Endocarditis in Mitochondrial Neurogastrointestinal Encephalomyopathy (MNGIE) Syndrome: The First in the Literature
Mustafa Yolcu1, Canan Yolcu2, Zekeriya Kaya3, Ender Ozgun Cakmak4, Yusuf Sezen5
1 Faculty, Department of Cardiology, Sanlıurfa Education and Research Hospital, Sanlıurfa, Turkey.
2 Faculty, Department of Pediatrics, Sanlıurfa Child Diseases Hospital, Sanlıurfa, Turkey.
3 Faculty, Department of Cardiology, Sanlıurfa Education and Research Hospital, Sanlıurfa, Turkey.
4 Faculty, Department of Cardiology, Sanlıurfa Education and Research Hospital, Sanlıurfa, Turkey.
5 Faculty, Department of Cardiology, Harran University School of Medicine, Sanlıurfa, Turkey.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Mustafa YOLCU, Sanlıurfa Bölge Eoitim ve Arastırma Hastanesi, Esentepe, 63000, Sanlıurfa, Turkey. Phone : 905552383776, E-mail : yolcudoctor@gmail.com
Mitochondrial neurogastrointestinal encephalomyopathy (MNGIE) syndromes is a rarely seen multisystem disorder with autosomal recessive inheritance due to thymidine phosphorylase gene mutation. It is characterized by progressive external ophthalmoplegia and/or pitosis, progressive gastrointestinal dismotility and abdominal pain, postprandial emesis, cachexia, demyelinating peripheral neuropathy, symmetrical and distal weakness especially in lower extremities and diffuse leucoencephalopathy in cranial magnetic resonance. Endocarditis is the infectious and inflammatory disease of the endothelial surface of the heart. MNGIE syndrome is a condition in which immune system is suppressed and infection risk increased. Herein we summarized a previously not reported endocarditis case in a patient with MNGIE syndrome who was under follow up for three years. In MNGIE syndrome of acute dyspnea, infective endocarditis should be kept in mind and prompt evaluation for surgical treatment should be done.
Endocarditis, MNGIE syndrome, Mitral valve
Case Report
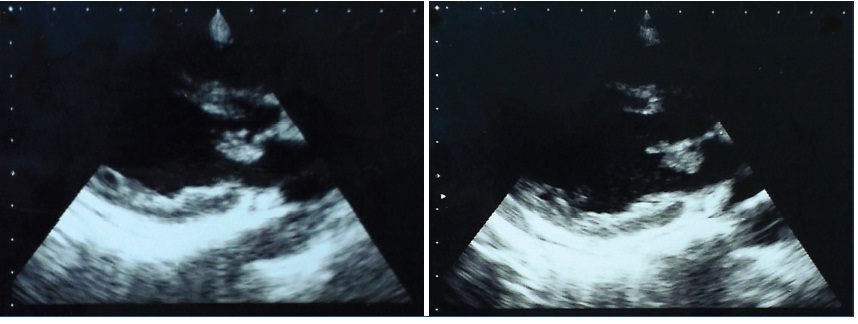
A 19-year-old female patient was admitted to our emergency clinic with the complaints of progressive dyspnea and fever for two days. In her past history, she was known to have MNGIE syndrome for three years. In the family history, first MNGIE syndrome event was detected in her brother and he had died because of pulmonary infection and sepsis four years after diagnosis. In her physical examination, she was 34 kgs, had pulse rate of 140 bpm and blood pressure of 80/55 mmHg with a 40 °C body temperature. She was tachycardic with S3 and had a 2/6 grade systolic regurgitation murmur at mesocardiac area. In her pulmonary system examination, crepitant rales were detected on bazal and mid zones of lungs. Her telecardiogram was consistent with pulmonary edema. In the transthorasic echocardiography, interatrial septum intact, tricuspid valve and left ventricular functions were normal but a 10x9 mm sized vegetation was detected on the atrial face of anterior mitral leaflet leading severe mitral regurgitation [Table/Fig-1]. Urinary, pharyngeal and sputum cultures were taken. The five blood cultures taken from the patient were incubated for four weeks in aerobic, anaerobic and fungal culture. The one year old venous port was removed and samples from port, including its tip, were taken for aerobic, anaerobic and fungal cultures. Intravenous diuretic, vancomycin plus gentamycin and low molecular weight heparin therapy was started soon. The patient’s symptoms was improved after the medical treatment. A surgical was planned after a period of time to use antibiotic. In the fourth day of hospitalization, she had suddenly experienced respiratory arrest and was intubated. She was unconsicious during mechanical ventilation period and had lost her life due to cardiac arrest on the sixth day of intubation. After death of the patient, all of the cultures were followed and examined but there was no growth in any of them.
View of vegetation in the transthorasic echocardiography
Discussion
MNGIE syndrome is a rarely seen multisystem disorder with autosomal recessive inheritance due to thymidine phosphorylase gene mutation [1]. It is characterized by progressive external ophthalmoplegia and/or pitosis, progressive gastrointestinal dismotility and abdominal pain, postprandial emesis, cachexia, demyelinating peripheral neuropathy, symmetrical and distal weakness especially in lower extremities and diffuse leucoencephalopathy in cranial magnetic resonance [2].
Although the symptoms commonly appear during first and second decades, it can be asymptomatic until fifth decade [3]. In MNGIE, onset of symptoms and sequence of organ involvement varies significantly between patients and gastrointestinal involvement is reported to be the first system leading symptoms in half of the patients [3]. Peripheral neuropathy or extraocular muscle weakness was the most common presentation in previous reports [3]. In MNGIE syndrome, it is considered that suppressed immune system increasing infection tendency can cause vegetatiton formation in native valves.
Endocarditis is the infectious and inflammatory disease of the endothelial surface of the heart [4]. Staphylococci are the most frequently detected microorganisms [4]. However, in 5% of the patients, any microbial growth can not be shown which is called culture negative endocarditis [4]. The most commonly seen microorganisms in culture negative endocarditis are Coxiella burnetti and Bartonella subspecies [4].
Herein, we summarized a previously not reported endocarditis case in a patient with MNGIE syndrome who was under follow up for three years. The echocardiography of our patient performed two years ago was normal and in the present echocardiographic examination, mitral and aortic valves were structurally normal, also, excluding any valvular etiology. There was not any microbiological growth in any of the cultures. In the light of these findings, we indicated that a culture negative endocarditis can be seen on normal valve in MNGIE syndrome. Thus, endocarditis sould be kept in mind in those patients with acute dyspnea.
Conclusion
MNGIE syndrome is a condition in which immune system is suppressed and infection risk increased. In case of acute dyspnea, infective endocarditis should be kept in mind and prompt evaluation for surgical treatment should be done.
[1]. Nishino I, Spinazzola A, Hirano M, Thymidine phosphorylase gene mutations in MNGIE, a human mitochondrial disorderScience 1999 283:689-92. [Google Scholar]
[2]. Colak Y, Tuncer I, Caglar E, Barutcu D, Ulasoglu C, Kızıltas S, Mitochondrial neurogastrointestinal encephalomyopathy: Case reportTurk J Gastroenterol 2010 21:305-07. [Google Scholar]
[3]. Garone C, Tadesse S, Hirano M, Clinical and genetic spectrum of mitochondrial neurogastrointestinal encephalomyopathyBrain 2011 134:3326-32. [Google Scholar]
[4]. Slipczuk L, Codolosa JN, Davila CD, Romero-Corral A, Yun J, Pressman GS, Infective Endocarditis Epidemiology Over Five Decades: A Systematic ReviewPlos One 2013 8:e82665 [Google Scholar]