During induction of anesthesia and intubation, hemodynamic changes are very important; especially in patients with CAD and left ventricular dysfunction. These patients who presented for CABG surgery are a high-risk group among the cardiac surgical population [1,2]. Laryngoscopy and endotracheal intubation is a standard technique of airway management in general anesthesia for cardiac surgery. This procedure is a noxious stimulus, which can provoke untoward response in the cardiovascular, respiratory and other physiological systems such as tachycardia, hypertension, and arrhythmia which can be deleterious in patients with poor cardiovascular reserve [3]. These hemodynamic changes may alter the delicate balance between myocardial oxygen demand and supply and consequently precipitate myocardial ischemia in patients with CAD [4]. Anesthetic induction techniques in patients with CAD undergoing CABG surgery are usually based on considerations such as minimizing intubation stress response, effects on myocardial oxygen supply and hemodynamic stability [2]. Many studies have been conducted to investigate the effects of wide variety of induction agents such as propofol, thiopental, midazolam, fentanyl and ketamine, on these hemodynamic changes [2, 5, 6].
Etomidate, which is an imidazole derivative and an ester, is the most commonly used anesthetic induction agent and characterized by rapid onset, with minimal side effects on cardiovascular and respiratory functions, as well as minimum histamine release. These properties make it especially useful for cardiac-compromised patients [7]. However, it has been shown that single bolus of etomidate, blunts the hypothalamic–pituitary–adrenal (HPA) axis response for more than 24 hour after operation in patients undergoing elective cardiac surgery [8]. Activation of HPA axis is an essential component of the general adaptation to illness and stress and contributes to the maintenance of cellular and organ homeostasis. Some studies suggest an association between etomidate administration, adrenal insufficiency (caused by reversible inhibition of cortisol synthesis), and increased mortality [8,9]. On the other hand, it has been shown that relative adrenal insufficiency in elective cardiopulmonary bypass (CPB) surgery patients may induce postoperative vasopressor dependency [9].
Ketamine is a fast-acting dissociative anesthetic agent. It has unique cardiovascular effects; it stimulates the cardiovascular system and is usually associated with increases in blood pressure, heart rate, and cardiac output. These stimulating effects may be blunted by reducing the dose or combination of ketamine with benzodiazepines [10]. Thiopental is a barbiturate that is widely used for the induction of anesthesia and can causes a dose-dependent reduction in cardiac output, stroke volume and systemic vascular resistance which associated with a compensatory tachycardia [10]. In theory, the opposing hemodynamic effects of these two drugs (ketamine and thiopental), might be complementary and minimize overall adverse effects. In balanced anesthesia, a mixture of small amounts of several anesthetic drugs concurrently administrated, which summates the advantages, but not the disadvantages of the individual components of the mixture [11]. Considering the concept of balanced anesthesia and also, a little information available on the hemodynamic effects of a combination of ketamine-thiopental in patients undergoing CABG surgery, with impaired ventricular function, this study was conducted to compare the hemodynamic responses to etomidate versus ketamine-thiopental sodium combination for anesthetic induction in CABG surgery patients with low EF.
Materials and Methods
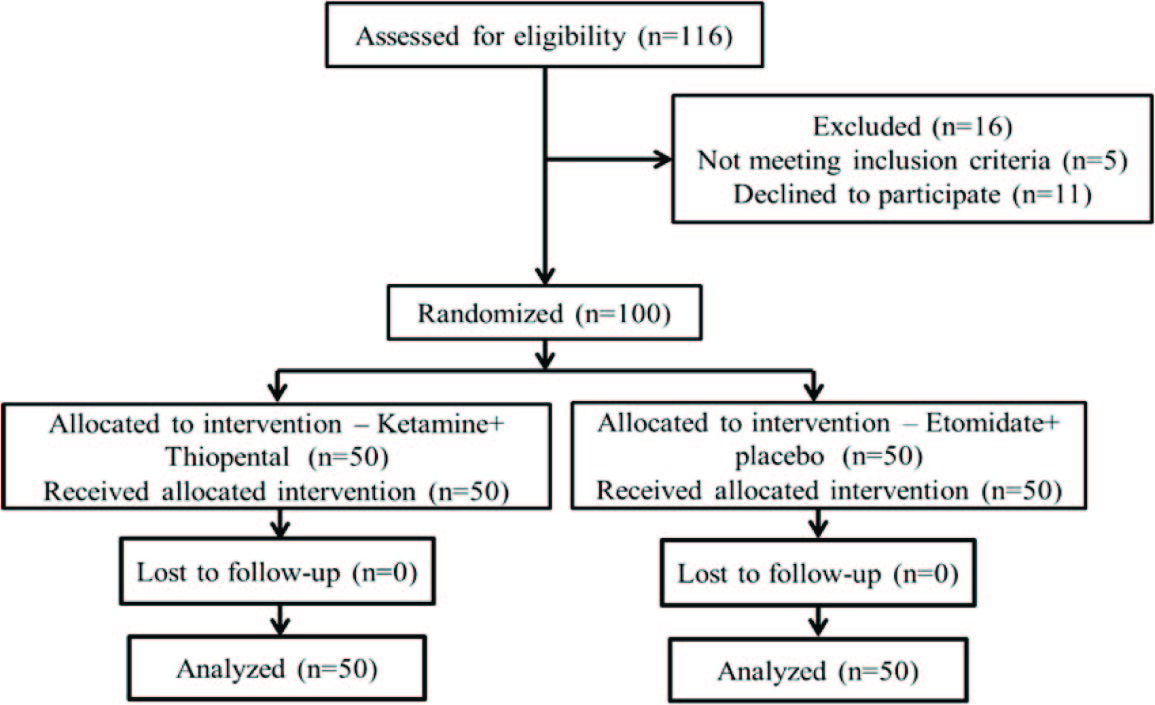
After approval from the institutional ethics committee and written informed consent from the patients, a total of 100 patients of both sexes, aged 40 – 75 years, with CAD and left ventricular dysfunction (EF < 45%) [2], scheduled for elective CABG surgery with CPB, were included in this double blind randomized, clinical study.
Exclusion criteria included known adrenal insufficiency, chronic inflammatory diseases, history of steroid use in the preceding six months, use of etomidate or thiopental within one week preoperatively, known sensitivity to thiopental or etomidate, serious psychiatric, endocrine or neurological illnesses, tracheal intubation time more than 30 seconds, sepsis, endocarditis, combined cardiac valve surgery with CABG and Bentall surgery. The study was performed from August 2012 to September 2013 in the cardiac surgery unit and the open heart intensive care unit (ICU) of a teaching hospital affiliated to Mazandaran University of Medical Sciences, Sari, Iran.
Patients who meet the inclusion criteria were randomly allocated to group A and group B (50 patients in each group) by the sealed envelope technique. Patient allocation was performed by a nurse who was unaware of the study groups, according to numbers generated by the computer generated list. In the operating room and before induction of anesthesia, 5 cc/kg Ringer lactate were infused for all patients via an intravenous line.
Also electrocardiogram, invasive arterial blood pressure, and pulse oximeter were applied for all patients and baseline systolic and diastolic arterial blood pressure (SAP, DAP), mean arterial pressure (MAP) and heart rate (HR) were measured and recorded for all of them.
Then all patients received fentanyl (2μg/kg) and midazolam (0.03 mg/kg) intravenously as premedication. One minute later, patients in group A were induced with ketamine 1mg/kg and thiopental sodium 3 mg/kg and group B, was induced with etomidate 0.2mg/kg and also placebo (normal saline). Considering that in group A, ketamine and Thiopental were prepared in two separate syringes and then administered separately for induction, so we use a syringe containing etomidate and another syringe which contained normal saline as a placebo for group B. All syringes were covered with masking tape to conceal any details of product. The end point of anesthesia induction was loss of eyelash reflex. Then, all patients received 1.5 mg/kg succinylcholine for muscle relaxation to facilitate intubation. One minute after succinylcholine administration, tracheal intubation was performed. Hemodynamic variables including SAP, DAP, MAP and HR were measured immediately before and after laryngoscopy and intubation, one, two and three minutes after intubation. Laryngoscopy and anesthesia administration was done by an anesthesiologist who was blinded to the study groups. The duration of laryngoscopy and intubation were recorded for each patient. If the blood pressure decreased to less than 20% of patient’s baseline, ephedrine (10 mg) was administered and then recorded. Also, occurrence of muscle twitching was recorded by a trained research nurses who was unaware of the study groups. This study registered in the Iranian Registry of Clinical Trials Database (IRCT201309242883N4).
The primary study endpoint was comparison of hemodynamics changes between the two groups. Also, the secondary endpoints were comparison of muscle twitching incidence between two groups. A power analysis from previous studies showed a sample size of 45 patients in each group was necessary to achieve 80% power at significance level of α=.05 for detection of anticipated changes in hemodynamic parameters (20 mmHg or 20 beats/minute in systolic blood pressure or HR respectively). We therefore recruited 100 patients to account for any dropouts.
Statistical Analysis
All statistical procedures were performed with SPSS 16 statistical software (SPSS Inc., Chicago, IL). Descriptive statistics were used to characterize the basic data of the sample. Differences between the two groups on demographical and clinical details were assessed using Chi-square tests (%) and two-sample Student’s t-test (with assuming equal variances) for qualitative and quantitative variables. A repeated-measures analysis of variance was performed to compare the effects of each of the two drugs to assess variety of pulse rate, blood pressure, and MAP. The assumption of sphericity was checked using Mauchly’s test. A two-way ANOVA was performed to determine if there is a difference in EF for interaction gender to groups. Statistical significance was set at p < 0.05.
Results
All 100 patients completed the present study and data from all patients were analyzed [Table/Fig-1]. There was no statistically significant difference between the two groups with regard demographic characteristics (p > 0.05) [Table/Fig-2].
Demographic characteristics of patients in the two groups
| Variable | | All subjects (N=100) | Ketamine+ thiopental (N=50) | Etomidate+ placebo (N=50) | p-value |
|---|
| Age (years) | Mean (SD) Range | 61.17 (8.18) 43-74 | 59.82 (7.72) 43-65 | 62.52(8.49) 45-74 | 0.091 |
| Gender | Male Female | 64 36 | 29(58.00) 21(42.00) | 35(70.00) 15(30.00) | 0.211 |
| BMI (Kg/m2) | | 24.2±2.8 | 24.3±2.5 | 23.9±3.4 | 0.19 |
Data are expressed as the mean ± standard deviation, Statistical significance was set at p < 0.05
A repeated measurement ANOVA, with Greenhouse-Geisser correction, have been shown that there were no statistically significant changes in HR, MAP, SAP and DAP at any time in two groups [Table/Fig-3,4,5and6].
Adjusted heart rate in six measurements in the two groups
| Group Heart Rate | Ketamine+ thiopental Mean (SD) | Etomidate+ placebo Mean (SD) |
|---|
| Baseline | 77.64(15.34) | 73.94(14.07) |
| Immediately before laryngoscopy and intubation | 74.38(14.44) | 70.82(10.92) |
| Immediately after laryngoscopy and intubation | 81.86(16.46) | 79.60(13.61) |
| One minute after intubation | 81.66(15.98) | 79.84(1313) |
| Two minutes after intubation | 79.82(15.44) | 77.06(13.01) |
| Three minutes after intubation | 77.94(16.32) | 74.22(12.69) |
F (3.37, 320.78) = 0.833, p= .488, eta2 = .009, Adjusted for: Age, Gender, Ejection fraction
Adjusted MAP in six measurements in the two groups
| Group MAP | Ketamine± thiopental Mean (SD) | Etomidate± placebo Mean (SD) |
|---|
| Baseline | 97.64±21.68 | 92.36±15.15 |
| Immediately before laryngoscopy and intubation | 68.38±13.65 | 69.40±15.03 |
| Immediately after laryngoscopy and intubation | 92.86±25.38 | 94.42±24.97 |
| One minute after intubation | 92.66±22.92 | 97.66±24.59 |
| Two minutes after intubation | 91.82±20.82 | 92.22±21.77 |
| Three minutes after intubation | 87.94±19.71 | 88.44±19.20 |
F (3.44, 327.07) = 1.325, p= .264, eta2 = .014., Adjusted for: Age, Gender, Ejection fraction
Adjusted systolic arterial blood pressure in six measurements in the two groups
| Group Systolic arterial blood pressure | Ketamine± thiopental Mean (SD) | Etomidate± placebo Mean (SD) |
|---|
| Baseline | 140.22±27.35 | 136.48±21.67 |
| Immediately before laryngoscopy and intubation | 95.60±18.86 | 96.20±20.43 |
| Immediately after laryngoscopy and intubation | 123.84±29.22 | 128.84±38.49 |
| One minute after intubation | 128.96±30.94 | 132.96±32.43 |
| Two minutes after intubation | 127.16±27.02 | 130.30±27.49 |
| Three minutes after intubation | 119.98±25.68 | 126.36±25.42 |
F (3.28, 312.26) = 0.537, p= .674, eta2 = .006., Adjusted for: Age, Gender, Ejection fraction
Adjusted diastolic arterial blood pressure in six measurements in the two groups
| Group Diastolic arterial blood pressure | Ketamine± thiopental Mean (SD) | Etomidate± placebo Mean (SD) |
|---|
| Baseline | 70.08±12.58 | 66.28±12.21 |
| Immediately before laryngoscopy and intubation | 53.74±13.40 | 52.92±14.74 |
| Immediately after laryngoscopy and intubation | 69.36±16.32 | 72.38±19.83 |
| One minute after intubation | 70.40±16.39 | 71.18±19.21 |
| Two minutes after intubation | 70.74±16.84 | 70.76±16.77 |
| Three minutes after intubation | 67.92±15.70 | 67.28±15.52 |
F (3.65, 347.56) = 0.696, p= .582, eta2 = .007., Adjusted for: Age, Gender, Ejection fraction
According to the two-way ANOVA test, there was no difference between the interactions of gender with two groups on EF [Table/Fig-7]. Since there was no significant interaction, we tested main effects. Main effect for gender was not significant F (1, 96) = 0.427, p = 0.515).
Adjusted ejection fraction between the interactions of gender with two groups
| Group | Gender(n) | Mean±(SD) |
|---|
| Ketamine+ thiopental | Female(21) | 41.24±3.34 |
| Male(29) | 42.16±1.25 |
| Etomidate+ placebo | Female(15) | 42.12±2.21 |
| Male(35) | 40.92±2.45 |
F(1,96)=0.427, p=.515, Adjusted for: Age
Muscle twitching was not observed in the two groups.
Discussion
We evaluate the influence of the administration of etomidate versus ketamine-thiopental sodium combination on hemodynamic variables at baseline, immediately before and after laryngoscopy and intubation and also one, two and three minutes after orotracheal intubation in patients undergoing CABG surgery with left ventricular dysfunction. The major finding of this study was that the differences in hemodynamic responses to etomidate versus ketamine-thiopental sodium combination for anesthetic induction in these patients were not statistically significant between two groups. In a study by Dehghani Firoozabadi et al., [12] with aim to evaluate the effect of the combination of ketamine and thiopental on hemodynamic changes during intubation in patient’s undergoing cesarean section with general anesthesia showed that combination of ketamine with thiopental can create better hemodynamic stability in patients after tracheal intubation which is inline with the result of our study. During CABG surgery, induction of general anesthesia may be a critical period especially in patients with low EF [2]. Hemodynamic changes due to anesthesia in various surgeries have become a great concern in anesthesiologists and evidence show that changes in blood pressure, either decrease or increase, independently are associated with side effects and complications in patients undergoing surgery [13]. In patients undergoing CABG surgery, cardiovascular stability is an important prerequisite for any anesthetic agent used for induction [14]. In our study before laryngoscopy, all patients had a reduction in SAP, DAP, MAP as well as in HR after drug injection, whereas all these variables increased after laryngoscopy and endotracheal intubation. The effects of this increase gradually disappeared within three minutes after intubation which is consistent with the results of the study by Lahsaee and colleagues’ that is conducted on candidates of elective surgery [15]. In our study although all of the hemodynamic variables increased after laryngoscopy and endotracheal intubation in two groups, but the increase in MAP, SAP and DAP after laryngoscopy and endotracheal intubation in group A (who received ketamine-thiopental sodium combination) was not as high as the changes of these variables in group B (who received etomidate).
Laryngoscopy and endotracheal intubation can cause sympathetic stimulation which often leads to an increase in systolic and diastolic blood pressures and HR. Thus, anesthesiologists have been trying to use a variety of induction modalities to minimize these hemodynamic changes [15,16]. A wide variety of anesthetic medications and strategy are available for induction of anesthesia in cardiac surgical patients; hypnotics, opioids and volatile anesthetics are used in different combinations for both the induction and maintenance of anesthesia [17]. Several studies have been conducted in this regard, and various anesthetic medications and their combinations have been proposed.
In a study by Pandey et al., [18] with the aim to compare the effects of propofol and etomidate induction on hemodynamic parameters and serum cortisol levels in patients with normal left ventricular function undergoing elective CABG surgery on CPB, have been demonstrated that etomidate provides more stable hemodynamic parameters when used for induction of anesthesia as compared to propofol. Although, etomidate routinely used for the induction of anesthesia for cardiac surgery including CABG and has least side effects on cardiovascular and respiratory functions, as well as minimum histamine release, especially for cardiac-compromised patients, [7] but several studies suggest an association between etomidate administration, adrenal insufficiency and increased mortality in patients undergoing cardiac surgery [8,9]. Etomidate suppresses cortisol synthesis in the adrenal cortex by reversibly inhibiting 11-beta-hydroxylase, an enzyme important in adrenal steroid production, leading to primary adrenal suppression [19]. Etomidate blunts the HPA axis responses. Activation of HPA axis is an essential component of the general adaptation to illness and stress and contributes to the maintenance of cellular and organ homeostasis which [8].
In a cohort study by Iribarren et al., [9] with aim to determine the risk factors for relative adrenal insufficiency in 120 CPB patients and the impact on postoperative vasopressor requirements, the results have been shown that 77.5% of patients who received etomidate during anesthetic induction developed relative adrenal insufficiency. They concluded that relative adrenal insufficiency in elective CPB patients may induce postoperative vasopressor dependency, and stated that the use of etomidate in these patients is a modifiable risk factor for the development of relative adrenal insufficiency that should be avoided. In another study that conducted by Morel et al., [8] with aim to compare norepinephrine usage over the first 48 h after elective cardiac surgery with CPB after a single dose of either etomidate or propofol administered for induction of anesthesia, the results have been shown that a single bolus of etomidate blunts the HPA axis response for more than 24 hour in these patients, but this was not associated with an increase in vasopressor requirements. They concluded that due to its significant inhibition of the HPA axis, etomidate should be used with caution in high-risk cardiac surgical patients.
Several studies have examined the effect of other anesthetic drugs or combinations for induction of anesthesia such as thiopental, ketamine and etc. on the changes of hemodynamic variables. Basagan-Mogol et al., [5] in a study with aim to evaluate the hemodynamic and analgesic effects of ketamine by comparing it with propofol starting at the induction of anesthesia until the end of sternotomy in patients undergoing CABG surgery have been shown that in these patients, there were significant changes in the measured and calculated hemodynamic variables when compared to their values before induction. One minute after induction, MAP and the systemic vascular resistance (SVR) index decreased significantly in patients who received propofol and the combination of ketamine, midazolam and fentanyl for the induction of anesthesia provided better hemodynamic stability during induction and until the end of sternotomy. In another study by Nayar et al. [20] aims to evaluate the benefit of a combination of thiopental and ketamine over either of these drugs alone as an induction agent for Cesarean section, showed that in patients who received thiopental (group 1) or ketamine (group 2) alone at intubation, HR increased and decreased respectively. But in patients who received thiopental and ketamine combination (group 3), no changes of HR have been occurred. These intergroup variations were statistically significant. Also, post induction values of systolic blood pressure (BP) were significantly higher for patients who received ketamine alone. Although after induction, diastolic BP increased significantly in all groups but in group 1 and 3, these values returned to baseline after 10 minutes and in Group 2 at the 30 minutes post induction stage. It should be noted that in balanced anesthesia, a mixture of small amounts of several anesthetics drugs administrated concurrently, which summates the advantages, but not the disadvantages of the individual components of the mixture [11]. Ketamine as an anesthetic agent stimulates the cardiovascular system and is usually associated with increases in BP, HR, and cardiac output. On the other hand, thiopental is a barbiturate that is widely used for the induction of anesthesia and can causes a dose-dependent reduction in cardiac output, stroke volume and SVR, associated with a compensatory tachycardia [10,11]. Considering that the opposing hemodynamic effects of these two drugs (ketamine and thiopental), the combination of these drug might be complementary and minimize overall adverse effects.
A limitation of this study was that even though two groups were given the same premedication with fentanyl (2μg/kg) and midazolam (0.03 mg/kg), the dosages per kilogram body weight may be unequally distributed between groups, and thus the dosing of these premedication drugs may be a confounding variable.
Conclusion
In conclusion, our study found no difference in hemodynamic variable such as SAP, DAP, MAP and HR after induction of anesthesia and intubation with etomidate versus ketamine-thiopental sodium combination between two groups. Due to these results we can consider the combination of ketamine and thiopental for anesthetic induction in CABG surgery patients with low EF.
Data are expressed as the mean ± standard deviation, Statistical significance was set at p < 0.05
F (3.37, 320.78) = 0.833, p= .488, eta2 = .009, Adjusted for: Age, Gender, Ejection fraction
F (3.44, 327.07) = 1.325, p= .264, eta2 = .014., Adjusted for: Age, Gender, Ejection fraction
F (3.28, 312.26) = 0.537, p= .674, eta2 = .006., Adjusted for: Age, Gender, Ejection fraction
F (3.65, 347.56) = 0.696, p= .582, eta2 = .007., Adjusted for: Age, Gender, Ejection fraction
F(1,96)=0.427, p=.515, Adjusted for: Age