Benign Osteoblastoma of Maxilla: A Case Report Emphasizing the Histopathological Differential Diagnosis
Deepak Pandiar1, Shameena P M2, Saakshi Gulati3, Vishal Singh Banyal4, Amit Kumar5
1 Senior Resident, Department of Oral Pathology, GDC Calicut, Kerala, India.
2 Former HOD, Department of Oral Pathology, GDC Calicut, Kerala, India.
3 Senior Resident, Department of Oral Medicine and Diagnosis, GDC Calicut, Kerala, India.
4 Post Graduate Trainee, Department of Oral Pathology, GDC Calicut, Kerala, India.
5 Post Graduate Trainee, Department of Oral Pathology, GDC Calicut, Kerala, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Deepak Pandiar, Senior Resident, Department of Oral Pathology, GDC Calicut-8, Kerala, India. Phone : 09497588985, E-mail : deepakpandiar1923@yahoo.com
Benign osteoblastoma is a rare bone tumour characterized histologically by production of woven bone spicules, which are bordered by prominent osteoblasts. It mainly affects male teenagers and young adults. A case of benign osteoblastoma of maxilla in a nineteen years old male is reported here. Also, histological comparison is made between benign osteoblastoma, aggressive osteoblastoma and osteosarcoma.
Aggressive, Benign osteoblastoma, Maxilla, Osteosarcoma
Case Report
A 19-year-old male patient reported to the Department of Oral Pathology and Microbiology complaining of pain and swelling over the upper right front and back tooth region of jaw of six months duration. The swelling was initially asymptomatic but two months after the onset of swelling the patient experienced a dull intermittent pain which was not relieved by analgesics. There was no associated toothache, pus discharge or bleeding from the swelling. There was no regional lymphadenopathy. Intra oral examination showed a swelling of size 3 x 2 cm in relation to 13–16 regions extending from mesial of 13 to distal of 16 obliterating right muco-buccal sulcus [Table/Fig-1a]. Surface was smooth and mucosa over the swelling was erythematous. On palpation, it was bony hard in consistency with well defined borders. A mild tenderness was elucidated. Buccal and palatal cortical plates were expanded. Routine blood and urine investigations were within normal limits. Radiographic interpretation revealed a predominantly radio opaque lesion of size 2 x 2 cm extending from the mesial aspect of 13 to distal aspect of 16. There was a radiolucent rim over the upper border of the lesion. Borders were well defined and there was no root resorption. Buccal cortical plate expansion was present. Lesion seemed to be attached to the root of 15 as the root morphology of 15 could not be clearly visualized. The floor of the maxillary antrum was pushed upwards [Table/Fig-1b–e]. Based on clinical background and radiographs, provisional diagnoses of benign fibro osseous lesion and odontogenic tumour were made [Table/Fig-1h].
(Benign osteoblastoma): (A) Clinical presentation; (B) Intra-oral radiograph showing radio-opaque mass in relation to 13-16; (C) Extra-oral radiograph of the lesion; (D-E) Shows computed tomographic images; (F-G) H & E sections showing angular osteoblasts, mineralized mass with prominent reversal lines, osteoclasts and areas of haemorrhage (100X); (I) Post-operative extra-oral radiograph
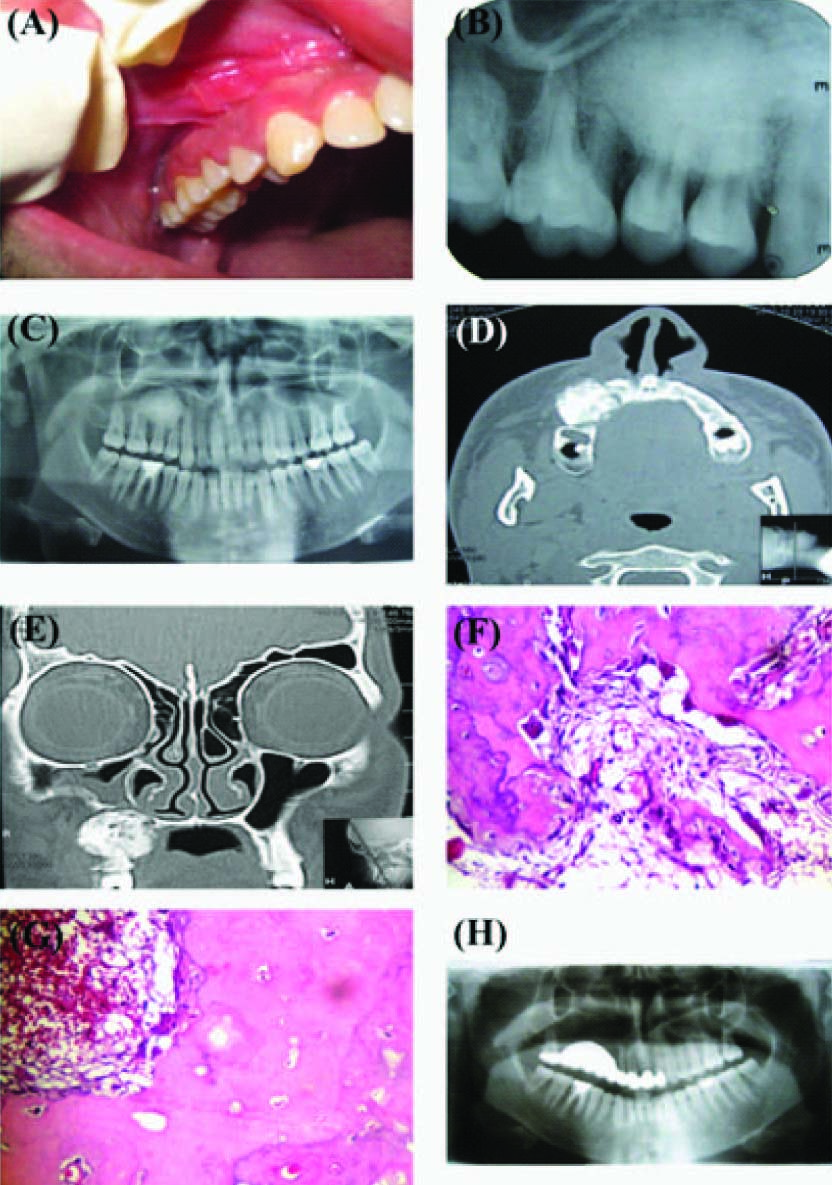
An incisional biopsy was taken which showed area of mineralized tissue, with entrapped osteocytes in lacunae, lined by flattened to angular cells with moderate to ample amount of cytoplasm and deep basophilic nuclei (osteoblastic rimming). Discernible numerous reversal lines were seen in the mineralized tissue. Multinucleated giant cells were seen in the resorption bays. The connective tissue was fibro-vascular with numerous proliferating angular cells [Table/Fig-1f]. Areas of hemorrhage were also seen [Table/Fig-1g]. Based on this a diagnosis suggestive of osteoblastoma was made.
En-bloc resection of the lesion was done under general anaesthesia. The excised specimen showed features indistinguishable from those seen in incised specimen. Final diagnosis of benign osteoblastoma was given. There was no sign of recurrence on a follow up of one year.
Discussion
Osteoblastoma is a rare benign bone forming neoplasm (accounting for about 1% of all bone tumours) which produces woven bone spicules, which are bordered by prominent osteoblasts [1]. It is a disease of male teenagers and young adults [1] and primarily involves the vertebral column, long bones, small bones of hands and feet (metacarpal and metatarsal), and facial bones including the jaw [2]. Literature narrates two main clinico-pathological entities of osteoblastoma: the benign form and an aggressive form [3]. A case of benign osteoblastoma of maxilla in a teenage male is reported here. Also, a pictorial histological comparison is made between benign osteoblastoma, aggressive osteoblastoma and osteosarcoma for better understanding.
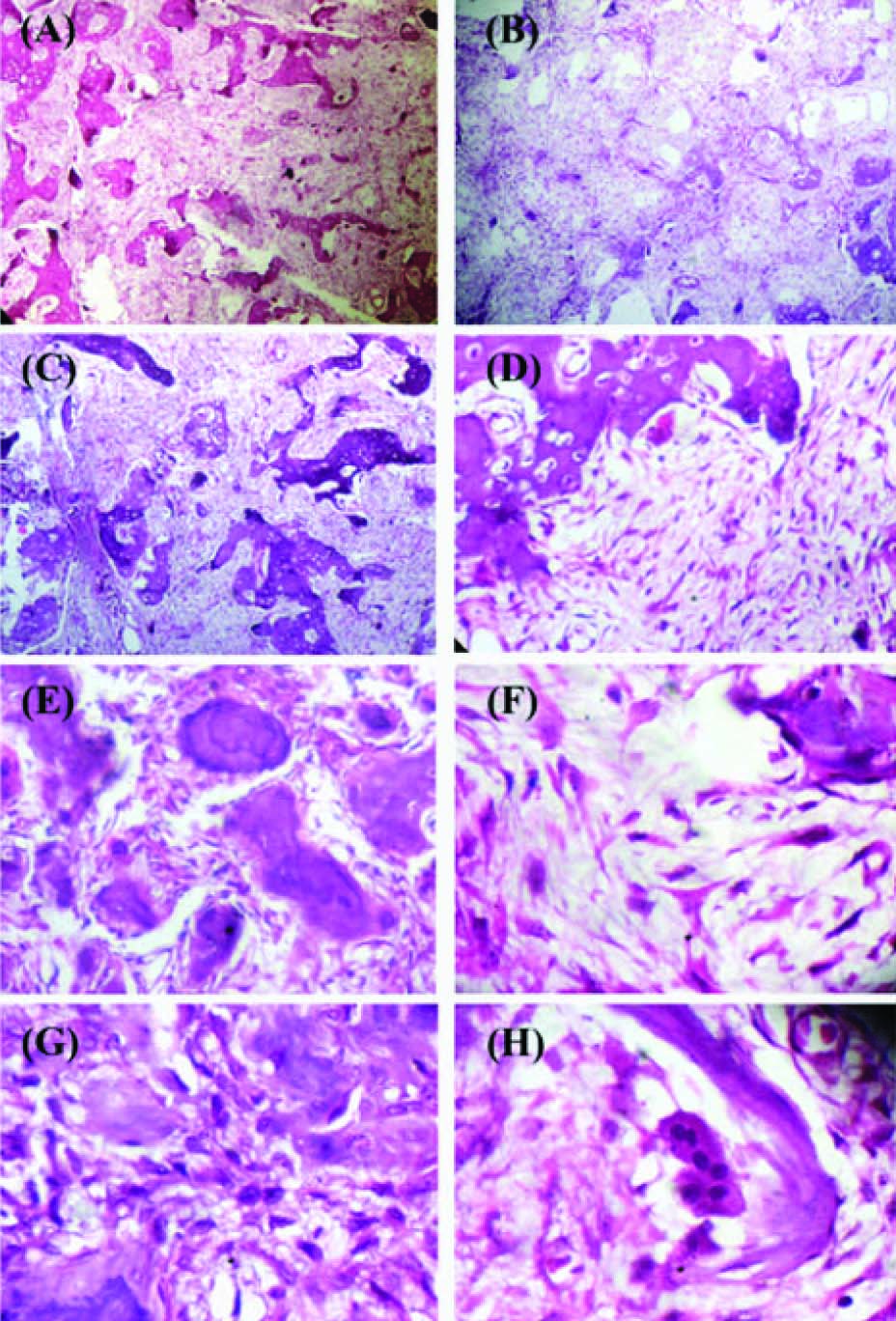
Histologically, this benign neoplasm shows proliferating osteoblasts and forming trabeculae in a fibro-vascular connective tissue stroma. Distinction of this entity from other very closely related lesions is of uttermost significance since they differ in the ministration and the denouement. Benign osteoblastoma should be discriminated from aggressive osteoblastoma (AO) and low grade osteosarcoma (LGO). [Table/Fig-2] shows the differentiating features of AO and LGO. Benign osteoblastomas are characterized by presence of polygonal osteoblasts with moderate amount of cytoplasm and round to oval nuclei with prominent nucleoli. The trabeculae are long and anastomosing with osteoblastic rimming. The vascularity is affluent, often with extravagated red blood cells [1]. The tumour borders are well- delineated. The etio-pathogenesis of this lesion is varied and widely debated in the literature with no clear consensus on its origin. Jaffe and Lichtenstein (1956) stated this lesion to be a true neoplasm of osteoblastic derivation. Other reasons cited in the published writings include trauma, inflammation, abnormal local response of the tissues to injury, and local alteration in bone physiology [2].
Differentiating features of AO and LGS
| AO [Table/Fig-3a–h] | LGO [Table/Fig-4a–h] |
|---|
| Proliferating cells | Large and epithelioid with ample amount of eosinophilic cytoplasm with eccentric round to oval nuclei and multiple prominent nucleoli. | Large round to oval, spindled or epithelioid containing deeply staining cytoplasm and hyperchromatic nuclei with prominent multiple nucleoli. The neoplastic cells tend to grow in an angiocentric fashion |
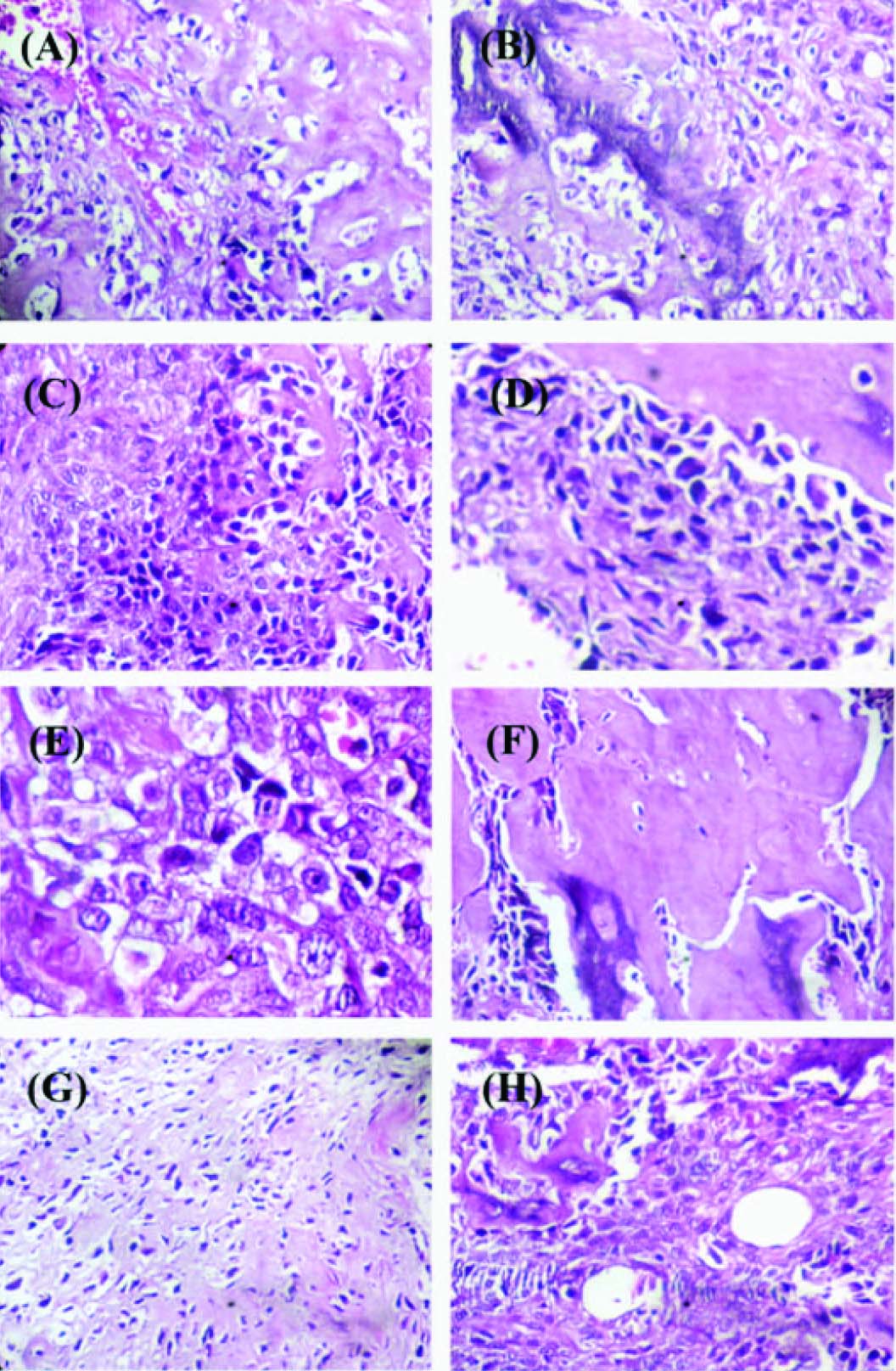
| Stroma | Hypercellular. Multi-nucleated giant cells are not uncommon | Shows dense, pink, refractory and amorphous intercellular material known as osteoid. The thickness of the osteoid is highly variable with the thinnest referred to as “filigree” osteoid. |
| Mineralized matrix | Trabeculae are large and irregular with osteoblastic rimming and may show reversal lines. | Osseous matrix also has a predisposition for appositional deposition upon previously existing normal bone trabeculae (i.e., “scaffolding”). Sometimes the neoplastic cells are confined within large amounts of bone matrix and thus appear as small, pyknotic, minimally atypical cells, a feature referred to as “normalization”. |
(H & E photomicrographs of aggressive osteoblastoma): (A-C) Showing hypercellular proliferating osteoblasts with large irregular bony trabeculae and osteoblastic rimming (40X). (D) Irregular trabeculae with entrapped osteocytes and osteoclast in resorption bays (100X); (E-H) showing reversal lines, polygonal osteoblasts with multiple nucleoli, epithelioid osteoblasts and multinucleated giant cells (Oil immersion)
(H & E photomicrographs of Osteosarcoma): (A-B) Tumour osteoid which appears mineralizing at areas (100X). (C-E) Neoplastic cells showing varying morphology, dysplastic features and occasional atypical mitotic figures (C and D- 100X; E-400X); (F) Normalization of cells (100X); (G) Tumour osteoid in filigree pattern (100 X); (H) Angiocentric distribution of neoplastic cells (100 X)
Radiographically, other differentials include fibro-osseous lesions, and odontogenic tumours. Fibro-osseous lesions such as late lesions of fibrous dysplasia are largely sclerotic and radiographically show features similar to osteoblastoma. However, classical fibrous dysplasia has a ground glass appearance with poorly discernible borders that appear to blend in with the surrounding unaffected bone. Similarly, late ossifying fibromas manifest as central radio-opaque masses surrounded by a radiolucent rim akin to osteoblastomas. But theses lesions of ossifying fibromas tend to be well demarcated and 70% of the lesions occur in the mandible [4]. Among odontogenic tumours cementoblastoma, odontoma and desmoplastic ameloblastoma may show radiographic appearance similar to osteoblastomas. But all aforementioned odontogenic tumours show distinct features histologically posing no problem in making a confirmatory diagnosis.
Dorfman in 1973 proposed the term ‘aggressive osteoblastoma’ [5]. Other terms used in the literature for this entity are ‘pseudomalignant osteoblastoma’ and ‘malignant osteoblastoma’ [6–7]. In contrary to benign osteoblastoma, aggressive osteoblastoma show aggressive clinical behavior with fast onset. These tumours tend to recur after conservative therapy. Conventional osteosarcoma is universally fatal thus it must be viewed as a systemic disease at the time of initial diagnosis [1].
There is no universally accepted diagnostic criterion for this spectrum of jaw tumours. And with an increasing number of reported cases in the literature, a universal consensus is essential for the diagnosis of jaw bone tumours and furthermore the treatment module differs. Osteoblastoma should be treated by curettage. Large lesions may have to be excised. The prognosis is excellent and recurrences are unusual and more likely in those cases, which were curetted from a bone, which has difficult surgical access [1]. AO and osteosarcomas are managed by more aggressive treatment [8–9].
Conclusion
Benign osteoblastoma is a rare bone tumour of teenager males with excellent prognosis. This tumour clinically and histologically resembles aggressive osteoblastoma and low grade osteosarcomas which differ in their treatment plan and of course the prognosis. Thus proper evaluation of the patient and a correlation with radiographic and histological findings is essential for the betterment of the patient.
[1]. Fletcher CDM, Unni KK, Mertens F, World Health Organization Classification of TumoursPathology and Genetics of Tumours of Soft Tissue and Bone 2002 LyonIARC Press:259 [Google Scholar]
[2]. Bokhari K, Hameed MS, Ajmal M, Togoo RA, Benign osteoblastoma involving maxilla: a case report and review of the literatureCase Rep Dent 2012 2012:351241doi: 10.1155/2012/351241 [Google Scholar]
[3]. Woniak AW, Nowaczyk MT, Osmola K, Golusinski W, Malignant transformation of an osteoblastoma of the mandible: case report and review of the literatureEur Arch Otorhinolaryngol 2010 267:845-49. [Google Scholar]
[4]. Alawi F, Benign fibro-osseous diseases of the maxillofacial bones. A review and differential diagnosisAm J Clin Pathol 2002 118(Suppl):S50-70. [Google Scholar]
[5]. Dorfman HD, Malignant transformation of benign bone lesionsSeventh National Cancer Conference Proceedings 1973 PhiladelphiaJB Lippincott:901-13. [Google Scholar]
[6]. Mirra JM, Kendrick RA, Kendrick RE, Pseudomalignant osteoblastoma versus arrested osteosarcoma: A case reportCancer 1976 37:2005-14. [Google Scholar]
[7]. Schajowicz F, Lemos C, Malignant osteoblastomaJ Bone Joint Surg (Br) 1976 58(B):202-11. [Google Scholar]
[8]. Lypka MA, Goos RR, Yamashita DD, Melrose R, Aggressive osteoblastoma of mandibleInt J Oral Maxillofac Surg 2008 37:675-78. [Google Scholar]
[9]. Chaudhary M, Chaudhary SD, Osteosarcoma of jawsJ Oral Maxillofac Pathol 2012 16:233-38. [Google Scholar]