A Case of Vander Woude Syndrome with Rare Phenotypic Expressions
Anurag Tripathi1, Brijesh Tiwari2, Shalini Gupta3, Ranjit Patil4, Vikram Khanna5
1 Assistant professor, Department of Oral Medicine and Radiology, King George Medical University, Lucknow,Uttar Pradesh,India.
2 Senior Research Fellow, Department of Dental Research & Implantology, Institute of Nuclear Medicine and Allied Sciences (INMAS), Defence Research and Development Organization (DRDO) Ministry of Defence, Government of India, Timarpur, Delhi, India.
3 Associate Professor, Department of Oral Pathology, King George Medical University, Lucknow, Uttar Pradesh, India.
4 Professor & Head, Department of Oral Medicine and Radiology, King George Medical University, Lucknow, Uttar Pradesh, India.
5 Assistant Professor, Department of Oral Medicine and Radiology, King George Medical University, Lucknow,Uttar Pradesh,India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Anurag Tripathi, Assistant Professor, Department of Oral Medicine and Radiology, King George Medical University, Lucknow-226003, India. Phone : 09839408707, E-mail : dranuragtripathi@yahoo.co.in
Van der Woude syndrome (VWS) is a rare developmental disorder with an autosomal dominant inheritance. The prevalence of VWS varies from 1:100,000 to 1:40,000 still born or live births. It has variable expressivity and generally expressed as orofacial manifestations like lower lip pits, cleft lip and/or cleft palate, hypodontia, cleft or bifid uvula, ankyloglossia and some extraoral anomalies involving hand, foot and genitalia.
Thorough family history, clinical examination and genetic counseling helps in correct diagnosis of VWS as Popliteal pterygium syndrome has overlapping clinical manifestations. Most cases of Van der Woude syndrome have been associated with mutations and genetic changes.
The current case has classical features of VWS with some rare features like undescended small testis and unreported finding of syndactyly of second and third toe adds on to the existing knowledge of VWS presentation.
Lip pits, Popliteal pterygium syndrome, Syndactyly, Van der woude syndrome
Case Report
A 12-year-old male patient reported to the Department of Oral Medicine and Radiology of King George Medical University, Lucknow, India with drainage of fluid from depression on the lower lip since birth. The watery discharge was continuous and was aggravated during eating.
Past surgical history revealed that the patient had undergone surgical correction of upper cleft lip and cleft palate at the age of 10 month. The family history did not reveal consanguineous marriage of his parents. According to his mother, the patient was single child born after a normal, full-term pregnancy with no exposure to radiation. The mother of the patient had bifid uvula but no cleft of lip or palate or any other related abnormality. No history of similar illness could be elicited in the father of the patient and previous two generations of the parents.
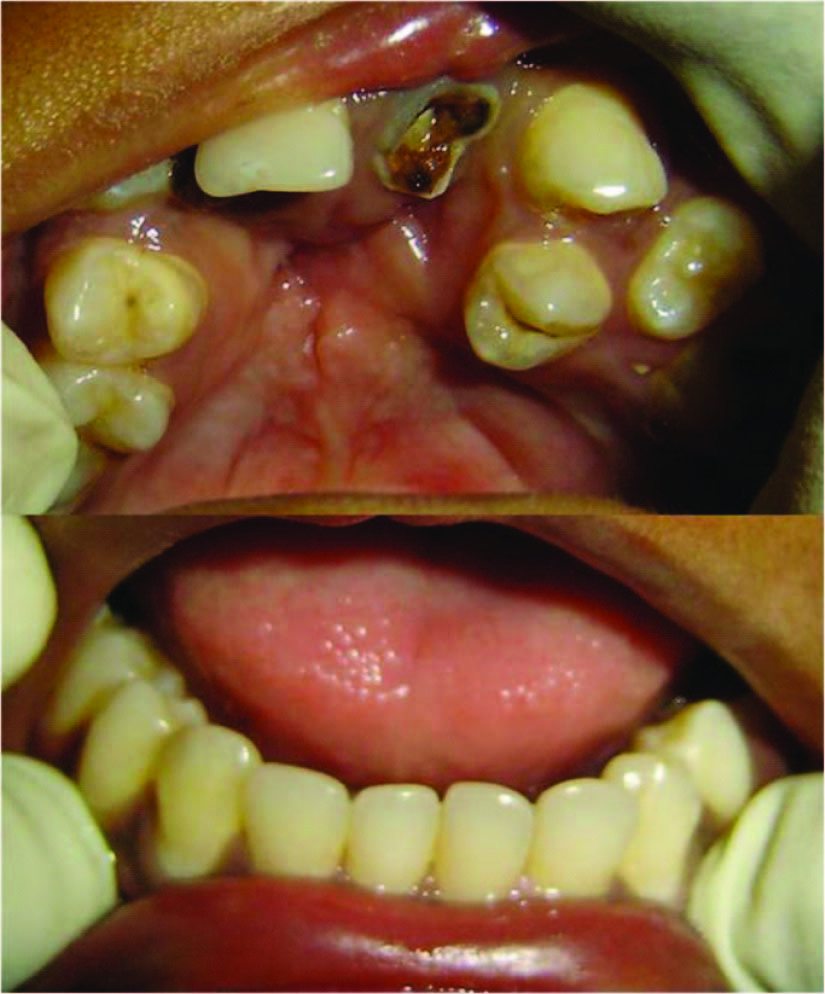
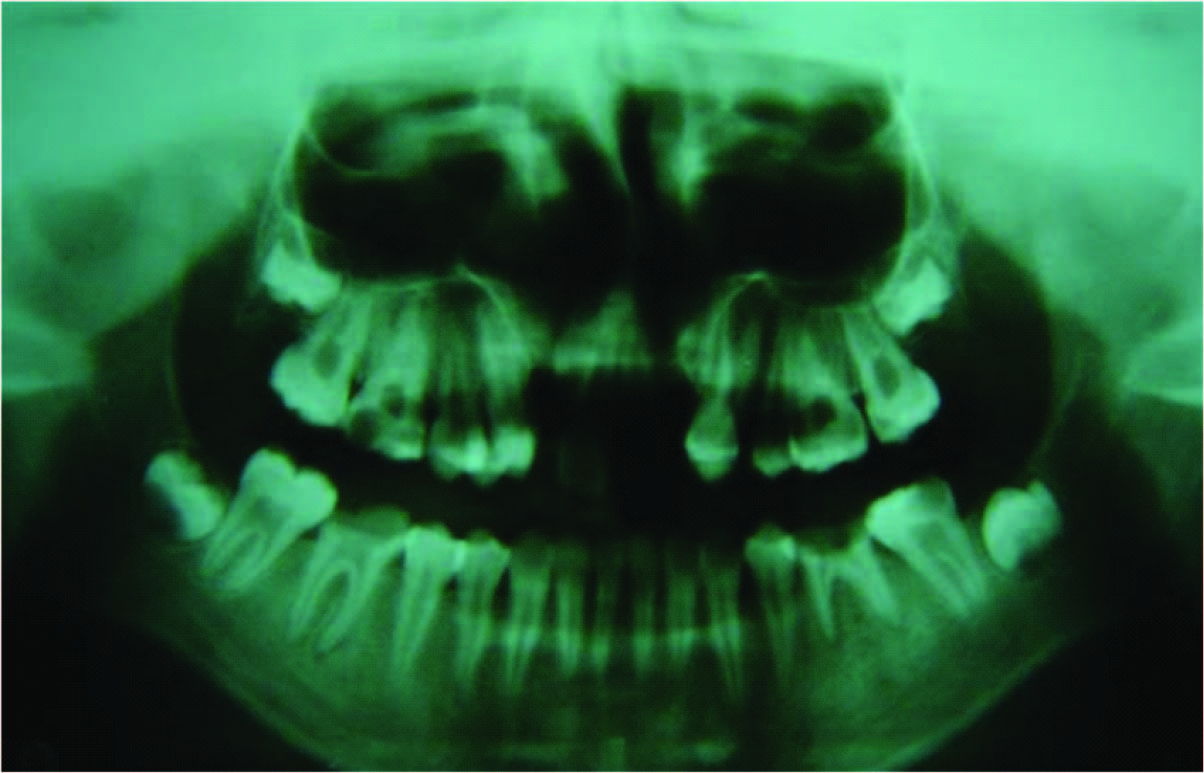
The extraoral examination revealed surgical scar of the upper operated bilateral cleft lip and a median transverse pit on the lower lip filled with watery fluid [Table/Fig-1]. Intraoral examination of soft tissues showed a surgical scar of palatal cleft correction [Table/Fig-2]. Dental examination revealed missing maxillary lateral incisors (hypodontia) and malpositioned teeth (13 and 24) [Table/Fig-2]. An orthopantamograph disclosed bilateral palatal cleft and missing maxillary lateral incisors [Table/Fig-3].
Surgical scar of the upper operated cleft lip and a median transverse pit on the lower lip

Surgical scar of cleft palate correction, missing maxillary lateral incisors (hypodontia) and malpositioned teeth (13and 24)
An orthopantamograph showing bilateral palatal cleft and missing maxillary lateral incisors
On examination the left feet showed complete syndactyly of second and third toe while partial syndactyly of second and third toe was evident in right feet [Table/Fig-4]. No popliteal webbing was noted and the scrotum and testes were absent [Table/Fig-5].
Complete syndactyly of second and third toe in left feet and partial syndactyly of second and third toe of right feet

Absence of popliteal webbing and the scrotum and testicles

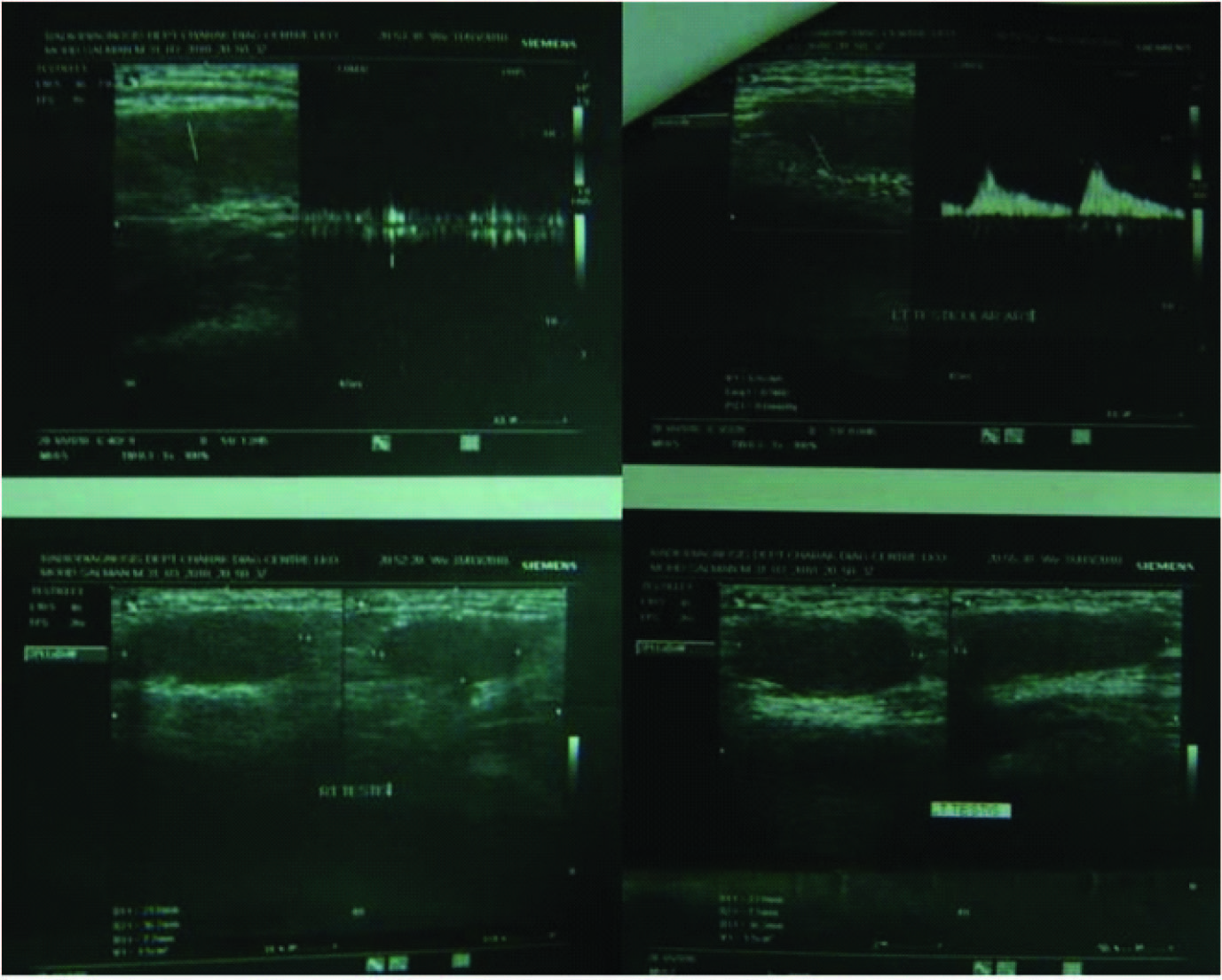
The ultrasonography (USG) of lower abdomen revealed undescended testes located in inguinal canal. The USG and colour Doppler examination further revealed that testes were slightly reduced in volume (1.5 ml each) with normal contour, echotexture and vascularity with no evidence of varicocele on any side [Table/Fig-6]. The clinical diagnosis of VWS syndrome was made on the basis of above findings.
The ultrasonography and Colour Doppler of lower abdomen showing smaller testes with normal contour, echotexture and vascularity with no evidence of varicocele on any side located in inguinal canal
Discussion
The lip pit in VWS can be typical bilateral symmetrical paramedian, single median or unilateral/ bilateral asymmetrical. Single median or paramedian lower lip pit is considered as incomplete expression of syndrome by researchers [1]. In the present case the patient presented with single median lip pit which is less common than classical type. Lip pits are usually round or oval in morphology but sometimes it can be transverse slit like as seen in present case. The conical elevations, the transverse mucosal ridges and/or shallow depth which probably represent microforms of lower lip pits are also reported [2]. In present case the pit is surrounded by fold of mucosa. The lip pits are continuous canal with labial mucosal lining which extended into the orbicularis oris muscle and may have ended in blind fundus or can have minor salivary glands in their inner part [3,4]. This connection with salivary glands is the reason for spontaneous or induced discharges of saliva or mucus from lip pit as noticed in the present case. The other feature of VWS is clefts. Various studies show that the lip pits are associated with clefts in about half of the patients. Among these two thirds have CL or CLP and one third have CP alone [4,5].
For appropriate diagnosis and genetic counseling it is important to differentiate other disease entities from VWS like Aganglionic megacolon combined with CL and lip pits, Popliteal Pterygium Syndrome (PPS), Oro-facial-digital syndrome type I and the Kabuki makeup syndrome [1] which have some features in common. PPS acquires more significance in this aspect as it is considered as an allelic variant of VWS. Besides lower lip pits and oral clefts the PPS show one or many other features like syngnathia, popliteal web, toe nail dysplasia, syndactyly of the toes, congenital heart disease and genital abnormalities [6]. In PPS occurrence of popliteal web is more common as compared to lip pits. Differentiation between VWS and PPS can sometimes be difficult owing to the overlapping phenotype [7]. So cases with VWS should be examined carefully for abnormality of the limbs to rule out PPS.
In current case we noted some rare findings like syndactyly of toes and undescended small testes. To the best of our knowledge congenital deformity of toes and undescended testes is reported by some author [8] but, specifically syndactyly of second and third toe is not yet reported in VWS. However, syndactyly of fingers is also reported by some authors [9]. In this case report we recorded missing maxillary lateral incisors (hypodontia) which is consistent with findings of other researchers [9,10]. In the reported case each testis was undescended and of 1.5 ml volume and hypoplastic while appropriate mean volume of testis for the age is 2.33 ml [11]. Undescended testes can lead to complications like psychological impact, infertility and testicular malignancy [12].
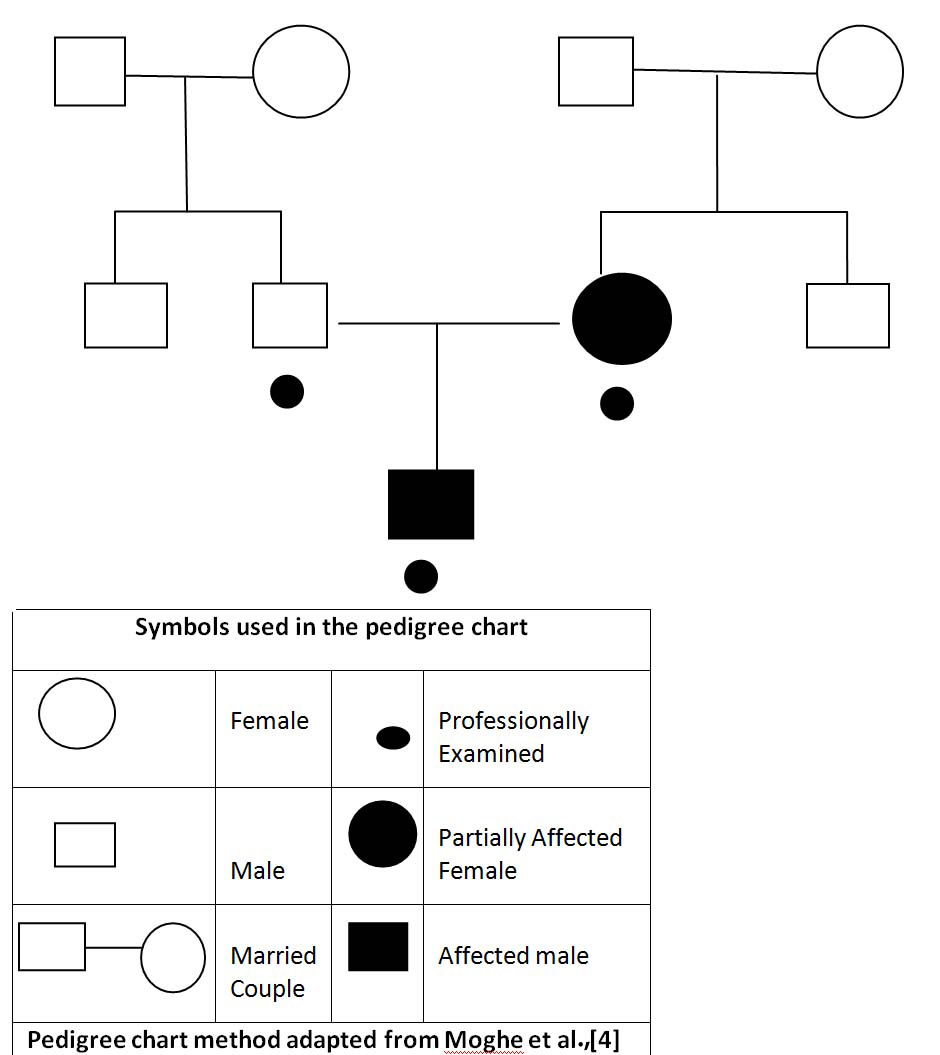
Heredity pattern of VWS is studied by many researchers. It has been reported that an offspring of a parent with lip pit only, has 22% higher risk of developing a cleft and if a parent has cleft only and his/her parent/sibling has lip pit then the risk of clefting in offspring becomes 30% while if the parenthas lip pit and cleft both then the risk of clefting in child increases to 39% [13] [Table/Fig-7].
Pedigree chart of the family studied
In the present case no genetic studies were performed although understanding of genetic pattern of VWS is also important for genetic counseling. The majority of VWS cases are caused by mutations in the interferon regulatory factor 6 genes (IRF6) on chromosome 1 in the 1p32-p41 region known as VWS locus 1. A second, less common, causative locus is found at 1p34, known as VWS locus 2 (VWS2). More recent work has shown that Grhl3 is the VWS2 gene. Grhl3 is downstream of Irf6 in oral epithelium, suggesting a common molecular pathway leading to VWS. IRF6 contains two non-coding and seven coding axons and is part of a family of nine transcription factors with a highly conserved helix-turn-helix DNA binding domain called the Smad-interferon regulatory factor binding domain (SMIR). Mutations in coding or non-coding IRF6 exons can result in Van der Woude syndrome [14].
The treatment of VWS should involve a multispecialty team approach for the correction of lip pits, CL, CLP and other associated anomalies.
Conclusion
Correct diagnosis of incomplete presentation and differential diagnosis of PPS, which has overlapping phenotypic presentation, is important for genetic counseling. A multispecialty approach is essential for physical, physiological and psychological management of the disorder.
[1]. Rizos M, Spyropoulos MN, Van der Woude syndrome: A review. Cardinal signs, epidemiology, associated features, differential diagnosis, expressivity, genetic counseling and treatmentEuropean J Ortho 2004 26:17-24. [Google Scholar]
[2]. Gorlin RJ, Cohen MM, Levis LS, Syndromes of the head and neck 1990 3rd ednNew YorkOxford Press:629-31.:738-40.:745 [Google Scholar]
[3]. Souto LR, Congenital bilateral lower lip pits associated with fistulae of the minor salivary glands: Case report of the principal Van Der Woude syndrome’s TrailAesth Plast Surg 2008 32:172-74. [Google Scholar]
[4]. Moghe GA, Kaur MS, Thomas AM, Raseswari T, Swapna M, Rao L, The role of 9qh+ in phenotypic and genotypic heterogeneity in a Van der Woude syndrome pedigreeJ Indian Soc Pedod Prevent Dent 2010 28:104-09. [Google Scholar]
[5]. Martelli-Junior H, Chaves MR, Swerts MS, de Miranda RT, Bonan PR, Coletta RD, Clinical and genetic features of Van der Woude syndrome in two large families in BrazilCleft Palate Craniofac J 2007 44:239-43. [Google Scholar]
[6]. Lees MM, Winter RM, Sue Malcolm S, Saal HM, Chitty L, Popliteal pterygium syndrome: a clinical study of three families and report of linkage to the Van der Woude syndrome locus on 1q32J Med Genet 1999 36:888-92. [Google Scholar]
[7]. Bixler D, Poland C, Nance W, Phenotypic variation in the popliteal pterygium syndromeClin Genet 1973 4:220-28. [Google Scholar]
[8]. Huang JJ, Hou JW, Tan YC, Chen KT, Lo LJ, Chen YR, Van der Woude syndrome: Clinical presentation in 64 patientsCleft Palate Craniofac J 2007 44:649-52. [Google Scholar]
[9]. Kuster W, Lambrecht JT, Cleft lip and palate, lower lip pits, and limb deficiency defectsJournal of medical genetics 1988 25:565-72. [Google Scholar]
[10]. Schinzel A, Klausler M, The van der Woude syndrome (dominantly inherited lip pits and clefts)J Med Genet 1986 23:291-94. [Google Scholar]
[11]. Goede J, Normative Values for Testicular Volume Measured by Ultrasonography in a Normal Population from Infancy to AdolescenceHorm Res Paediatr 2011 Accessible online at: www.karger.com [Google Scholar]
[12]. Raghavendran M, Mandhani A, Adult cryptorchidism: Unrevealing the cryptic factsIndian J Surg 2004 66:160-63. [Google Scholar]
[13]. Cervenka J, Gorlin Rj Anderson Ve, The syndrome of pits of lower lip and cleft and/or palate. Genetic considerationsAmerican journal of human genetics 1967 19:416-32. [Google Scholar]
[14]. Peyrard-Janvid Dominant mutations in GRHL3 cause Van der Woude syndrome and disrupt oral periderm developmentAm J Hum Genet 2014 94:23-32. [Google Scholar]