone/ sensor alignment. This is due to the long distance between the film/sensor and the x-ray cone, causing difficulty in aiming the x-ray cone towards the film/sensor [8]. The other demerits of this technique includes technique sensitivity and lower image resolution [11].
Chen et al., further enhanced this approach by designing an extraoral aiming device. The advantage of the aiming device is that the x-ray beam can be aimed directly at the sensor under the guidance of the locator ring. Moreover, the aiming device is inexpensive and can be easily assembled with all the components readily available in most dental clinics. Chen et al., also suggested a lesser vertical angulation of the x-ray beam (i.e.,-200 to -300 for maxillary teeth and – 100 to -150 for mandibular teeth) when compared with Newman and Friedman. Chen et al., attributed these changes to the difference in facial height among Taiwanese and whites [7].
Saberi et al., tested the angulations prescribed by Chen et al., in phantom head models. The authors observed that an angulation of approximately -250 for maxillary teeth and -200 for mandibular with a head tilt of approximately 100 from the midsagittal plane towards the side being imaged (similar to lateral oblique technique) were found to be effective in imaging the teeth of interest [8].
Considering the above literature, the present study was conducted to evaluate the utility of extra-oral aiming device and the methodology developed by Chia-hui chen with an addition of 100 head tilt as advised by Saberi et al., to image the posterior teeth along with its periapical regions. The rationale behind adopting chai-hui chen and saberi et al methodology in this study followed a pilot trail done prior to the original study. The pilot trail showed neither Chai-hui chen nor saberi et al., technique when used alone could not image the teeth of interest completely, whereas the combination of Chia- hui chen extraoral device with saberi et al., angulation showed positive outcome. To our knowledge this is the first original research work, previous studies available in the literature were case based studies [3,10,12].
From the present study, it is arguable that this approach is an efficient technique for achieving diagnostic films in our selected population of patients. From our observation we found that all the subjects tolerated the procedure well especially paediatric, dental phobic and patients with gagging reflex and trismus. Moreover the technique is simple, reproducible, time saving and the chance of cross contamination is very minimal. The most important advantage is that this technique permits imaging of endodontic films and edentulous areas where placement of intraoral films is difficult [Table/Fig-10].
Comparative analysis of intraoral technique and extra oral approach
| Intraoral technique | Extraoral approach |
|---|
| Patient compliance | Questionable | Good |
| Paediatric patients | Not comfortable | Comfortable |
| Dental phobic patients | Not acceptable | Easily acceptable |
| Reproducibility | Possible | Possible |
| Dimensional accuracy | Accurate with parallelingtechnique | Questionable |
| Endodontics | Useful | Useful |
| Edentulous area | Difficult | Easy |
| Gagging | More chance | Nil |
| Trismus | Not the technique of choice | Ideal for mandibular projections |
| Cross contamination | Possible | Very minimal |
| Radiation exposure | Minimal | Comparatively higher |
The possible disadvantage of this technique is the dimensional inaccuracy of the resultant image. Another questionable aspect of this technique is the increase in the amount of radiation and a slight decrease in the resolution of the resultant image. The increase in amount of radiation is generally negated by the reduction in the number of unacceptable films taken intraorally. Moreover with the usage of sensor, a less KVp was used and the patient’s used protective barriers such as lead aprons. Another interesting observation is that with the usage of sensor and further with the digital enhancement, there was no gross reduction in the resolution of the image and all the images were easily available for interpretation.
With regard to its diagnostic utility, the radiographic images were evaluated for complete coverage and visualization of the crown-root and periapical areas of the teeth imaged. The accuracy of visibility of imaging area for the child patients ranged from 65-100% and for the adults it ranged from 75-95%. There was no much difference in the overall accuracy among children (88%) and adult (92.3%) patients [Table/Fig-9]. From our observation none of the patients encountered difficulty in handling the aiming device, especially paediatric patients showed great interest in holding the device.
The visibility of imaging area was more in mandible (95%) than in maxilla (86.5%). Among the mandibular teeth, the molars were better imaged (97%) than premolars (93%). Similarly the maxillary molars were imaged better (89%) than maxillary premolars (83%) [Table/Fig-9]. The reason for these negligible differences can be due to the complex anatomical architecture of maxilla and premolar region.
The overall accuracy was 90.75%. Among the reason for reduced accuracy include overlapping of the opposite arch teeth (4%), improper alignment of the sensor-teeth being imaged (2.25%), inadequate coverage of the sensor (0.75%), horizontal overlapping of teeth (0.5%) and patient movement (1.75%) [Table/Fig-9]. The above mentioned pitfalls were secondary to anatomical constraints, technical inexperience and patient factors.
Overlapping of the opposite arch teeth were more common and found mostly with the premolars than the molars, the reason behind it was obvious due to the fact that the premolars have comparatively longer roots thus requiring more angulation owing to overlap. Improper alignment of the sensor and horizontal overlapping of the teeth were also found and were secondary to technical errors which can be rectified with expertise. One interesting observation from the study is the inadequate coverage of the sensor with the teeth being imaged especially with the premolars, the reason can be attributed to two factors: one as stated earlier the roots of the premolar are comparatively longer and secondly, the relatively smaller rectangular size of the sensor which cannot accommodate it specially when the parallelism is not attained between the source (X-ray)-object (teeth) and receptor (sensor).In such instances placing the sensor with its long axis vertically will permit adequate coverage of the tooth; however, with a compromise of minimal coverage of adjacent teeth in its horizontal axis.
Conclusion
Extraoral approach to image objects within the jaws such as teeth are required in certain patient populations. The approach postulated by Newman and Friedman then enhanced by chen et al., and later by saberi et al., is undeniably a useful supplement aid to our clinical practice. This technique is not meant to replace the conventional intraoral radiographic technique; however it can be used irrefutably when situations demand. To our knowledge this is the first study done to validate the extraoral approach in imaging periapical regions of posterior teeth; hence no literature was available to compare the findings of the study. Further studies with larger sample size can be done to authenticate our findings.