Retroperitoneal Schwannoma: An Atypical Presentation
Siddha K Loka Vijayan1, Sunil Shetty2, Sri Ram Bhat3, Suyog Shetty4, Urmila N Khadilkar5
1 Post Graduate, Department of General Surgery, Kasturba Medical College, Mangalore, India.
2 Associate Professor, Department of General Surgery, Kasturba Medical College, Mangalore, India.
3 Professor, Department of General Surgery, Kasturba Medical College, Mangalore, India.
4 Assistant Professor, Department of General Surgery, Kasturba Medical College, Mangalore, India.
5 Professor, Department of Pathology, Kasturba Medical College, Mangalore, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. S. K. Loka Vijayan, Post Graduate, Department of General Surgery, Kastuba Medical College, Mangalore-575001, India. Phone : +91 9901832864, E-mail : lokavijayan@gmail.com
Schwannoma is a rare tumour arising from Schwann cells in myelinated neural sheath of the nerves. They can arise in various places like head, neck, extremities, adrenal, retro peritoneum, psoas muscle. We here present a case of 33-year-old male who came with features of acute pancreatitis, with incidentally detected mass in presacral region on ultrasonography. Investigations like CECT and MRI were suggestive of neurofibroma, radical excision of the mass was done which showed solitary encapsulated tumour and cut sections showed areas of necrosis, and histopathologically it was proven as schwannoma. Most of the schwannoma’s are benign, but rarely malignant transformation can occur. It can be associated with von Recklinghausen disease. Benign tumours have excellent prognosis, malignant tumours can present at later date with metastasis after excision also. Radiology plays a key role in diagnosis and follows up. Treatment is radical excision of tumour; recurrence is most common and has to be carefully followed up.
Retroperitoneal space, Schwann cells, Schwannoma, Von recklinghausen disease
Case Report
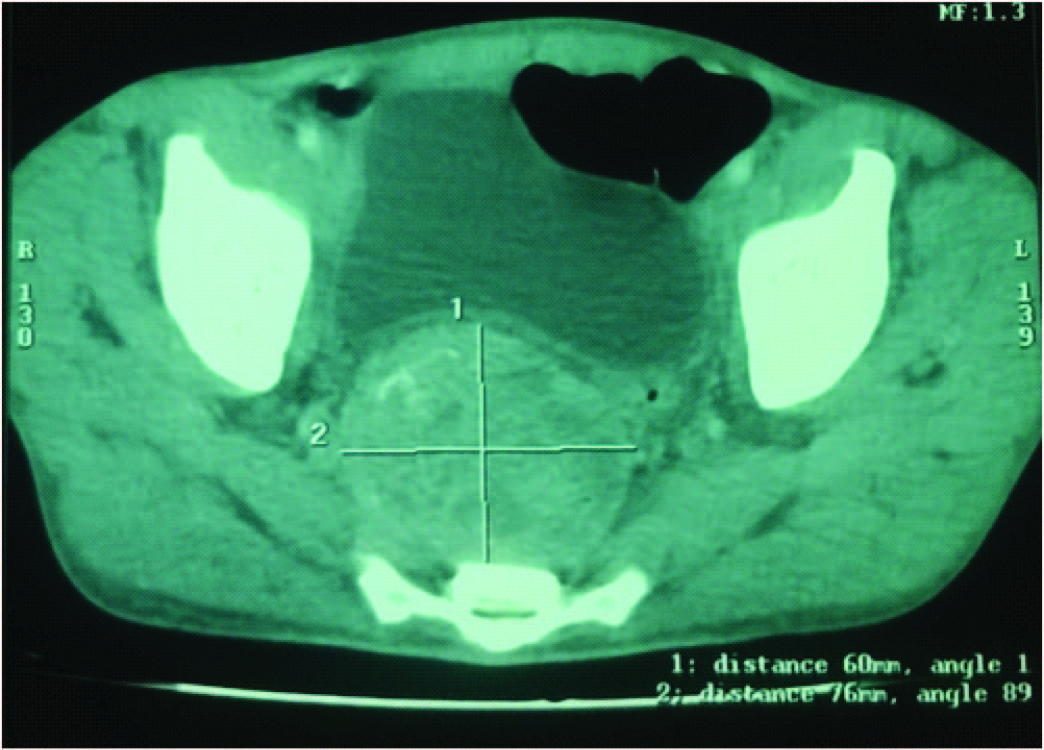
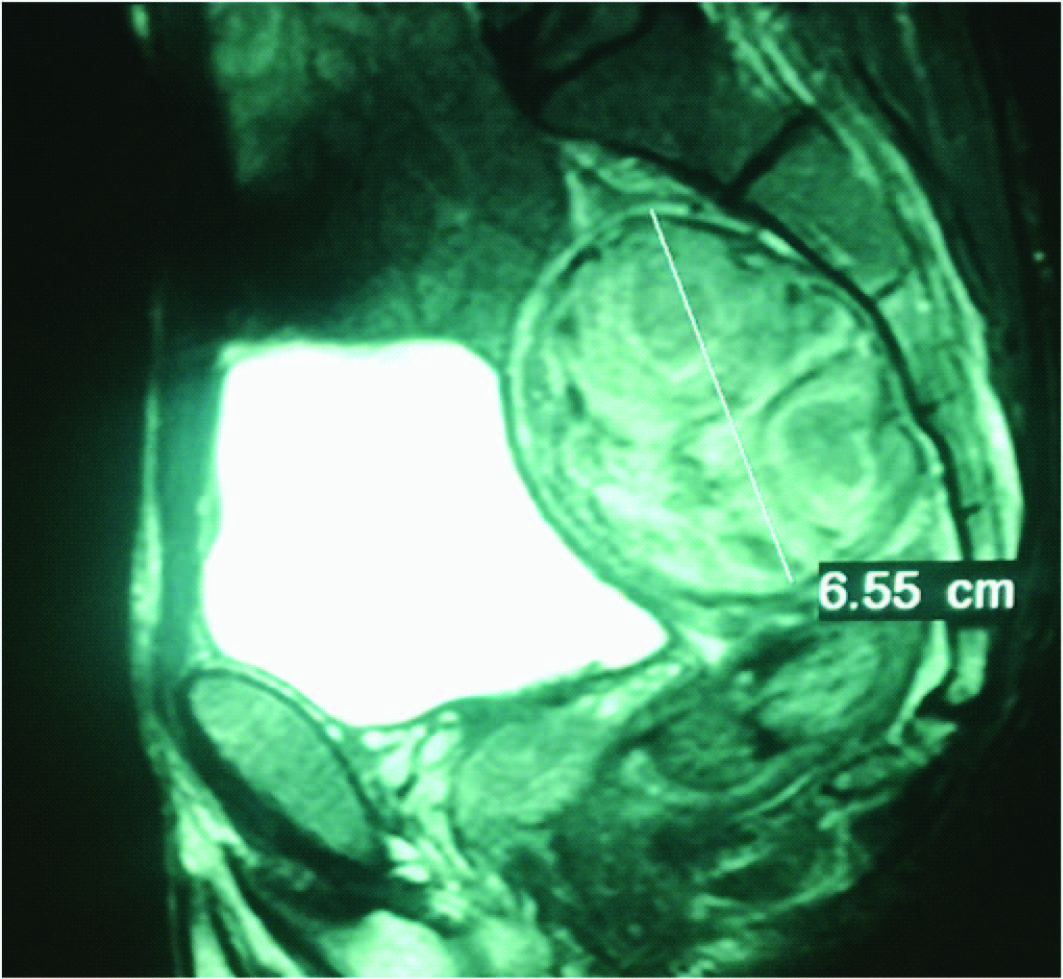
A 33-year-old male presented to emergency department with a complaint of pain abdomen in the epigastric region since past three days. On physical examination there was diffuse abdominal tenderness along with diffuse guarding and per rectal examination revealed a hard pre sacral mass in the sacral promontory region. Ultrasound abdomen showed minimal amount of free fluid with 3×3 cms capsulated mass at the presacral region. Blood investigations revealed a raise in total count, serum amylase levels, and deranged renal function tests. After treating the patient for acute pancreatitis for 10 days, CECT abdomen was done which revealed a 8×8×6 cms heterogenous enhancing mass with peripheral rim of calcification’s and central areas of necrosis in the presacral region [Table/Fig-1]. MRI with contrast showed hypo intense lesion in T1 weighted images and hyper intense on T2 weighted images without involvement of adjacent structures suggestive of neurofibroma or liposarcoma [Table/Fig-2].
CECT showing heterogenous enhancing lesion
MRI in lateral view showing the encapsulated lesion
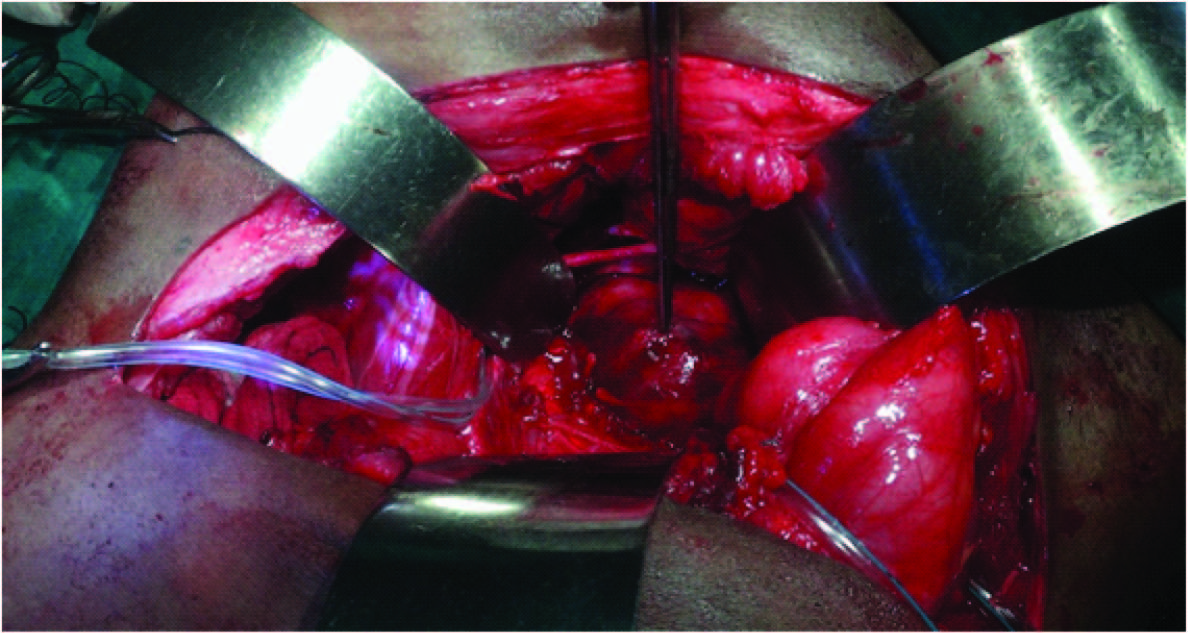
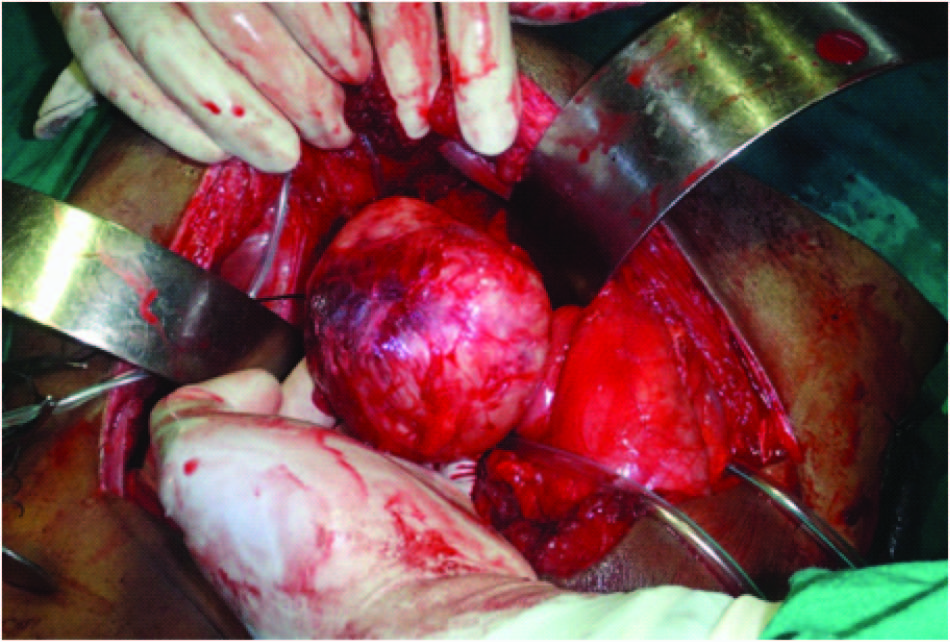
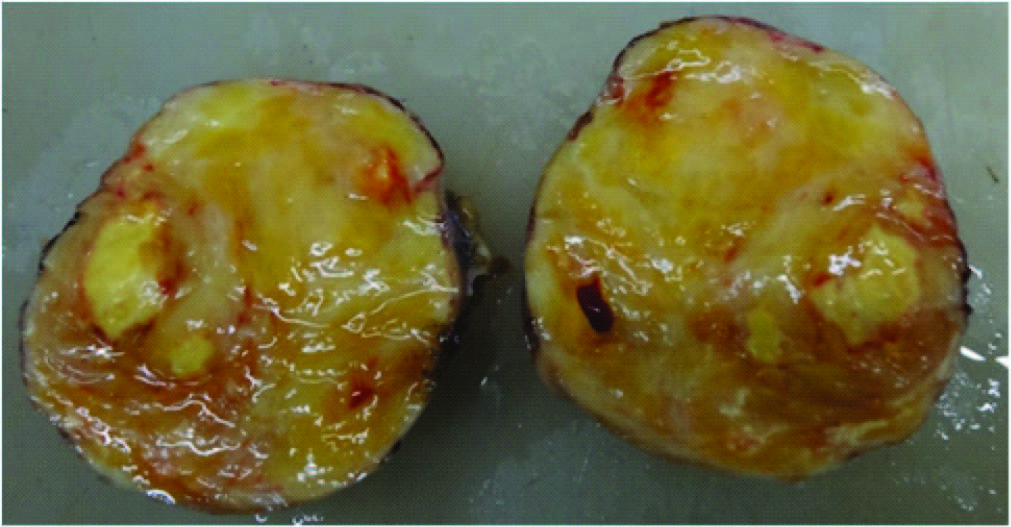
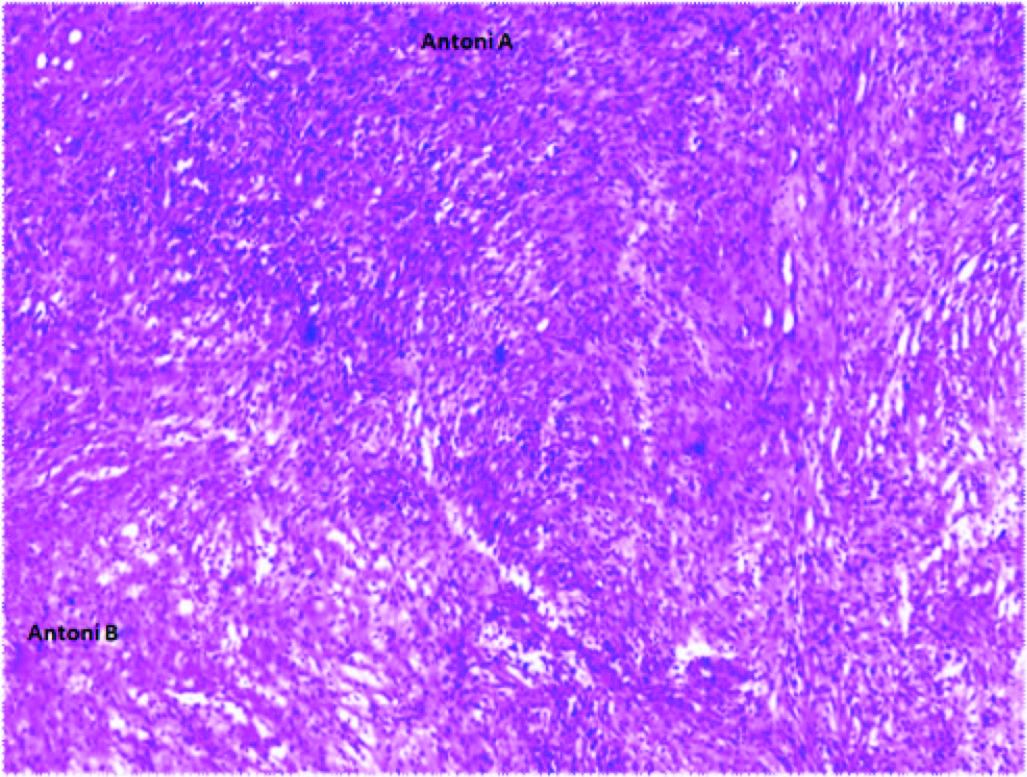
As patient was not willing for FNAC of the mass lesion, so radical excision of mass was planned, with extended left sided Pfannenstiel incision, by extra peritoneal approach. A well- defined smooth encapsulated mass of 8×6×4cms was excised without damaging other structures [Table/Fig-3,4,5] Cross sections of the mass showed solid yellow with areas of haemorrhage with focal areas of calcification [Table/Fig-6]. Postoperatively patient did not develop any incontinence for bladder and bowel. Histopathology revealed features suggestive of schwannoma with no mitosis, and multiple foci of coagulative necrosis bordered by atypical cells [Table/Fig-7].
Intraoperative dissection of specimen
Intraoperative excision of specimen
Solid encapsulated lesion

Cut sections showing areas of necrosis and calcifications
Histopathological picture showing hyperdense Antoni A and hypodense Antoni B areas
Patient is in regular follow up till now since seven months and with imaging showed no recurrence of the tumour.
Discussion
Schwannoma’s are the tumours that are arising from the Schwann cells of peripheral nerve fibre, and are usually found in the head, neck and extremities [1]. Around 5 – 8% cases are in association with Von Recklinghausen’s disease [2]. They are mostly benign in nature, more commonly occurs in adult females between 20–50 y age with a male to female ratio of 2:3 [3]. Retroperitoneal schwannoma’s more commonly found in paravertebral spaces and pre sacral region [4], it is unusual in these locations in absence of Von Recklinghausen’s disease. Among retroperitoneal schwannomma’s around 0.7% are benign and 1.7% are malignant were reported [5]. The capsule of these tumours is derived from epineurium. Retroperitoneal schwannoma’s produces vague symptoms like abdominal pain and distention [6]. MRI is the investigation of choice which describes about the origin, extent, and internal structure, and infiltration of the lesion. The typical diagnostic signs in MRI are “Target sign” which is hypo –intense centre with hyper-intense periphery, and “Fascicular sign” which is seen in presence of fascicular bundles [7]. These findings will be lacking in retroperitoneal schwannoma which makes the diagnosis challenging. Ultrasonography is useful in guided biopsies and CT scans detects malignant changes associated like bony erosions [8]. In case of malignant transformation irregular margins with infiltration into adjacent structures are seen [1]. In a study carried out in Japan, of all the cases of schwannoma 94 (72.3%) were benign and 36 (27.7%) were malignant [9]. Very rarely schwannoma’s undergo malignant transformation and invades adjacent organs like colon, kidneys, and adjacent viscera [10]. Tissue diagnosis can be achieved by FNAC and excision biopsies. CT guided biopsies and FNAC are not always reliable as they should contain significant amount of Schwann cells, and FNAC from the areas of degeneration will be misdiagnosed as malignant. FNAC increases the risk of haemorrhage, infection, tumour seeding so it is not preferred by many surgeons. Calcification and cystic degeneration occurs in these tumours were around 23% and 66% respectively [6]. Diagnosis for malignant changes lack specific standardised criteria except for features like dense fascicules in marble like pattern comprising of asymmetrically tapered spindle cells [11]. Microscopically dense cellular areas are named as “Antoni A” areas and necrotic hypo dense areas as “Antoni B” areas [7] [Table/Fig-7]. Malignancy is usually characterised by mitotic figures, pleomorphism, and infiltration of blood vessels. Malignant schwannomas are more aggressive and likely to have high incidence of local recurrence after excision and have chance of distant metastasis, more commonly associated with Von Recklinghausen disease. Malignancy could not be ruled out pre operatively and by frozen sections, so complete excision with negative margins is recommended. Recurrence of the tumour is usually within six months of surgical excision, and it varies from 16% to 54% [12]. The completeness of excision and tumour grading are the most important in assessing the recurrence and survival. Prognosis is usually good, but related with the site of the lesion, differentiation, invasion, and excision clearance [13]. Radical excision is considered as the best treatment for this condition but controversies exists regarding the margin clearance. Recent advances by laparoscopic excision have also been explained [14] and adjuvant chemotherapy and radiation will not add up for the benefit for schwannomas. Differential diagnosis of retroperitoneal schwannomas includes paraganglioma, liposarcoma, and malignant fibrous histiocytoma.
[1]. Wong CS, Chu TY, Tam KF, Retroperitoneal Schwannoma: a common tumor in an uncommon siteHong Kong Medical Journal 2010 16:66-68. [Google Scholar]
[2]. Parfitt Jr HG, Hamonnd ME, Midletton Jr AW. Perirenal malignant schwannoma: a case report and review of literatureJ Urol 1982 128:1299-301. [Google Scholar]
[3]. Ohigashi T, Nonaka S, Nakanoma T, Ueno M, Deguchi N, Laparoscopic treatment of retroperitoneal benign schwannomaInt J Urol 1999 6:100-03. [Google Scholar]
[4]. Song JY, Kim SY, Park EG, Kim CJ, Kim DG, Lee HK, Schwannoma in the retroperitoneumJ Obstet Gynaecol 2007 33:371-75. [Google Scholar]
[5]. Goh BK, Chung YF, Chow PKH, Ooi LLPJ, Wong WK, Retroperitnoeal schwannomaAmerican Journal of Surgery 2006 192:14-18. [Google Scholar]
[6]. Kalayci M, Akyuz U, Demirag A, Gurses B, Ozkan F, Gokce O, Retroperitoneal Schwannoma: a Rare CaseCase Reports in Gastrointestinal Med 2011 2011:465062 [Google Scholar]
[7]. Hughes MJ, Thomas JM, Fisher C, Moskovic EC, Imaging features of retroperitoneal and pelvic schwannomasClinical Radiology 2005 60:886-93. [Google Scholar]
[8]. Medcyclpaedeia. Neuroradilogy: Neurilemmoma. [cited 2012 Dec 10] Avilable from: URL:http://www.medcyclopedia.com [Google Scholar]
[9]. Okamura K, Ito K, Aota Y, Suzuki Y, Shimoji T, A case report of retroperitoneal malignant schwannomaHinyokika Kiyo 1984 30:1045-51. [Google Scholar]
[10]. Enzinger FM, Weiss SW, Benign tumors of peripheral nervesSoft Tissue Tumours 1995 3St LouisMosbyEnzinger FM, Weiss SW:821-88. [Google Scholar]
[11]. Cury J, Coelho RF, Srougi M, Retroperitoneal schwannoma: case series and literature reviewClinics 2007 62:359-62. [Google Scholar]
[12]. Andonian S, Karakiewicz PI, Herr HW, Presacral cystic schwannoma in a manUrology 2003 62:8-10. [Google Scholar]
[13]. Song JY, Kim SY, Park EG, Kim CJ, Kim DG, Schwannoma in the retroperitoneumJ Obstet Gynaecol Res 2007 33:371-75. [Google Scholar]
[14]. Yukio K, Kazunori Endoscopic assisted mini laparotomy for retroperitoneal schwannomasJpn J Clin Oncol 2002 32(5):177-80. [Google Scholar]