Oral Cysticercosis: A Diagnostic Difficulty
Jaya Joshi1, Manjunatha Bhari Sharanesha2, Rameshwar Jatwa3, Shaleen Khetrapal4
1Associate Professor & Head, Department of Oral Pathology and Microbiology, Govt College of Dentistry, Indore, Madhya Pradesh, India.
2Professor, Department of Oral Pathology and Microbiology, K M Shah Dental College & Hospital, SumandeepVidyapeeth, Vadodara, India.
3Assistant Professor, Department of Molecular Medicine and Toxicology, Devi Ahilya Vishwa Vidyalaya, Indore, Madhya Pradesh, India.
4Assistant Professor, Department of Periodontology, Govt College of Dentistry, Indore, Madhya Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. BS Manjunatha, Professor, Department of Oral and Maxillofacial Pathology, K M Shah Dental College & Hospital, Sumandeep Vidyapeeth, Pipariya-391760, Vadodara, India. Phone : 91-02668-245266,
E-mail: drmanju26@hotmail.com
Cysticercosis is a rare disease caused by the ingestion of the parasite Cysticercus cellulosae, a larval stage of Taenia solium. The definitive host is human who harbors the adult worm and may accidentally or incidentally become the host. The larval form of cyst is commonly seen in the brain, meninges and eyes. Cases in the maxillofacial region including oral cavity and cheek muscles are rarely reported. Cysticercosis is not commonly considered in the diagnosis of swellings of the head and neck and a diagnostic and therapeutic dilemma for clinicians. Hence, they are of utmost interest to the practitioner and have to be studied. We present an unusual case of cysticercosis presenting as a solitary cystic nodule in the upper left vestibule of the oral cavity in an 18 year male and the diagnosis was made on histopathological examination.
Cysticercosis, Cysticercus Cellulosae, Larvae, Parasite, Taenia solium
Case Report
An 18-year-old male from Central India presented with an asymptomatic nodule in the right mucobuccal fold of upper arch. The patient reported that the lesion was present since 5-6 years with no associated pain. Intra oral examination revealed that the nodule is spherical in shape, 2 x 2 cm in size, firm, smooth surfaced and mobile noted in the alveolar mucosa mainly in mucobuccal fold of maxillary right canine region [Table/Fig-1]. There was no much change in the size and other features of the lesion in the due course. The patient was otherwise healthy without any systemic signs and symptoms. The patient works as a taxi driver and lives in a joint family of middle income group. Medical and family histories were non-contributory.
A clinical differential diagnosis of mucocele, lymphangioma and minor salivary gland tumor were given. The lesion was surgically excised under local anesthesia and sent for histopathological examination [Table/Fig-2]. Solely on the basis of histopathological findings, a diagnosis of cysticercosis was made.
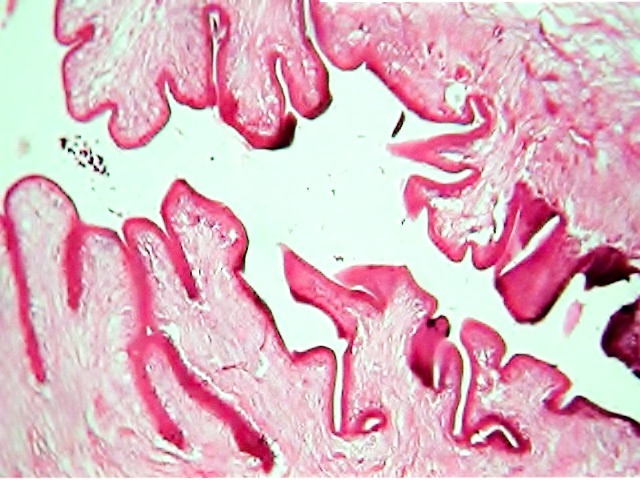
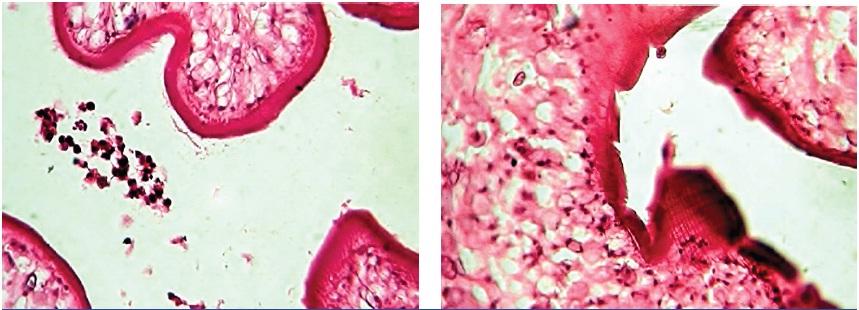
Microscopically, the excised tissue showed a thin fibrous connective tissue capsule adjacent to a cystic cavity containing a duct like tubal segments that was lined by a homogeneous membrane typical of cysticercosis cellulosae (larval form of Taenia solium) [Table/Fig-2]. Cyst wall and outer fibrous tissue [Table/Fig-3a,3b] was presenting in many papillary projections along with numerous inflammatory cell infiltrations and macrophages [Table/Fig-4a,4b]. A complete blood count and stool examination was performed, results of which were not significant and within normal limits.
Discussion
Cysticercosis is an infection with cysticercus cellulosae, the larval stage of Taenia solium or pork tape warm [1]. Cysticercosis is more Sectionprevalent in developing countries, mainly the sub- Asian continent, Africa, Peru and Mexico [2]. Cysticercosis was first described by Johannes Udalric Rumler in 1555. By the middle of the 19th century, it was established that cysticercosis was caused by the ingestion of the eggs of T. solium. However, intially, the connection between tapeworms and cysticercosis had not been recognized. Several laboratory tests and radiologic imaging techniques have been implemented to confirm a definite diagnosis of cysticercosis. However, histopathology and advanced molecular techniques have emerged as tools for conformational diagnosis [3].
Cysticercosis may involve many parts of the body including the subcutaneous tissues, eye, heart, liver, lungs, and peritoneum. Cysticercosis very rarely affects the oro-maxillo-facial region [4]. Although the exact incidence is unknown, oral cysticercosis is considered a rare event and presents as a component of disseminated cysticercosis [5]. Oral cysticercosis Dixon and Lipscomb found that only 1.8% of the cases of cysticercosis had oral involvement [6]. The oral cysticercosis may present as variety of benign lesions. Lesions on the buccal mucosa may be diagnosed as fibroma, mucocele and a plethora of other benign mesenchymal tumors, even benign salivary gland neoplasms cannot be left in the differential diagnosis [7].
Intraorally, the favored sites for the development of cysticerci are the lips, cheeks and tonque. Most oral presentations are in the form of painless, well- circumscribed, soft swellings that may mimick fluctuant lesions like mucocele [8]. Treatment of oral cysticercosis is surgical excision.
In the present case, the patient complained of a solitary nodule in the buccal vestibule, which was asymptomatic. Histopathologic examination of the intraoral nodule was characteristic in the present case and the authors wish to stress to include cysticercosis in the differential diagnosis of oral nodular lesions. In the present case, the patient had no other symptoms of cysticercosis. Hence no additional treatment was given. The patient after periodic follow-ups showed satisfactory response and no occurrence was evident.
Post operative image showing area of submucosal nodule on right vestibule near maxillary canine region

Duct-like invagination lined by bilayered eosinophilic membrane (Haematoxylin and eosin stain, Original magnification x 250)
Photomicrograph showing caudal end of larva lined by acellular, homogeneous eosinophilic membrane (H & E Stain, Original magnification X100)
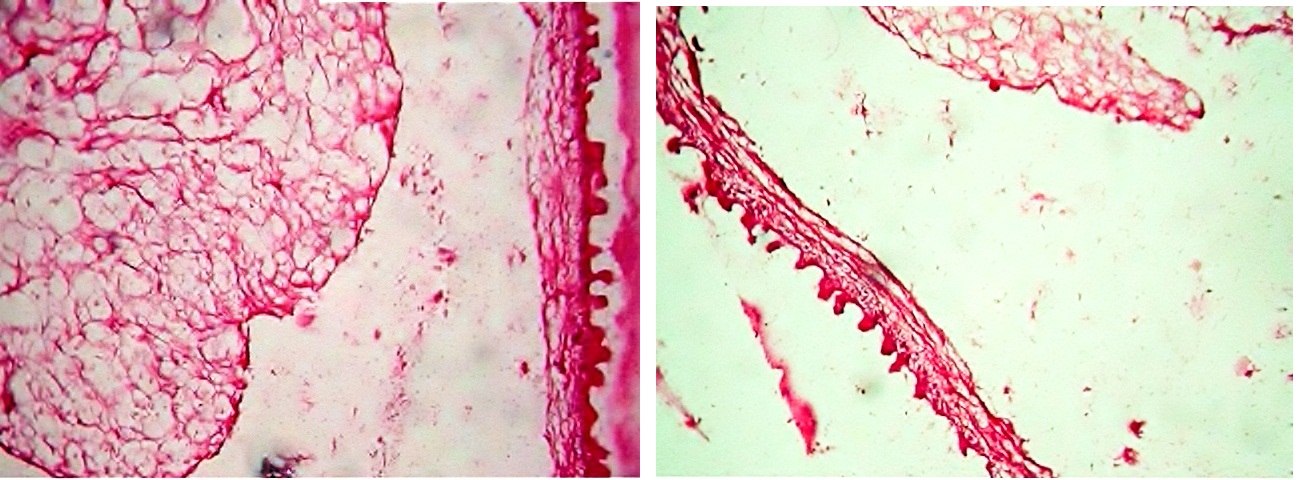
Photomicrograph showing caudal end of larva lined by acellular, homogeneous eosinophilic membrane (H & E Stain, Original magnification X100)
Summary and Conclusion
Oral cysticercosis is a rare disease caused by the parasite Cysticercus cellulosae. Most oral presentations are in the form of painless, well- circumscribed, soft swellings that may mimick fluctuant lesions like mucocele, fibroma or benign salivary gland lesion. The final diagnosis has to be done based on the histopathologic examination. In the present case, the patient complained of a single asymptomatic nodule in the upper buccal vestibule.
[1]. JL Hernandez, G Leung, DM McKay, Cestode regulation of inflammation and inflammatory diseases.Int J Parasitol. 2013 43(3-4):233-43. [Google Scholar]
[2]. E Romero de Leon, A Aguirre, Oral cysticercosis.Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995 79:572-77. [Google Scholar]
[3]. WA Delgado-Azañero, A Mosqueda-Taylor, R Carlos-Bregni, Oral cysticercosis: a collaborative study of 16 cases.Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007 103:528-33. [Google Scholar]
[4]. NJ Mazhari, N Kumar, S Jain, Cysticercosis of the oral mucosa: aspiration cytologic diagnosis.J Oral Pathol Med. 2001 30:187-89. [Google Scholar]
[5]. P Pinswasdi, DJ Charoensiri, Cysticercosis in labial tissue. Case report.Aust Dent J. 1997 42:319-21. [Google Scholar]
[6]. HBF Dixon, FM Lipscomb, Cysticercosis, an analysis and follow up of 450 cases.: Privy Council, Med. Res. Council, Special Report series No. 299. Her Majesty’s Stationary Office.London. 1961 [Google Scholar]
[7]. HH Garcia, OH Del Brutto, Taenia solium cysticercosis.Infect Dis Clin North Am. 2000 14:97-119. [Google Scholar]
[8]. LS Hansen, RH Allard, Encysted parasitic larvae in the mouth.J Am Dent Assoc 1984 108(4):632-36. [Google Scholar]