Introduction
Morbidity related to hypertrophic scars and contractures which are well known sequelae after burns remains high and in fact has increased as more severely burned patients are surviving. The goal in management is to restore the function and form of the origin.
Post burn neck contractures not only affect the movements of the neck, but also can affect the function of the lower face as well as result in possible tracheal alteration and distortion of the cervical spine. As these contractures cause major functional and cosmetic problems with resultant economic and psychosocial implications, operative correction is generally recommended, particularly in children in whom they can cause growth imbalance in the head and neck area.
The objectives of surgical intervention are releasing the scar, restoring cervical movements, appearance and natural profile and avoiding recurrence of contracture.
This study was undertaken in order to assess the varied clinical presentation, precipitating factors, preventive measures, treatment modalities of neck contractures and evaluate the results after surgical procedures.
Materials and Methods
This hospital based study was conducted on patients admitted in our institution with proven cases of Post burn neck contracture from 1st August 2009 to 31st July 2011. Twenty two patients of post burn neck contracture who underwent operative treatment were included.
Inclusion Criteria
a) Proven cases of post burn neck contracture
b) Both males & females were taken in this study
c) Patients of all age group were included.
Exclusion Criteria
a) Patients who had been operated at other places for neck contracture release came with re-contracture at same site
b) Infected cases of post burn neck contracture
c) Patients with sinus and fistula formation over neck contracture.
Preliminary recording of patient particulars, a brief relevant history and details of the burn injury were taken along with clinical examination.
Local examination
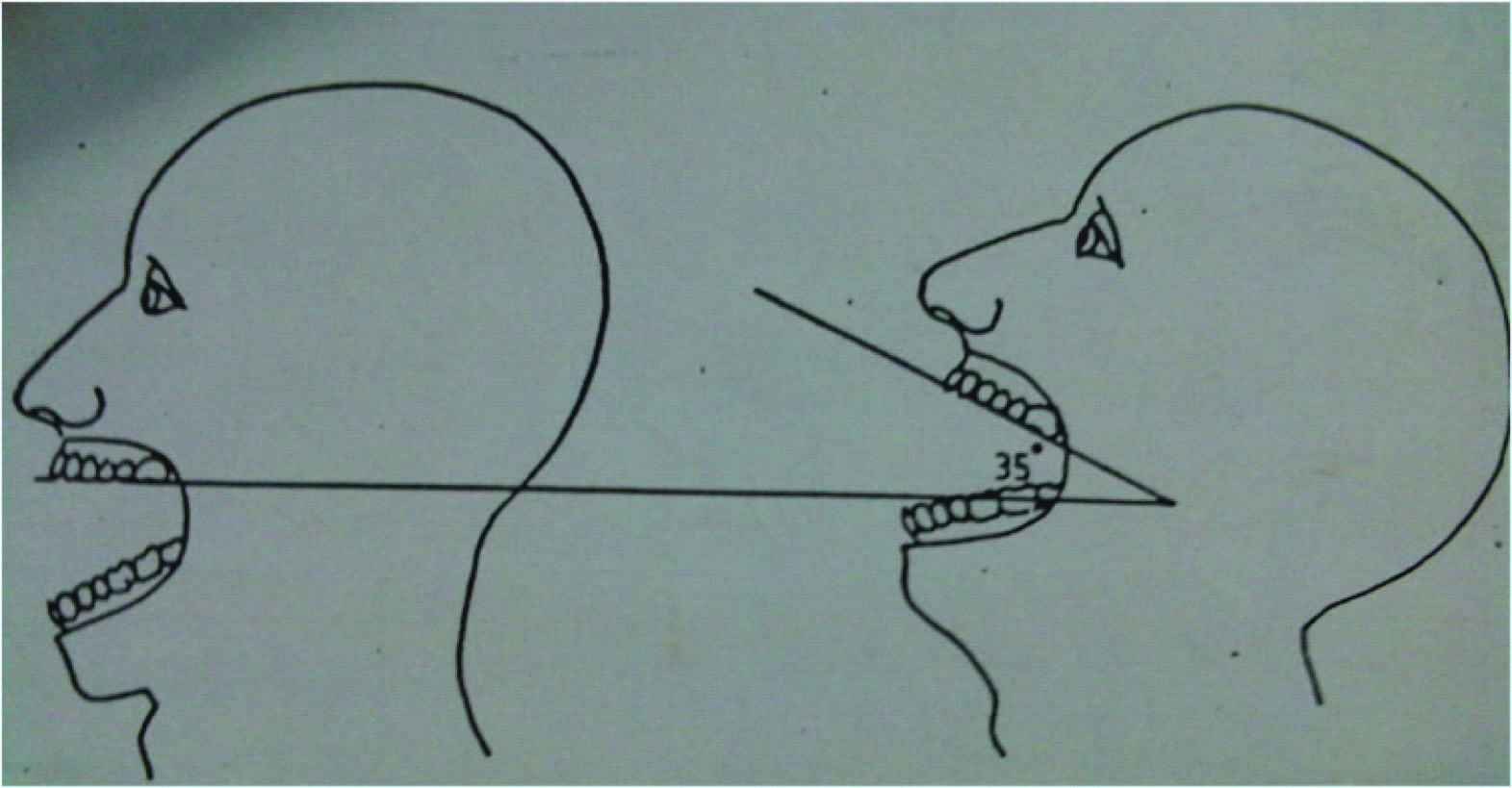
This included extent of contracture as per classification of Achauer [1] and Salisbury/Bevin [2] , [Table/Fig-1,2], range of neck movement, skin texture, colour match and contour. Evaluation of atlanto-occipital extension was performed by having the patient sit straight with head held erect and facing directly to the front as described by Bellhouse and Dore [3] [Table/Fig-3].
Surgical planning
The lines of contracture and proposed incisions were marked on the patient pre-operatively. To calculate the amount of soft tissue coverage required bony prominences such as the mental tubercle, sternal notch, midpoint of the clavicle, mandibular angle etc. were selected as reference points. The vertical extent is calculated by measuring the mentosternal distance. Then the reference points on each side were connected by a line and the horizontal measurement was made across these lines at the level of the seventh cervical vertebrae. The raw area following release was estimated by comparing these distances with those between similar points marked on another individual of approximately the same height and stature. In general, the technically most feasible operation was favoured if functional and aesthetic results were good and post-operative risks for recurrent mentosternal contractures are low.
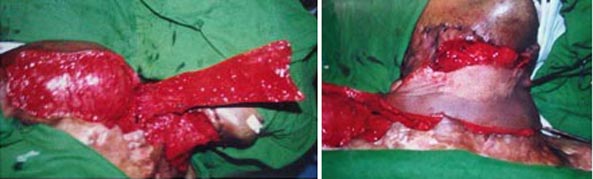
Operative procedures [Table/Fig-4,5,6]: Incisional or excisional release was done till full extension was obtained and the defect was created by dissection through the scar to underlying normal tissue [Table/Fig-7]. Skin graft was the mainstay of treatment. It was applied immediately and held in position with sutures and tie-overs while the neck was immobilised with a bulky dressing. When the local or adjacent skin was unscarred, resurfacing was done with a flap alone or in combination with a graft.
Post-operative management
Patients were nursed in supine position. If a flap was used its temperature, colour and capillary blanching time were monitored and appropriate measures taken as necessary, in case of doubtful vascularity. In grafted patients, the neck was maintained in extension with a shoulder support. A small rolled towel or a blanket was placed transversely beneath the neck. The dressing was changed 5-7 days after surgery. At the next dressing, if the graft was well settled, local lubricating creams were advised and a customised neck collar (for 6 months) [Table/Fig-8,9,10] and chin neck pressure strap was given. In case of graft loss, the area was resurfaced with autograft or dressed regularly. As soon as the grafts were adherent i.e. after 2-3 wks, an active and resistive dynamic and static self exercise program was begun. Extension was the primary exercise performed besides alternate flexion, lateral rotation, and flexion on both sides and circumduction. Physiotherapy was commenced in the early post operative period i.e. within a day or two, when flaps were used for resurfacing.
Discharge
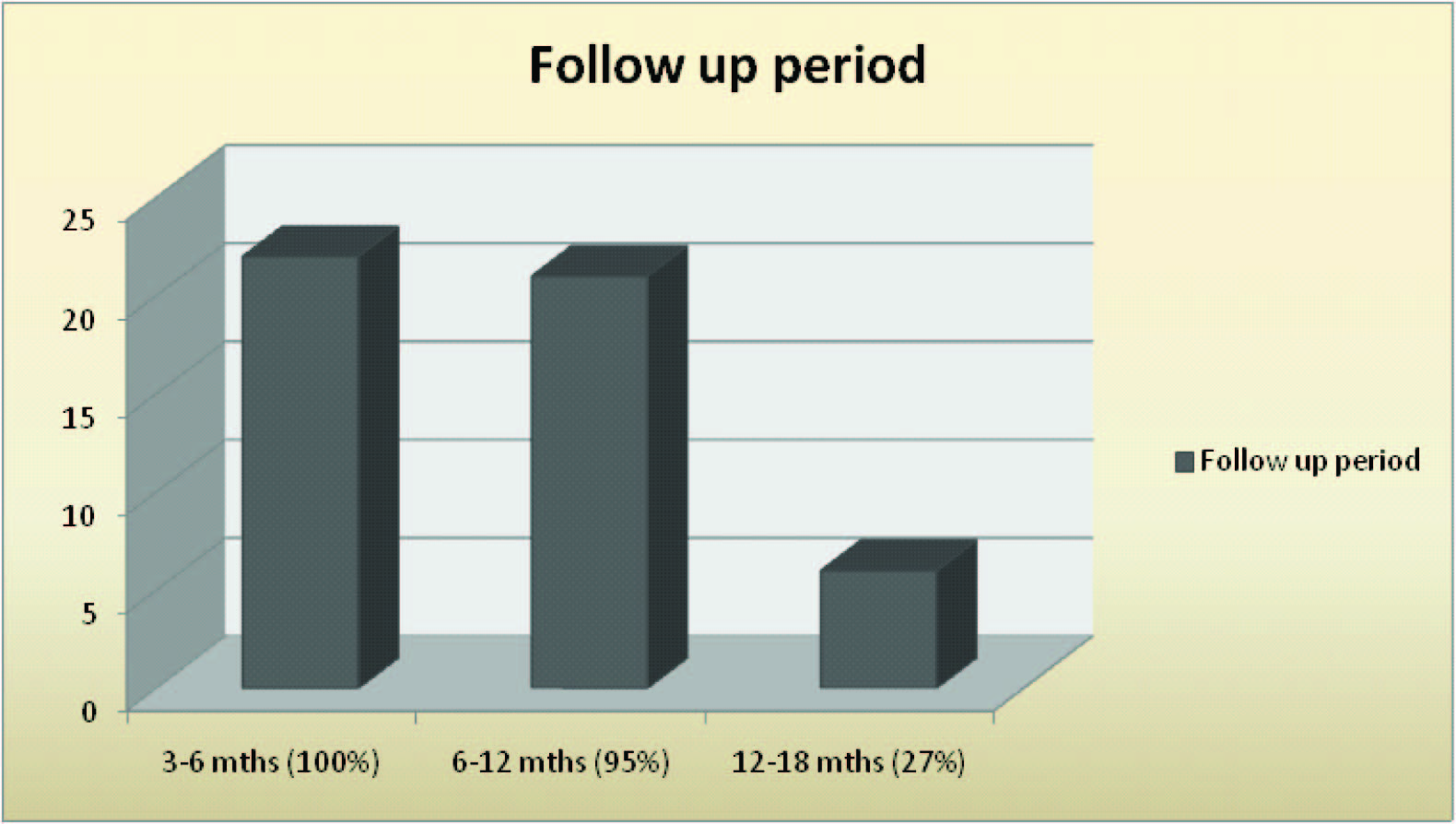
The range of movement and condition of the recipient and donor sites were recorded. Instructions regarding position, splintage / pressure strap, local care and physical therapy were given. The patient was then asked to attend the outpatient department regularly. During this period the results were evaluated with respect to range of extension, overall cosmetic appearance i.e. colour match, flap texture, maintenance of contour and donor site morbidity. The results were assessed graded in the follow up period.
Results
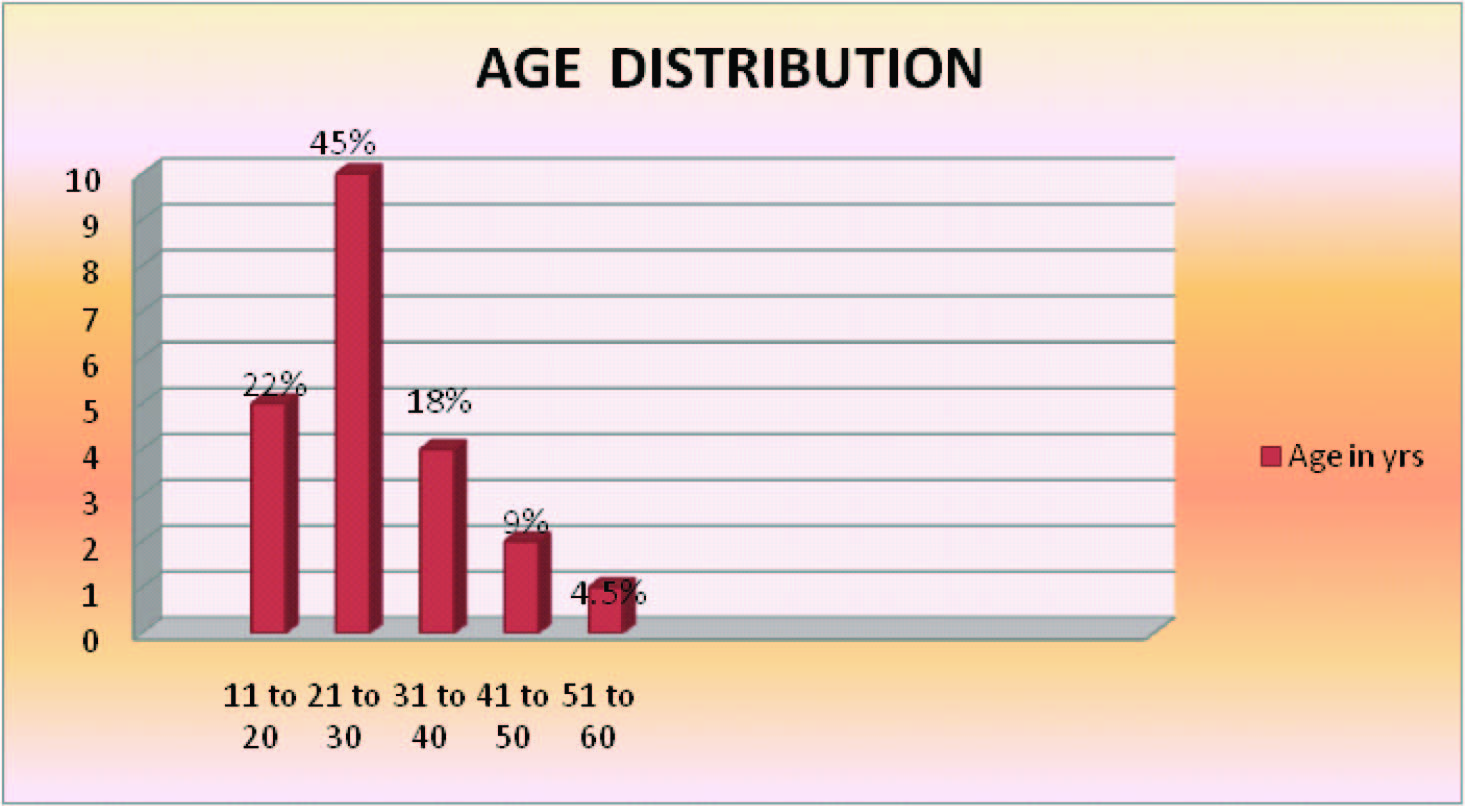
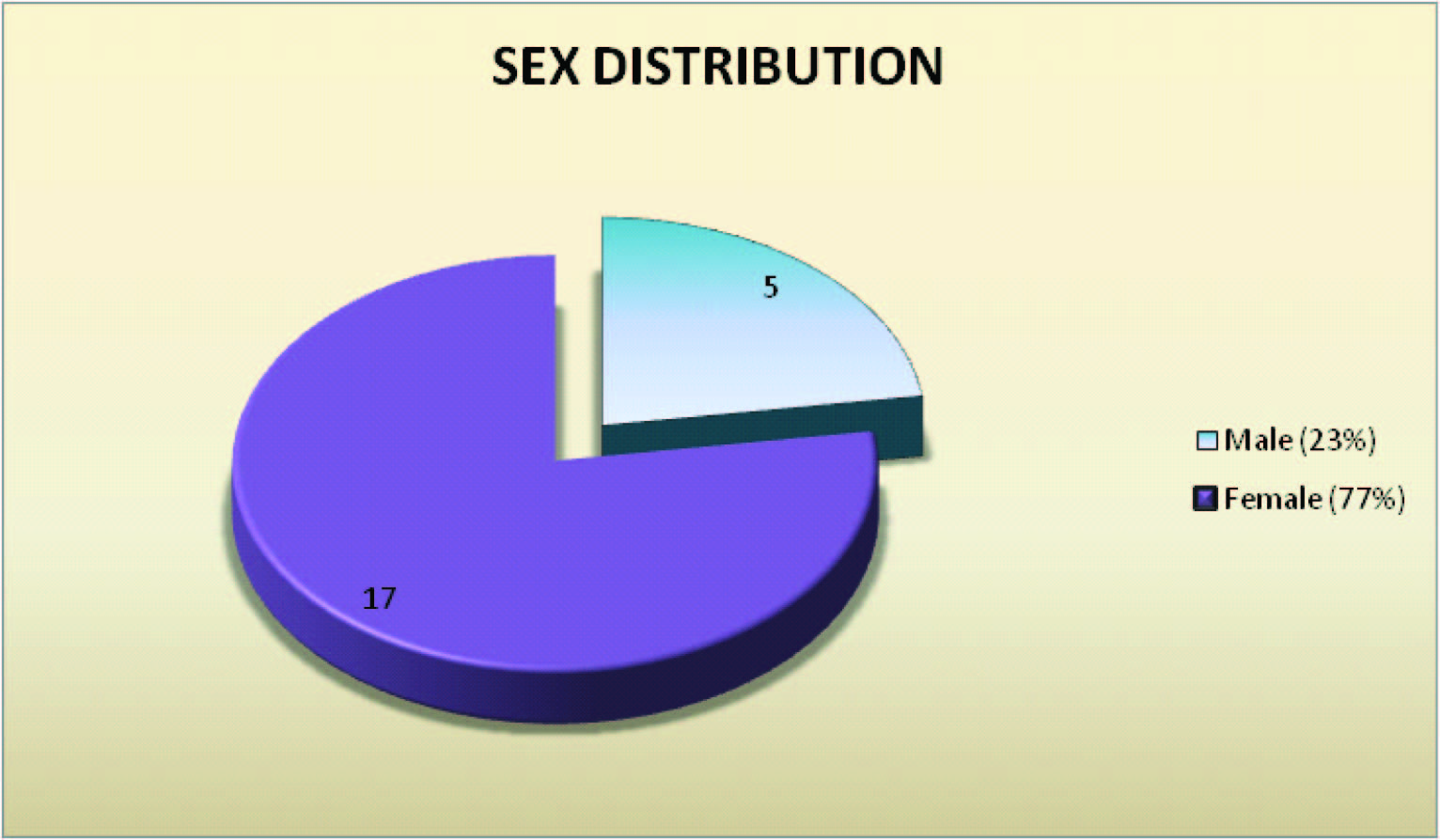
[Table/Fig-11,12,13,14,15,16,17,18,19,20,21,22]
Discussion
Agni or fire is supposed to be foremost among the ancient Aryan Gods. It was also supposed to be ‘Vahak Devta’ which used to convey the offering of Yagnya to the respective Gods. However, Contractures and hypertrophic scars are two frustrating sequel of thermal injury. Scars of the anterior cervical region are prone to be unusually severe because:
1. Its skin is rather loose, thin and thus easily destroyed
2. The area from chin to the sternum is a concave flexor surface.
3. The extreme mobility of the neck makes it prone to contracture formation.
4. Vertical incisions in the skin of the anterior cervical area, whether accidental or surgical, are likely to result in contracted scar bands.
Other than burn scar and contracture these patients are completely flaphealthy and successful reconstructive surgery can often restore them to happy and productive life. Patience, persistence, determination are essential to accomplish successful reconstruction. The ultimate principle of reconstruction of post burn neck contracture is learning to understand, appreciate and favourably influence the process of wound healing & scar maturation.
A total of 22 patients with post burn neck contracture were managed in this study. 45.5% of our patients were in the 21-30 year age group. The youngest patient was 13 years and the oldest was 53 with a mean age of 28.2 years [Table/Fig-11]. The mean age of C. Angrigiani’s [4] 86 patients who were treated with a free extended scapular flap was 28.3 years. Saygin Abdul Kadir Mohd et al., [5] treated 18 patients with the ages ranging from 8 to 45 years with an average of 23 years. S. Bhattacharya [6] managed 28 patients and their age ranged from 12 to 43 with an average of 21.2 years.
Females accounted for 77.3% of patients in our study [Table/Fig-12]. 78.5% of Bhattacharya’s [6] cases were females. Similar observations were made by M.Farid Moustafa [7] (66.3%) who treated 264 patients and Jain [8] (64%) who studied 50 cases with severe contracture. Ahuja [9]also, in his review of the management of burns in developing world found that females are more prone suggesting that the domestic pattern of life has an important bearing on the problem.
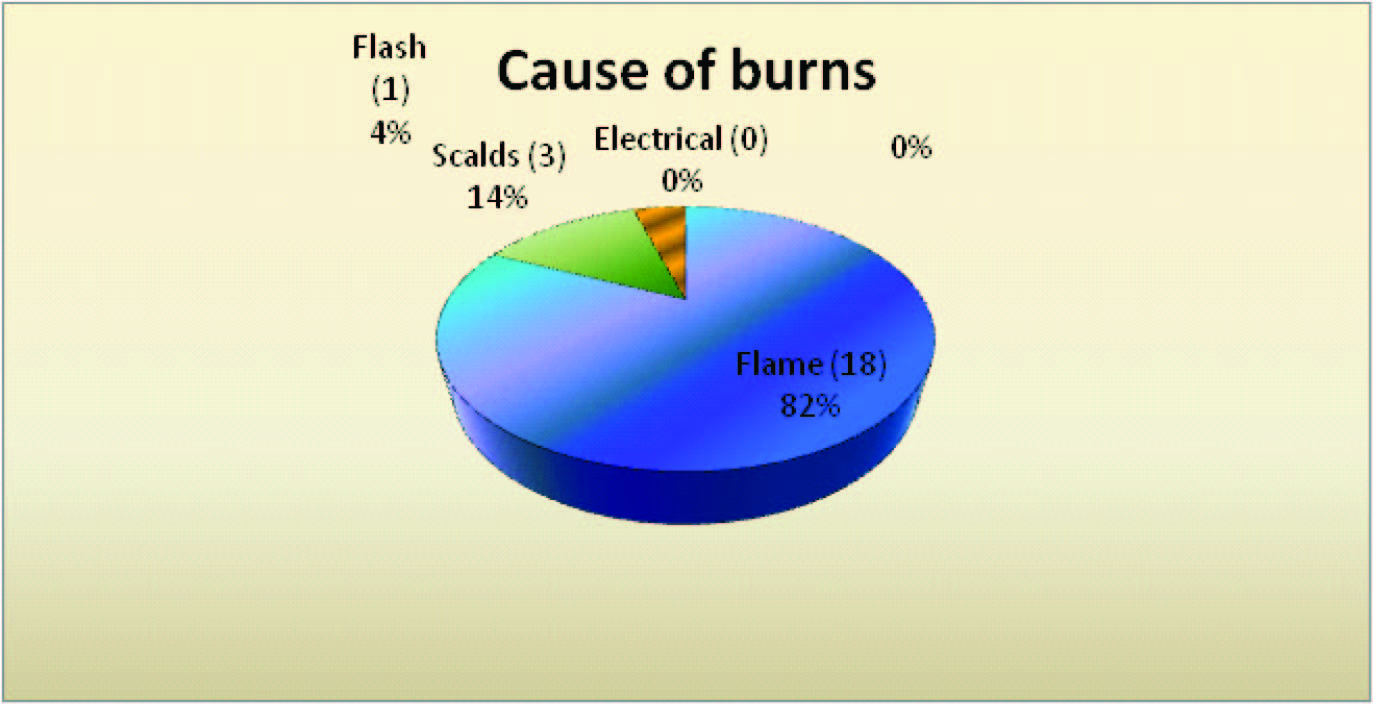
Contractures were caused by flame bums, in 81.8% of our patients [Table/Fig-13]. In Bhattacharya’s [6] series 24 patients followed flame burns and 4 contractures resulted from scalds. Ahuja [9] observed that in developing countries like India thermal burns are most frequent in contrast to uncommon chemical and electrical injuries. He adds that most of them are accidental and occur in the kitchen with floor level cooking on kerosene pressure stoves of open- hearth fires. He attributed them to malfunctioning stoves or moving about with loose flowing garments e.g. saris or dupattas, which contact the fire unknowingly. Jain [8] opines that thermal burns are very common in our country due to lack of awareness of safety measures. He adds that deep burns involving the anterior aspect of neck produce contracture because of lack of trained personnel and equipment at district hospitals and health units.
Moderate, severe and extensive contractures were present in 77.3% of patients in this study [Table/Fig-1,2,14] . M. Moustafa [7] treated 264 patients with burn contractures of the neck and 23 had multiple webs, 139 partial and 59 complete obliterations i.e. 83.7 which appear to correspond to the latter 3 groups of B.M. Achauer’s [1] classification. Mohmed Makboul et al., [10] classified his patients in 3 groups i.e. mild, moderate and severe contracture. Patients in each group were again classified in 3 subgroups i.e. linear scar, band scar and broad scar. Onah [11] introduced a classification system for PBC included major numeric categories of 1-4, which encompassed position, severity and likely problems. Tsai et al., [12], classified PBC by defining the zones of scar contractures in burn patients and the aim of this classification was to use it in microsurgical reconstruction.
Wilson [13] observed that severe contractures are more commonly seen in the developing world, a result of both the widespread use of open fires and the inadequacy of primary and secondary burn care in these countries.
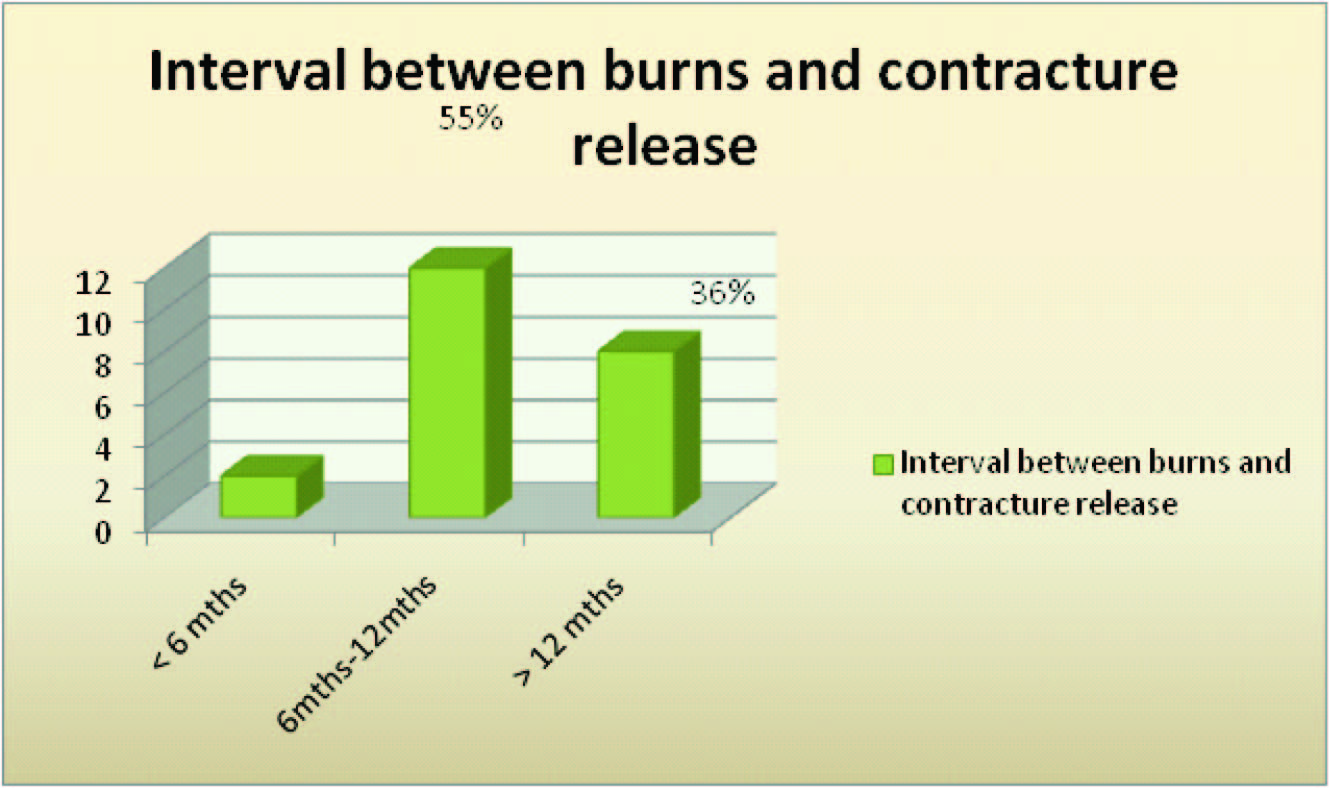
63.6% of our patients were operated within a year of burns [Table/Fig-15]. The indications for release in our study were limitation of movement (present in all our patients) besides disfigurement, malignant change, unstable scar and intolerable subjective symptoms. Patients present early for reconstruction of neck contractures because of severe functional disturbances and hence surgical procedures are often required early. C. Angrigiani [4] treated 86 patients and the interval from the initial injury to reconstruction was between 6 months and 3 years.
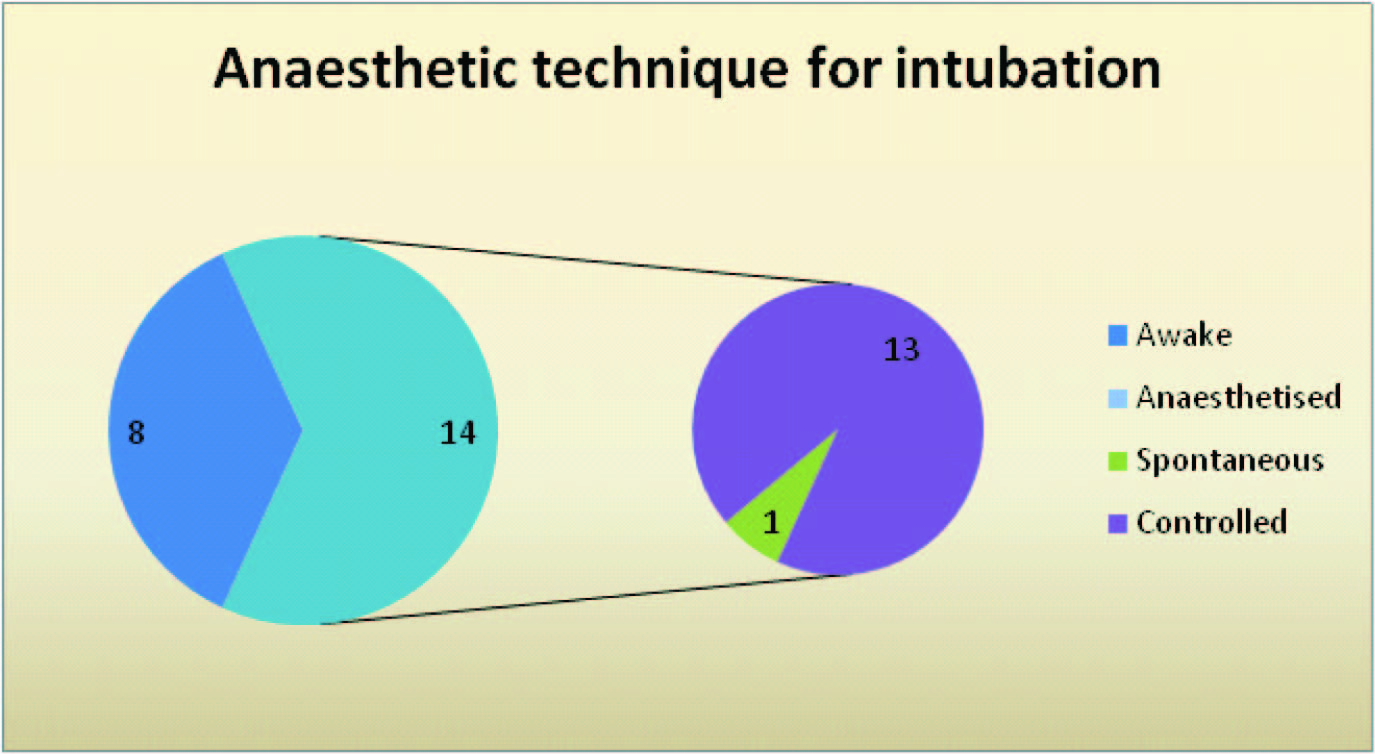
Intubation was successfully carried out in all patients in this series. In 1 case of extensive contracture, initial release was performed STSGunder ketamine and local infiltration followed by intubation [Table/Fig-16]. Alzacko et al., [14] also proposed initial release under ketamine, while Pawan Agrawal et al., [15]used tumescent local anaesthesia and ketamine. Qazi Ehsan Ali et al., [16]has used Airtraq laryngoscope for severe post burn neck contracture. In our study the contractures were probably less severe as the patients had presented at an early stage.
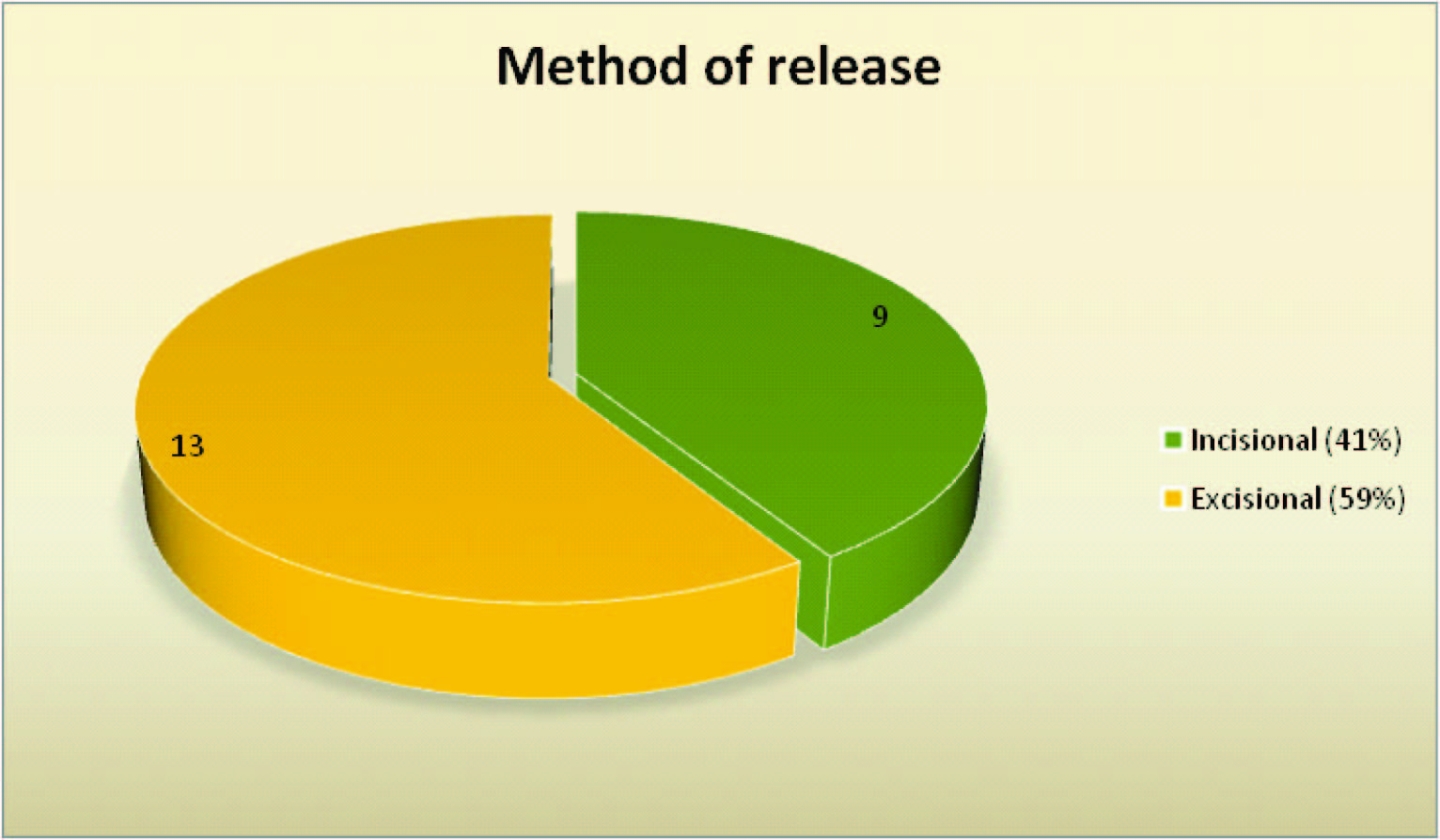
In our series, the limiting scar was excised in mild cases while incision was mainly used in severe and extensive contractures as the created defects were wide and donor sites limited [Table/Fig-7,17]. Breaking of the scar contracture and relaxation of the scarred area had a beneficial effect on the scar itself. Bhattacharya [6] excised the entire piece of scar tissue from the menton to the manubrium. Segun Aranmolate [17] tailored the excision of scars to the available bilobed flap, which he employed in 5 mentosternal contractures. Pappalardo [18] observed that there is no need to excise the scar unless it is redundant or excessively protuberant. He recommends a complete excision of unsightly scar at a later procedure after maximum function is obtained.
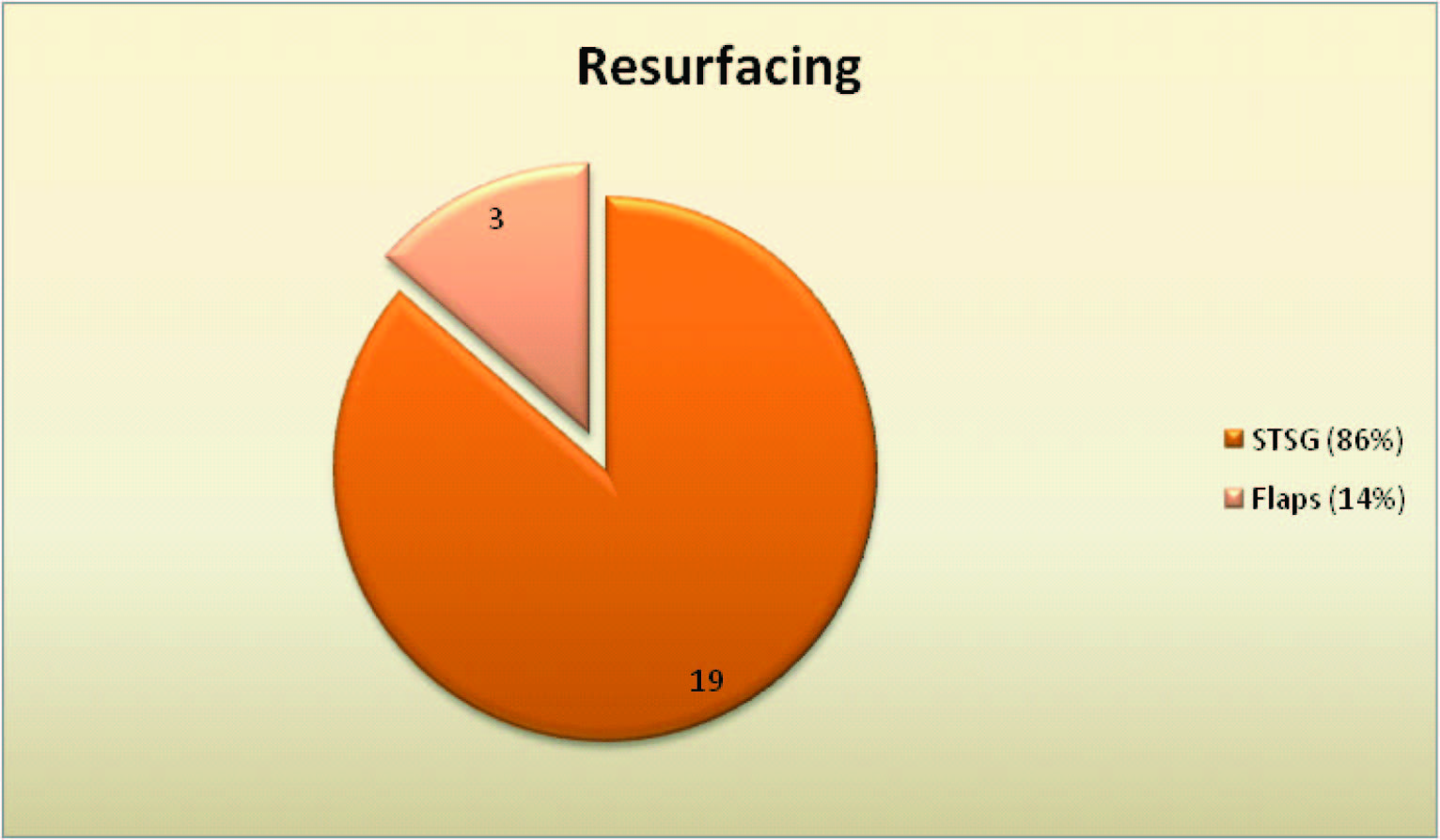
During this study, both the extensive and most of the other contractures were resurfaced with STSG and it proved to be a practical method of resurfacing [Table/Fig-18,4,5,6,8,9,23,24,25,26,27,28]. Bhattacharya [6] and Jain [8] utilized split skin grafts harvested from the thigh or leg or abdomen followed by splinting in all the patients admitted and managed by them.
Flaps were used for defect coverage in 3 patients in our study [Table/Fig-29,30,31,32,33,34,35,36]. A. Dias [19] employed the principle of bipedicled flap in the correction of 4 cases of neck contractures and skin grafted the raw areas formed above and below the transverse pedicle after release. We advanced a bipedicled flap in one patient and grafted the secondary defect in the region of the cervico-thoracic junction. There was no donor site in this flap and it stretched over time with an excellent functional and cosmetic result [Table/Fig-29,30,31].
B.G.H. Lambarty [20] used the supraclavicular flap, which he described, in a 19 years old girl who presented with severe neck contracture resulting from thermal burns. Norbert Pallua [21] modified it and used it as an island for releasing post burn mentosternal contractures in 8 patients. Laredo Ortiz C et al.,[22] used supraclavicular bilobed fasciocutaneous flap for neck contracture release. The supraclavicular artery flap was used in 1 of our cases [Table/Fig-32-34]. It can be raised in one stage without a delay and matched the colour and texture of the neck.
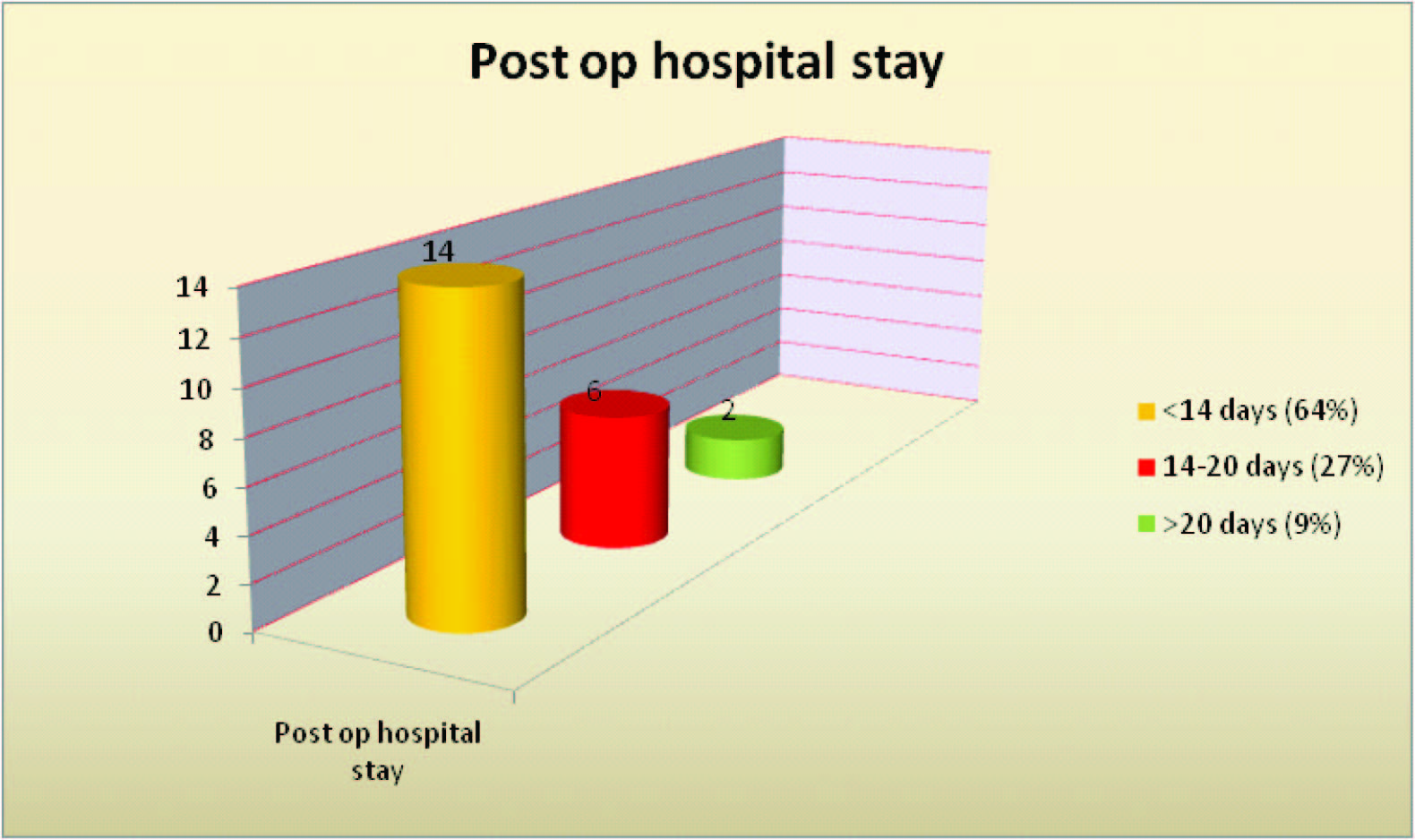
The post operative stay for our patients was around 2 weeks and a longer admission was required for patients who had to undergo repeat STSG [Table/Fig-20]. The hospital stay for Nath’s [23] patients who had been skin grafted varied from 1-3 weeks. Jain [8] discharged the patient from the hospital on an average on the 11th post operative day.
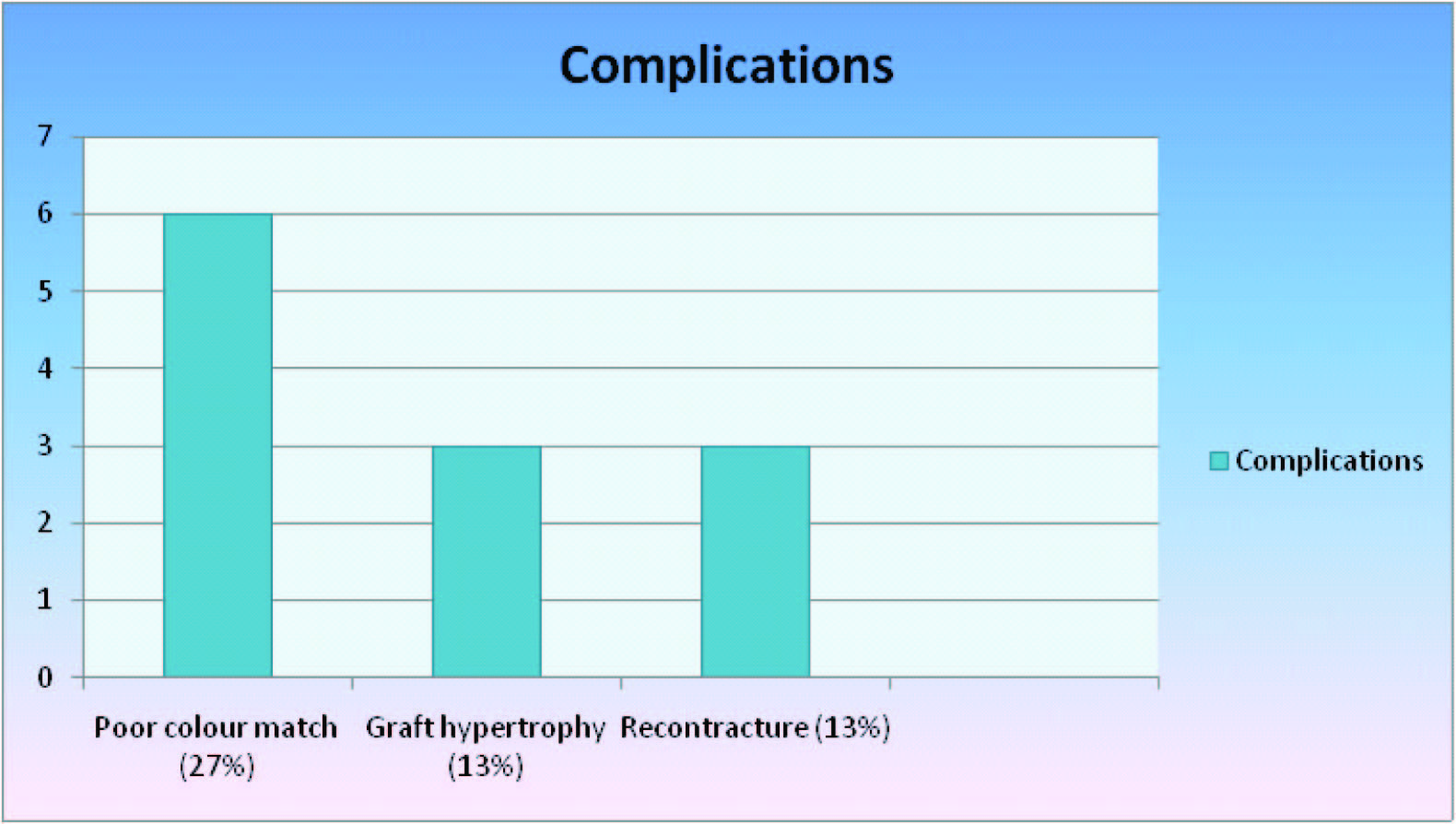
STSG which was used in the majority of cases evaluated also tends to hypertrophy and there was recontracture in 3 of our patients (13.6%) requiring release [Table/Fig-9,37]. A review by Waymach [24] of 143 neck release procedures, documented a 17% rate of contracture recurrence following releasing incisions with skin grafting and use of a neck hyperextension brace for over 1 year. Cronin [24] points out that despite the greatest care, small to large hematomas are prone to occur with loss of the skin graft if it has been applied at the time of the scar excision, as has been the protocol followed in our study. J Feldman [25] opines that it is not wise to apply the skin graft at the time of excision because of 100% ‘take’ of the graft is extremely important.
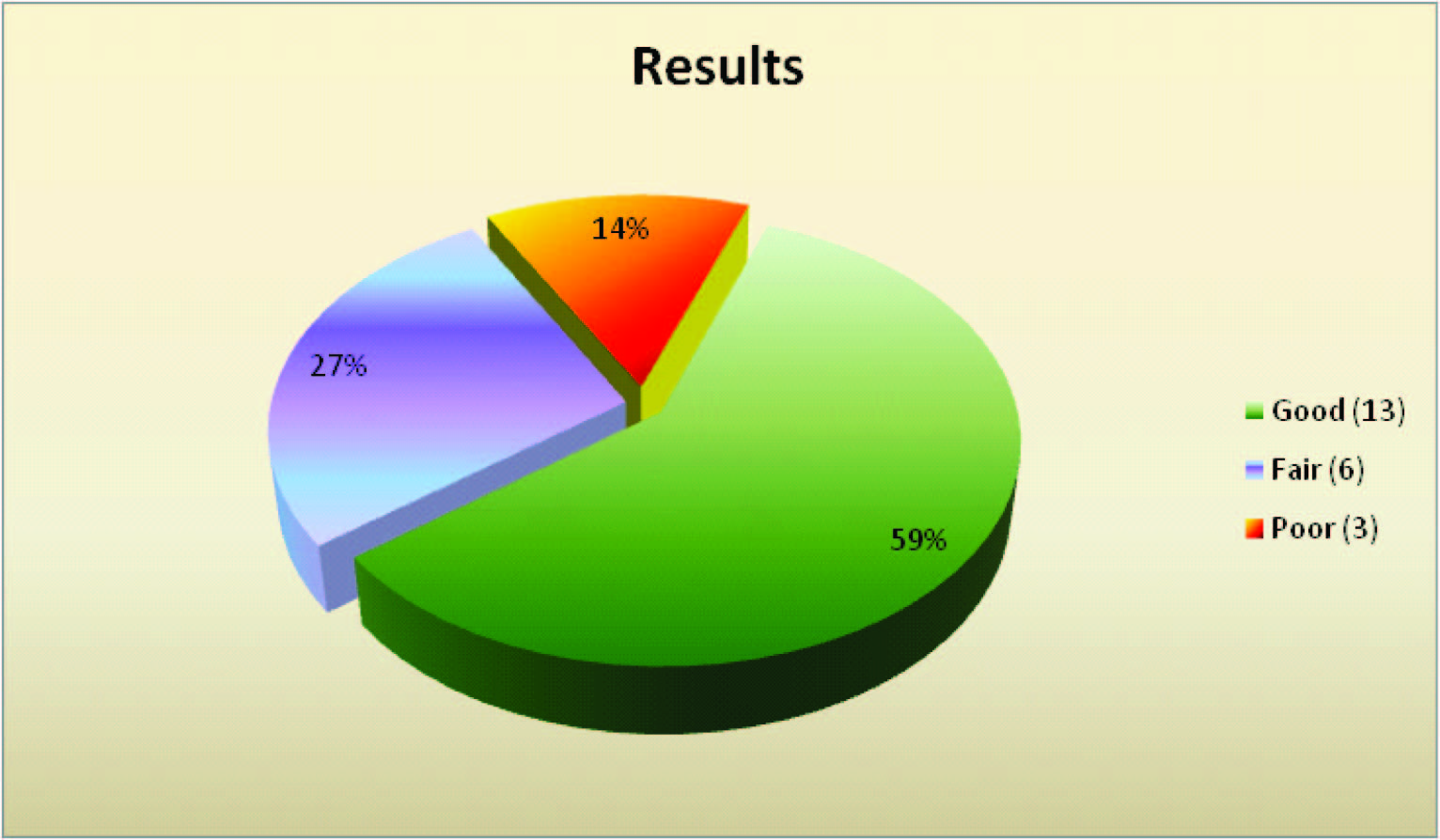
86.4% of our patients had acceptable neck function and cosmesis [Table/Fig-21]. We assessed function after rehabilitation 6 months postoperatively by the range of motion and also determined the aesthetic results by the presence of colour match and absence of hypertrophy [Table/Fig-38]. Function and cosmesis were the criteria also used by Nath [23] to determine the outcome of surgery. The former was evaluated in reference to the neck movements and the latter was defined as the appearance of the graft by its colour and texture.
B.M.Achauer’s mild and moderate contracture

B.M.Achauer’s severe and extensive contracture

Evaluation of Atlanto-occipital
Pre op neck contracture- profile view and Raw area following its release

Meshing of the graft and graft placement in the defect

op result with good mentocervical angle

Raw area following incisional and excisional release

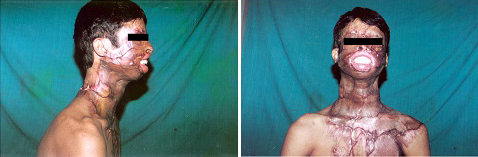
Pre op severe mentosternal contracture- Frontal and profile view

Post op result with good mentocervical angle- Frontal and profile view.,
Patient with cervical collar (Post STSG)

| Severity | No. of patients | Percentage |
| Mild | 5 | 22.7 |
| Moderate | 10 | 45.5 |
| Severe | 4 | 18.2 |
| Extensive | 3 | 13.6 |
Interval between burns and contracture release
Anaesthetic technique for intubation
Method of release of contracture
Legal knowledge based on age

Pre op moderate mentosternal contracture- profile view,

Pre op moderate mentosternal contracture

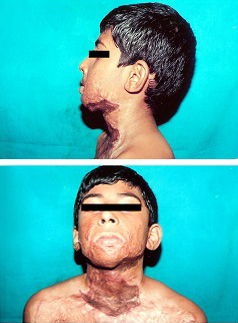
Pre op severe mentosternal contracture- Frontal and profile view

Post op result with good mentocervical angle

Pre op mild mentosternal contracture and marking for bipedicle flap

Bipedicle flap raised and flap & graft placed in defect

Post op result after bipedicle flap

Pre op mild mentosternal contracture and marking for supraclavicular flap

Supraclavicular flap raised and transposed into defect
Post op result after supraclavicular flap,

Pre op mentosternal contracture and mid arm tube flap in defect

Post op result after tube flap

Poor colour match and recontracture after STSG.,

Post op result with good colour match after STSGunder

Conclusion
Excision of all scar tissue is possible in severe contractures but incisional release is required in extensive contractures. Skin grafting is a simple, reliable and safe operation, but has disadvantage of hypertrophy and recurrence of contracture. Local and regional flaps provide a predictable reconstruction with a good colour and texture match but may not be available because of severe scarring of the surrounding tissues. While post-operative neck function is essential, the cosmetic appearance is also equally important with special attention given to the cervico-mandibular angle
[1]. BM Achauer, Neck reconstruction. In: Achauer BM, editor. Burn Reconstruction. 1991 New YorkThieme Medical Publishers:pp79-86. [Google Scholar]
[2]. R.E. Salisbury, A.G. Bevin, Atlas of Reconstructive Burn Surgery. 1981 PhiladelphiaW.B. Saunders Co:pp89-105. [Google Scholar]
[3]. J.L. Benumof, anagement of the difficult adult airway.M Anesthesiology. 1991 75:1087 [Google Scholar]
[4]. C Angrigiani, Aesthetic microsurgical reconstruction of anterior neck burn deformities.Plast. Recostr. Surg. 1993 93:507 [Google Scholar]
[5]. Mohmmed Saygin Abdul Kadir, Post burn flexion neck contracture.Tikrit medical journal. 2007 13(1):116-21. [Google Scholar]
[6]. S Bhattacharya, S.K. Bhatnagar, R Chandra, Post burn contracture of the neck – our experience with a new dynamic extension splint.Burns 1991 17:65 [Google Scholar]
[7]. M.F. Moustafa, A Borhan, A.M.A. Abdel Fattah, Burn contractures of the neck. Plast. Reconstr. Surg. 1978 62:66 [Google Scholar]
[8]. S.C. Jain, S Baliarsingh, Burn contracture neck.Postgrad Med J 1987 New Delhi, IndiaTransactions of the IXth International Congress of Plastic and Reconstructive Surgery:1-6. [Google Scholar]
[9]. Ahuja Rajeev B, Bhattacharya S, The etiology and treatment of intrinsic discolorationsBMJ 2004 329(7463):447-49. [Google Scholar]
[10]. Makboul Mohamed, El-Otteify Mahmoud, Classification of post burn contracture neck.Indian journal of burns. 2013 21(1):50-54. [Google Scholar]
[11]. Igwilo Onah Ifeanyichukwu, A classification system for post burn mentosternal contracture.Arch Surg. 2005 140:671-75. [Google Scholar]
[12]. Tsai Feng-Chou, Mardini Samir, Chen Da-Jeng, Yang Jui-Yung, Hsieh Ming-Shium, The classification and treatment algorithm for post-burn cervical contractures treated reconstructed with free flaps. 2006 32(5):626-33. [Google Scholar]
[13]. I.F. Wilson, A Lokeh, W Schubert, Latissimus dorsi myocutaneous flap reconstruction of neck and axillary burn contractures.Plast. Reconstr. Surg. 2000 105:27 [Google Scholar]
[14]. Al-Zacko S.M., Al-Kazzaz D.A., scar of neck for intubation under ketamine.Ann burns fire disaster. 2009 22(4):196-99. [Google Scholar]
[15]. Agrawal Pawan, Safe method for release of severe post burn neck contracture under tumescent local anaesthesia and ketamine.Indian journal of plastic surgery. 2004 37(1):51-54. [Google Scholar]
[16]. Ali Qazi Ehsan , Amir Syed Hussain, Siddiqui Obaid Ahmad, Jamil Shaista, Airway management in severe post burn neck contracture using Airtraq: A case series.Indian journal of anaesthesia. 2013 57(6):620-22. [Google Scholar]
[17]. S. Aranmolate, A.A. Attah, A.M.A. Abdel Fattah, Bilobed flap in the release of post burn mentosternal contracture.Reconst Surg. 1989 83:356 [Google Scholar]
[18]. C Pappalardo, The late care of burn wounds, W.W. Monafo (Ed)Postgrad Med J 1971 1st EditionSt. LouisThe Treatment of Burns – Principles and Practices Warren H. Green,:1-6. [Google Scholar]
[19]. A.D. Dias, A bipedicle flap in the correction of burn contractures.Br. J. Plast Surg 1983 36:56 [Google Scholar]
[20]. B.G.H. Lamberty, The supraclavicular axial patterned flap.Br. J. Plast. Surg. 1979 32:207 [Google Scholar]
[21]. N Pallua, HG Machens, Rennekampff The fasciocutaneous superaclavicular artery island flap for releasing post burn mentosternal contractures.Plast. Reconst. Surg. 1997 99:1878 [Google Scholar]
[22]. C Laredo Ortiz, A Valverde Carrasco, A Novo Torres, L Navarro Sempere, M Márquez Mendoza, Supraclavicular bilobed fasciocutaneous flap for postburncervical contractures. Burns 2007 33:770-75. [Google Scholar]
[23]. S Nath, K Erzingatsian, S Simonde, Management of post burn contracture of the neck.Burns 1994 20(5):438-41. [Google Scholar]
[24]. T.D. Cronin, A Barrera, Deformities of the cervical region J.G. Mc Carthy (Ed), Plastic Surgery 1990 31st EditionPhiladelphiaW.B. Saunders Co:2057-2093. [Google Scholar]
[25]. J.J. Feldman, burns Facial, J.G. McCarthy, Plastic Surgery 1990 31st EditionPhiladelphiaW.B. Saunders Co:2153-2236. [Google Scholar]