Christ-Siemens-Touraine Syndrome: Case Report of 2 Brothers
Rita V Vora1, Gopikrishnan Anjaneyan2, Arvind Chaudhari3, Abhishek P Pilani4
1 Professor and HOD, Department of Skin and VD, PS Medical College and SKH, Karamsad, Anand, Gujarat, India.
2 Assistant Professor, Department of Skin and VD, Amrita Institute of Medical Sciences, Kochi, Kerla, India.
3 2rd year Resident, Department of Skin and VD, PS Medical College and SKH, Karamsad, Anand, Gujarat, India.
4 2nd Year Resident, Department of Skin and VD, PS Medical College and SKH, Karamsad, Anand, Gujarat, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rita V Vora, B/4 Om Villa, Rajababu Lane, Opp Big Bazar, 80 Feet Road, Anand, Gujarat-388001, India. Phone : 09879290417, E-mail : ritavv@charutarhealth.org
Ectodermal dysplasia is a rare disorder. Christ-Siemens-Touraine syndrome (Hypohidrotic Ectodermal dysplasia (HED)) is a diffuse, non-progressive disease present at birth and involves at least two tissues of ectodermal origin. It is caused by mutation in gene ectodysplasin (EDA, EDA1) located at Xq12-13. Main clinical feature of HED is sparse or absent eccrine gland as well as hypotrichosis, nail, and teeth abnormality with characteristic faces. The absence or diminished activity of sweat gland results in patients having more chances of developing hyperthermia and with intolerance to warm environment. Most do well with simple measures such as wet clothes, air conditioning, wet bands etc. We present cases of two brothers, born of non-consanguineous marriage, who presented to us with complaints of heat intolerance and abnormal facial features.
Dysplasia, Ectodermal, Hypohidrotic
Case Report
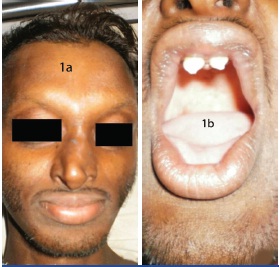
A 22-year-old male presented to the Medicine Department with fever, was referred to Skin Department for abnormal premature looking face and decreased sweating. Patient gave history of very minimal sweating since childhood associated with heat intolerance. He gave h/o hyperthermia at work. On examination frontal bossing, periorbital wrinkling of skin, saddle nose, sunken cheeks, thick lips & prominent chin was present [Table/Fig-1a]. Oral cavity revealed 4 conical teeth (2 incisors and 2 molar) with mild gum atrophy [Table/Fig-1b]. Anterior hairline was retracted with short, sparse and thin hair present over scalp, eyebrow, beard, axilla & pubis. Terminal hairs on trunk and limbs were absent. The skin was smooth & shiny all over with wrinkling at places. No nail abnormality seen. Palms & soles were normal with mild alteration in dermatoglyphic pattern. Salivation and lacrimation was normal. No Otorhinolaryngological or ophthalmic abnormality was detected. Routine investigations along with LFT, RFT was normal. LDH (382) & CPK (562) were raised. Chest X-ray showed bilateral pleural effusion probably responsible for his fever. CSF & pleural fluid study was normal.
(a)Patient with frontal bossing, periorbital wrinkling of skin, saddle nose, sunken cheeks, thick lips & prominent chin was present.(b) Patients picture showing Oral cavity with two conical peg shaped incisors
While evaluating family history, his 18-year-old brother also gave a typical history of heat intolerance at work and after eating hot food. He required lots of water to drink regularly & bathed 3-4 times daily. He had multiple febrile episodes in the past. O/E he had typical hypohidrotic dysplastic face with frontal and chin prominence with thick everted lips and saddle nose [Table/Fig-2a]. Oral cavity showed 4 teeth (2 conical incisors & 2 molar) with macroglossia [Table/Fig-2b,3a]. Hair was short, thin & sparse over scalp [Table/Fig-3b], eyebrow, beard, axilla & pubis. Terminal hairs on trunk and limbs were absent. Sweating was minimal with shiny hyper pigmented skin over body [Table/Fig-3c]. Palms, soles and nails were normal. Routine investigations were within normal limits. No Otorhinolaryngological, ophthalmic or medical problems were detected.
a Patients brother showing similar features (b) Patients brother with similar features

(a) Patients brothers picture showing macroglossia (b) Patients brothers picture showing retracted hair line with short sparse and thin hair over scalp (c) Patients brothers picture showing classical facies with smooth and shiny skin over trunk with absence of terminal hair

Both brothers were born of a non-consanguineous marriage and by normal delivery without any complications like oligohydramnios. Family history was not significant with none of their parents, grandparents or the three sisters showing any defects. Both brothers had normal social, physical, sexual and mental development.
Discussion
Ectodermal dysplasias are relatively rare and occur with a frequency varying between 1:10,000 and 1:100,000 live births [1]. Freire-Maia and Pinheiro [2] clinically classified Ectodermal Dysplasias into various subgroups according to defects like trichodysplasia, dental abnormalities, onychodysplasia and dyshidrosis using ‘1-2-3-4 system’.
The most common form of Ectodermal Dysplasias, Christ-Siemens-Touraine syndrome {MIM 305100}, commonly known as anhidrotic/hypohidrotic ectodermal dysplasia (HED), is an X-linked recessive disorder characterized by heat intolerance, absence of sweat glands and abnormal spiky or absent teeth.
It was first described in 1848 by Thurnam [3] and later in the 19th century by Darwin [4]. In 1913, Christ characterized it as a congenital ectodermal defect. In 1921, Siemens confirmed the X-linked nature of inheritance & in 1936, Touraine published on the wide range of features.
HED is inherited in an X-linked recessive, autosomal dominant or autosomal recessive manner. A 95% of randomly selected individuals with HED have the X-linked recessive inheritance. The remainder (5%) have either the autosomal recessive or autosomal dominant inheritance. It is fully expressed in males only. Heterozygotic females may be mildly affected.
It is caused by mutation in gene ectodysplasin (EDA, EDA1) located at Xq12-13 coding for transmenbrane protein, ectodysplasin A [5]. HED is a diffuse, non-progressive disease present at birth and involves at least two tissues of ectodermal origin. Genetic defects in ectodysplasin signal transduction pathways are the basis of this syndrome. Epithelial cells in hair follicles, eccrine sweat glands, and developing teeth use this pathway during morphogenesis. Therefore, genetic defects result in aplasia, hypoplasia, or dysplasia of these structures. They also lead to disturbances in the enamel matrix and tooth buds and subsequent hypodontia and hypoplasia of teeth [6].
Main clinical feature of HED is sparse or absent eccrine gland as well as hypotrichosis and oligodentia with peg-shaped teeth with incisor and/or canine teeth mainly affected which looks conical and pointed and sometimes is the only obvious abnormality. The absence or diminished activity of sweat gland results in patients having more chances of developing hyperthermia with minimal exertion. Affected infant may present with recurrent fever [7]. Our patient also had similar complains of recurrent high grade fever with intolerance to warm environment. Sparse and often light pigmented scalp hair, eyebrow, eyelashes with nail abnormality is common. HED patient have a characteristic faces with frontal bossing, a saddle nose, and full, everted lips. Abnormal mucus gland results in extreme nasal secretion leading to recurrent respiratory tract infections. Most infants have difficulties in feeding or episodes of severe illness associated with infections commonly pneumonia. This ill health adversely affects their growth and development. Most female carriers of HED are recognised by dental anomalies, and most of those whose teeth are normal may be recognised by their abnormal pattern of sweating [8].
Histologically, the epidermis is thin and flattened, the eccrine sweat gland are absent or rudimentary. The dermal connective tissue is grossly normal but elastic and collagen fibre may be sparse or fragmented. Mucous gland may be absent in respiratory tract [9].
The management of children and adults with HED is a challenge because of their heat intolerance and their susceptibility to pulmonary infections. Maintenance of cool ambient temperature is vital to prevent hyperpyrexia. Heat intolerance seems to decrease with age due to the development of some ability to sweat in adolescence and adaptation of changed lifestyle. DNA-based mutational analysis now offers the opportunity for prenatal diagnosis of this condition [10]. Most do well with simple measures such as wet clothes, air conditioning, wet bands etc. Dental restoration is of great psychological benefit and early implementation of dentures is very helpful. Early prosthetic therapy for children with ectodermal dysplasia provides a unique opportunity for cooperative effort between the pedodontist and the prosthodontist, as pedodontists are better trained in the psychological management of children. Prosthodontic treatment may commence at an early age of 3-4 y as it enhances conditions for growth and development of orofacial structures [11]. Future treatments may involve gene correction or administration of recombinant EDA protein. These two patients were counselled regarding the condition & referred to Dental, ENT departments and advised regarding the lifestyle changes including restriction of physical exertion, choice of occupation to ensure a disease free life. Dental prosthesis was offered and the brothers were advised regarding regular follow up and to be extra careful during febrile episodes. This case presentation of two brothers is done due to its rarity and the need for the physicians to diagnose such cases at the earliest. It is to be stressed that the counseling of the patients empowers them to get adjusted to the society and helps them live a better life by simple lifestyle modifications. Most of the times, a patient doesn’t yearn for cure but empathy and reassurance from the physician.
[1]. Vallejo AP, Monje ELA, Garcia MG, Fernandez MM, Buylla FBMA, Treatment with removable prosthesis in hypohidrotic ectodermal dysplasia: a clinical caseMed Oral Patol Oral Cir Bucal 2008 13:119-23. [Google Scholar]
[2]. Freire-Maia N, Pinheiro M, Ectodermal dysplasia: a clinical classification and a causal reviewAm J Med Genet 1994 53:153 [Google Scholar]
[3]. Thurnam J, Two cases in which the skin, hair and teeth were very imperfectly developedMed Chir Trans 1848 31:71-82. [Google Scholar]
[4]. Darwin C, The Variations of Animals and Plants Under Domestication 1857 22nd ednLondonJohn Murray:319 [Google Scholar]
[5]. Kere J, X-linked anhidrotic (hypohidrotic) ectodermal dysplasia is caused by a mutation in a novel transmembrane proteinNature Genet 1996 13:409 [Google Scholar]
[6]. Mokhtari Sepideh, Mokhtari Saeedeh, Lotfi Ali, Christ-Siemens-Touraine Syndrome: A Case Report and Review of the LiteratureCase Reports in Dentistry 2012 vol. 2012:3Article ID 586418 [Google Scholar]
[7]. Agrawal S, Gupta S, Hypohidrotic ectodermal dysplasiaIndian Dermatol Online J 2012 3:125-27. [Google Scholar]
[8]. Clarke A, Philips DI, Brown R, Clinical aspects of X-linked hypohydrotic ectodermal dysplasiaArch Dis Child 1987 62:989-96. [Google Scholar]
[9]. Mahajan V, Sharma N, Sood A, Ectodermal dysplasisas: Severe palmoplanter Hyperkeratosis And Chronic Angular CheilitisIndian J Dermatol 2003 48(4):223-28. [Google Scholar]
[10]. Zonana J, Schinzel A, Upadhyaya M, Prenatal diagnosis of X-linked hypohidrotic ectodermal dysplasia by linkage analysisAm J Med Genet 1990 35:132-35. [Google Scholar]
[11]. Kaul S, Reddy R, Prosthetic rehabilitation of an adolescent with hypohidrotic ectodermal dysplasia with partial anodontia: Case reportJ Indian Soc Pedod Prev Dent 2008 26:177-81. [Google Scholar]